Recommended Blood Pressure Goals for Patients with Diabetes
Diabetes affects an estimated 100 million people worldwide. 5-10% suffer from type 1 (formerly known as insulin-dependent) and 90% -95% have type 2 (insulin-dependent). Heart disease (CVD) is the leading cause of death and death in people with diabetes. People, especially adults with diabetes, have a higher rate of CVD than those without. CVD as a whole affects approximately 32.2% of all people with T2DM. CVD-related complications include angina, ischemic stroke, coronary artery disease (CAD), and coronary artery disease-account for about half of all deaths in type 2 diabetes patients. Due to the clinical burden of CVD in T2DM patients there has been an increased focus on the combined management of T2DM and CVD. Therefore, the most effective way to prevent macrovascular disorders is seen as a reduction in risk factors (glycemic control, smoking cessation, diet, exercise, blood pressure control, and treatment of dyslipidemia).
Blood pressure (B.P.) in diabetic patients remains controversial. Although CVD morbidity and mortality decrease slightly with the reduction in B.P., the goal of lowering B.P. in patients with T2DM remains a challenge. The uncertainty surrounding B.P. control in T2DM complicates these patients’ care, as the risk of future cardiac events associated with the presence of diabetes is equal to people who have had myocardial infarction before. It is not yet clear why people with diabetes will not benefit from lowered SBP below <140 mm Hg (1) Control Cardiovascular Risk in Diabetes (ACCORD) reported that CBP compared with low blood pressure (target <120mm Hg) had lower rates of various adverse events associated with antihypertensive treatment.
The study reviews
The article study was a randomized trial carried out at 77 clinical settings arranged into seven networks within Canada and the United States. All identified high-risk participants were randomly assigned to pharmacological measures that fitted their conditions.
Two study groups were employed in the study. Inclusion criteria are the following:
- Participants who suffer from 2 diabetes mellitus and elicited elevated glycated hemoglobin ranging from 7.5% and above. Inclusion criteria involved:
- Those individuals who are 40 years and older were considered, and only those who suffered cardiovascular disease.
- 55-year-old individuals and older with obvious evidence of the considerable level of anatomical conditions such as atherosclerosis, left ventricular hypertrophy, albuminuria. Those who were proved to have at least two additional risk factors for CVD, such as dyslipidemia, obesity, smoking, were included in this group.
- Individuals found to have systolic blood pressure between 130-180 mm Hg, taking three or fewer antihypertensive drugs were used. Also, the individuals were required to have a proven 24-hour protein excretion rate of not more than 1g.
Exclusion criteria involved those with BMI not less than 45, those with a high serum creatinine level of not less than 1,5mg/dl, and those who suffered from other serious medical conditions apart from the stated ones.
Individuals consented through a formal written note, and recruitment occurred in two phases.
During the main trial recruitment, an upper age limit of not exceeding 79 years old was considered for individuals’ eligibility.
The study outcome was evaluated at the coordinating center.
- Tools for analysis included version 8, S-Plus software (Insightful), or version 9.1 SAS software (SAS Institute).
- Various primary characteristics of variables, considered among the participants, and essential vital feedbacks were compared between the two groups used for the study. Statistical tests, including ‘fisher’s, chi-square, Wilcoxon rank-sum, and two-sample t-test were used in drawing the identified comparisons.
- Analyses of primary and secondary outcomes were performed using time-to-event methods according to the intention-to-treat principle.
- Kaplan–Meier estimates were used to calculate the proportion of participants who had an event during follow-up.
- Hazard ratios and confidence intervals of 95% were used to compare the two groups’ secondary and primary outcomes.
- Only observed data were considered in the analysis. The missing data were assumed to be completely absent at random.
Four thousand seven hundred thirty-three participants were eligible for the ACCORD BP trial. Of these, 2362 randomly used intensive blood pressure control while 2371 used standard therapy.
Of all participants, 445 experienced CVD-related adverse events such as nonfatal stroke, myocardial infarction, or even death.
The rate of undergoing adverse effects related to pressures was 1.87% per year in individuals who used intensive therapy while 2.09% for those assigned standard therapy.
There was no significant difference noted between the two groups despite using different therapies.
Cardiovascular-related diseases caused some deaths while others died from other causes, 294 and 118. The death rate was 1.28% and 1.19, respectively.
As for deaths caused by cardiovascular causes, the two groups’ death rate was 0.52% and 0.49 for the intensive therapy group and standard group, respectively.
In terms of the stroke rate, a significant difference was noted—a rate of 0.32% and 0.53 for intensive and standard therapy groups, respectively.
Strengths
- The purpose of the study was clearly stated in the research topic.
- Participants were randomly obtained hence eliminating the aspect of the study bias.
- Eligibility criteria were comprehensive, making the study more focused and easy for analysis.
- The then clinical practice protocols approved treatment strategies employed; hence, clinical safety and improved clinical outcome were maximized.
- Autonomy, privacy, and confidentiality of participants were ensured. Consent was obtained from individuals who participated in the study. Their details are not disclosed.
- The research was grounded in previous literature on the subject. Critical analysis of previous research literature is provided in the introduction.
- The acronyms used in the study are clearly defined.
- Methodology, analysis, and discussion or research find is a comprehensive boosting understanding of the study.
- References of articles from which literature the study is grounded are provided.
Weaknesses
- Therapy was randomly assigned to the two groups. They questioned the safety of individuals who could otherwise have benefited from the other therapy not assigned to them.
- The research questions or research objectives were not outlined.
- It is not clear if the participants were protected from harm resulting from participating in the study, especially concerning health such as side effects of the therapies given.
Other Design Issues That Might Influence the Results
- Participants aged up to 79 years were involved in the study. With age, there is a degeneration of body systems. This would have affected how the body responded to given therapies, hence influencing the outcome.
- Control of chronic diseases such as diabetes and hypertension call for a multi-factorial approach, especially checking lifestyle. It is not clearly stated if the lifestyle of the individuals involved in the study was standardized.
The research had limited to a specific population- diabetic patients and specific age groups- above 40-79 years. In terms of location, the population sample was obtained in the USA and Canada. This limits the applicability of the research findings to a certain population. Therefore, the results cannot be generalized in the application.
Clinical Relevance
The findings of the research significantly contribute to the improvement of clinical practice. Since the study was founded on a rich literature review, its findings can be used as a basis for further studies. From the study, it is realized that despite the therapy T2DM patients undergo, there are still risks of suffering from CVD adverse events. Therefore, this enables care providers to handle such patients to be more cautious in ensuring the patients’ safety and quality of life.
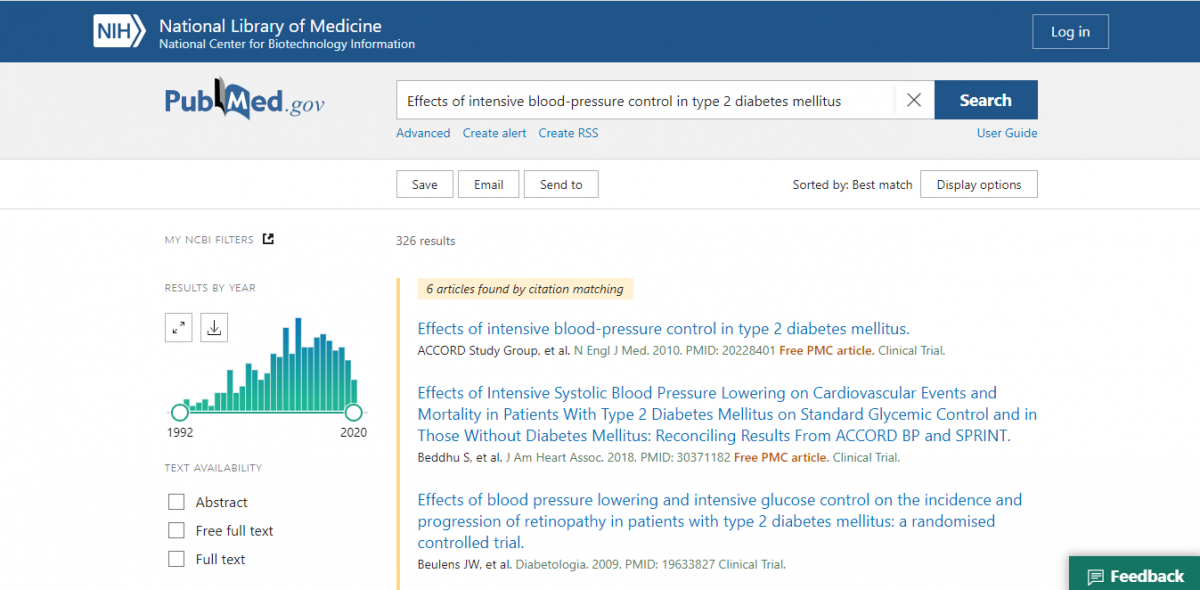
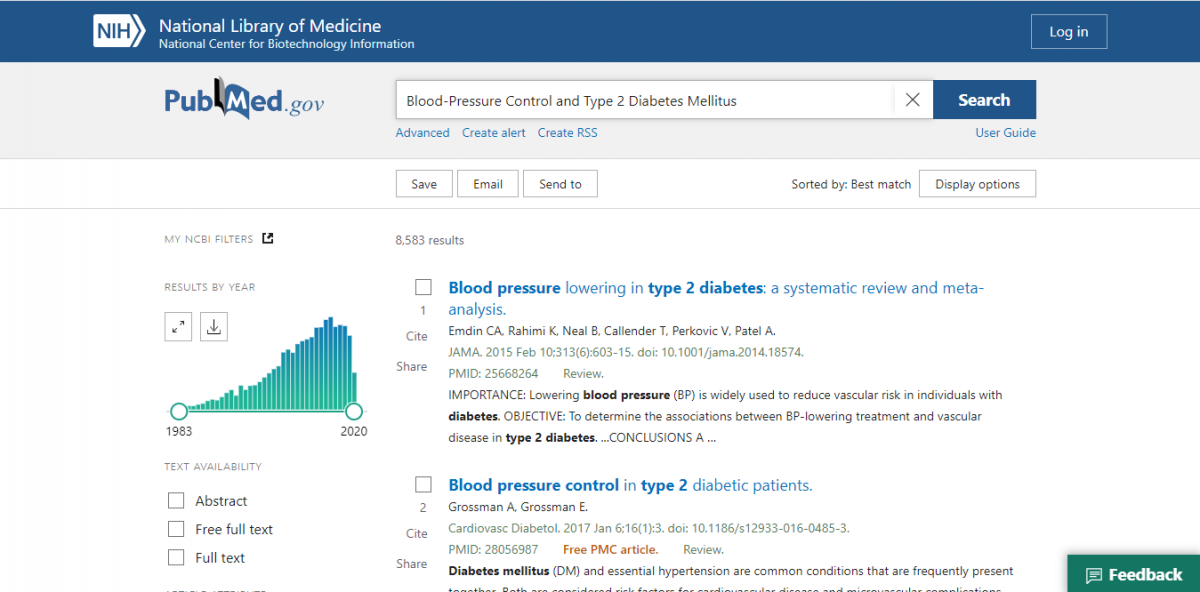
Literature Search
Keywords such as Intensive “Blood-Pressure Control” and “Type 2 Diabetes Mellitus” were used. One article identification led to another related resource. Only articles within five years were chosen; all articles were obtained from PubMed.
References
ACCORD Study Group, Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010; 362(17):1575-1585.
Beddhu S, Chertow GM, Greene T, et al. Effects of intensive systolic blood pressure lowering on cardiovascular events and mortality in patients with type 2 diabetes mellitus on standard glycemic control and those without diabetes mellitus: reconciling results from ACCORD BP and SPRINT. J Am Heart Assoc. 2018; 7 (18):e009326.
Buckley LF, Dixon DL, Wohlford GF 4th, Wijesinghe D.S., Baker WL, Van Tassell BW. Intensive 3. Versus standard blood pressure control in SPRINT-Eligible participants of ACCORD-BP [published correction appears in Diabetes Care. 2018; 41(9):2048]. Diabetes Care. 2017; 40(12):1733-1738.
Einarson, Thomas R., et al. “Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017.” Cardiovascular diabetology 17.1 (2018): 83
Espeland MA, Probstfield J, Hire D, et al. Systolic blood pressure control among individuals with type 2 diabetes: A comparative effectiveness analysis of three interventions. Am J Hypertens. 2015; 28(8):995-1009.
Rahman F, McEvoy JW, Ohkuma T, et al. Effects of blood pressure lowering on clinical outcomes according to baseline blood pressure and cardiovascular risk in patients with type 2 diabetes mellitus. Hypertension. 2019; 73(6):1291-1299.