Introduction
The quality and quantity of callus formed is dependent on Inter-fragmentary motions. The directions of these movements are dictated by the mounting plane contained in the external fixators. This study indulges in determining the role played by external fixators in the fracture healing process which is closely influenced by the mounting service. Biomechanical parameters and histomorphological aspects are important in description of the healing process of the bone. When the mounting plane is changed, there will be modification of the initial healing process due to the changing formation of the callus tissue which is very instrumental in fracture repair. Research has shown that anteromedially mounted fixators lead to more mechanical movements which lead to the formation of smaller callus tissue which is characterized by stiffness owing to its advanced healing process. The type of the fixaor therefore greatly influences the repair of fractures especially during the initial healing phase where the process is rapid (Bergmann, Graichen & Rohlmann 1999).
Biological Fracture healing
Fracture repair process takes place in three main phases namely, inflammation, reparation, and remodeling.
Inflammation
This is the initial stage which occurs upon the fracturing of the bone where blood or hermatoma clot is formed at the site where the fracture is formed. Hermatoma has two functions which are vital in the repair process of fracture. First this substance provides some level of mechanical stability to the site which is fractured. The second function which is more significant is the bringing of substantial amounts of chondrocyte and osteoblast, which will then be differentiated at the fracture area and thereafter the matrix is formed. Necrotic and the damaged tissue are removed from the fracture site courtesy of Osteoclasts and macrophages. Moreover, due to the disruptive nature of the fracture, periosteum tissue affected is supplied with more cells which will act as the precursor cells to the healing process. Osteogenesis then begins where the callus tissue is formed and the bone is laid on tissue which is soft. Endochondral ossification, osteogenesis and intra-membranous are processes which are initiated at the same time at the fracture area. These process aid in proliferation and hence the callus tissue is broken by the woven bone tissue. The consequence of the above processes is the bridging of the gap formed during the fracture (Newton & Nunamaker 1985).
Reparation
This is the phase where osteogenesis process is continuous and thus the gap caused by the fracture is reduced using the callus tissue.
Remodeling
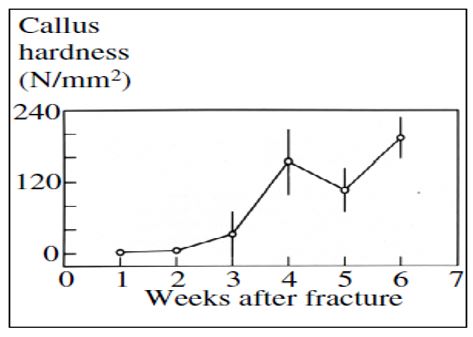
This is the last phase of the repair process when the callus formed has hardened fully and therefore the fractured part of the bone is now fully replaced by the newly formed bone tissue. Either endochondral or intra-membranous ossification process or both are important in yielding new bones. The mechanical stimuli, is very important at this level since it has the greatest impact on the healing process. The main reason for this is that it increases mechanical stability of the fractured site which is vital for the repair process. This fixation devices will help to reduce motion as much as possible to ensure that the fracture is repaired fully otherwise non-union might result in situations where soft tissue replaces the fracture instead of the bone itself. This has called for the deployment of different types of fixators depending on the area of fracture so as to appropriately stimulate the healing process (McCoy, Briggs & Chao 1980).
The resultant of the all process is made of both the primary bone and the woven bone which is in the form of a large bony bridge to connect between two primary bones. The base material which forms the callus is very strong in nature than the original mature lamellar bone. Owing to this the lamellar bone should be remodeled to remove the excess callus mass. During this process, the mechanical integrity of the bone functioning should be upheld. The remodeling process therefore ensures that the size of the new bone has been reduced to the size of the original bone of the fracture site. This process of replacing the original bone with a secondary lamellar bone might take several months or even years (Buckwalter, Einhorn & Marsh 2001).
Fracture Repair Optimal conditions
Stress which is compressive in nature helps in shielding and sharing the load which is subjected to the fractured bone. There is need for micro-motion of the fractured segment so that there is no rigid fixation or gross movement. Further there should be adequate supply of blood to the fractured area to facilitate revascularization process (Fung 1981).
Biomechanics of Fracture Healing
Postfixation is the most influential biomechanical factor during the healing process of a fracture. The healing process of a fracture is greatly dependant on the mechanical factors which are present in or within the vicinity of the fracture. Orthopaedists are charged with the responsibility of reconstruction of a normal anatomy from a bone which has been fractured and provision of minimal allowable stability required for the process of healing.
The processes ensures that motion is reduced since this is the determinant for the survival of the tissue found between the fracture terminals and eventually determine the resultant jointing whether it will be primary, non-union or secondary. The angular and normal motions involved should be considered therefore before fixing an external fixator. The cartilage, bone and granulation tissue dictates the amount of stress and strain that the fracture can withstand (Bucholz & Heckman 2001).
Mechanical Concepts
Fracture etiology and the modalities of fracture repair are better understood by analyzing the bone biomechanics when they are functioning normally at their health condition.
Mechanical concepts that are related to the materials used in bone repair are relevant in this process. It is therefore important to discuss the concepts that are common to both the clinical expert and the engineers who join hands to ensure that this process of fracture healing is a success.
Bones are solid in nature and they are subjected to forces as well as deformations during their normal functioning. The contextual use of load and force is to mean the magnitude vector which is always deforming the structure or the whole of the bone. In this case stress can be defined as the amount of force applied per unit cross-sectional area of the bone which is supporting the force. The two terms force and stress are not the same but they are related.
Strength and stiffness are other two important engineering aspects as much as engineering is concerned. The term strength has two main methodologies of measuring; structural strength is the strength of the bone due to the structural facets such as the difference in cross sectional area where as material strength is the difference of strengths of different bones of the same structural features (Allen et al. 1968).
Effects of External fixing devices on the bone repair process
Tension Band Principle
The external devices fixed on fractures are in many cases placed on the side of the fracture which is always under tensile stress during its normal operation. The devices are exposed to stress prior to the fixing process and therefore there is residual tensile stress that will be subjected to the bone under treatment. The main reason for doing all this is to ensure that the bone is always under compressive stress and loads across the entire bone cross sectional area. A good example is shown in figure 2 (Hayes 1980).
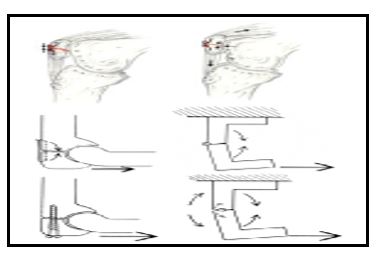
Tension banding can be used as a principle for repair process of the olecron or patellar which contain cerlage wiring. The use of plates as external devices for fracture repair acts as tension bands which help in enhancing the repair process. The use of screws is not appropriate for these types of fractures (Hayes & Perren 1972).
There are two types of fixators which are employed depending on the type of the fracture; full frame, and half frame. The nature of the external device used also has an impact on the healing process of the fracture. Research shows that the rigidity of the bones that result from osteogenesis of fractures related to oblique and transverse structures is higher. From clinical point of view the researchers concluded that the use of half frame was unsatisfactory however it found out that under optimal conditions, the results can be improved. The modifications that can be done for the half frame external fixators for optimum performance include minimizing the side bar lengths which connect the fracture area, the clamps used should be fixed as close to the bone as possible and the number of pins used should be increased to three from the normal two pins which are maximally fixed in each fragment. The half frame under the optimal conditions makes the fixator to behave as an elastic rather than rigid support. This property therefore allows minimal motion facilitating fracture healing through the formation of periosteal callus (Evans 1979).
On the other hand the full-frame external fixator employs through to through pins. The resultant from this external device is more stability and therefore has been used for a long time in the clinical sector. The transition from flexible to rigid nature of the fixator is achieved through the design of the pin sizes. The symmetric nature of these fixators allows them to be applied in producing distraction forces to the fracture area (Hipp & Hayes 2003).
Conclusion
In conclusion external devices fixed to facilitate the healing process of the fracture are very important. The main reason for using external immobilization is to increase the stability of the internal structures of fracture area particularly when the device is rigid. The process leads to the sandwiching of the soft tissue between the splint and the bone which are characteristically rigid. The stability of the fracture which is achieved by using, external fixator is not as rigid as when internal fixators are used but this is controlled by the tolerance to stress and compressibility of the tissue which is interposed (Paul 1965).
The immediate post fixation of the fracture is very effective when they are applied to a fractured area but it is not comparable to the stability which results from transfixation or internal fixation.
When the external fixation is applied, particularly the one which is compatible to the biological process specific to the repair process then secondary bony union occurs. External devices therefore increase the rate of healing when they are used appropriately and in good time.
References
Allen, et al., 1968. Biomechanical Principles of Intramedullary Fixation. Clin Orthop Rel Res, 60(5), pp.13-20.
Bergmann,G., Graichen, F. & Rohlmann, A., 1999. Implantable Telemetry in Orthopaedics. Berlin: Freie Universitat Berlin.
Bucholz, R.W. & Heckman, J.D., 2001. Rockwood and Green’s fractures in adults. Philadelphia: Lippincott Williams & Wilkins.
Buckwalter, J.A., Einhorn, T.A. & Marsh, J.L. 2001, Bone and joint healing. Philadelphia: Lippincott Williams.
Evans, M., 1979. The Oxford external fixateur. Oxford, England: The 6th Annual Report of the Oxford Orthopaedic Engineering Centre.
Fung, Y.C., 1981. Biomechanics: Mechanical Properties of Living Tissue. New York: Springer-Verlag.
Hayes, W.C., Perren, S.M., 1972. Plate-bone fixation in the compression fixation of fractures. Clin Orthop Rel Res, 89(16), pp.236-240.
Hayes, W.C., 1980. Biomechanics of fracture treatment. Philadelphia: WB Saunders.
Hipp, J.A. & Hayes, W.C., 2003. Biomechanics of fractures. Philadelphia: WB Saunders.
McCoy, M.T., Briggs, B.T., Chao, E.Y.S., 1980. A comparative study of external factors based on bone fracture stiffness. Atlanta: Proceedings of the 26th Orthopaedic Research Society.
Newton, C.D. & Nunamaker, D.M., 1985. Small Animal Orthopaedics. New York: International Veterinary Information Service Ithaca.
Paul, J.P., 1965. Bioengineering studies of the forces transmitted by joints. London: Pergamon Press.