Abstract
“Black and Healthy” is a nongovernmental organization that was started in 2001. The main focus of the organization is to reduce the burden of sexually transmitted diseases (STDs) in the United States. Since its inception, the organization has been facilitating this kind of programs in the US (In Texas and Illinois). In the 1990s, the transmission of primary and secondary syphilis had been adequately contained but from the beginning of the new millennium, it began to rise again. Since then, the State of California has had the highest number of P&S syphilis cases. This research paper reviews past literature to analyze how syphilis in the US has plagued African American women and what should be done to reduce the sustained domestic transmission of the disease. Four interventions will be used to deal with the challenge. These are screening for syphilis infection, behavioral counseling, youth development and behavioral interventions and comprehensive risk reduction. The program that is suggested in this study will be implemented within a period of five years. The main aim of the plan is to reduce sustained domestic transmission of primary and secondary syphilis among African American females between the ages of 18 and 24 by 60 percent. Throughout the course of implementation, the allocation of resources will be altered according to the changing needs of the target population.
Reduced Sustained Domestic Transmission of Primary and Secondary Syphilis among Females: Planning Healthy People 2020
Introduction
The Center for Disease Control launched a program to eliminate the transmission of syphilis in 1991. Back in the 1990s, the rate of syphilis infection in the United States was very low and the diagnosis and therapy were inexpensive. However, the rate of infection in the nation began to increase from 2000 especially among African American women. This and other related factors led to the revision of the plan in 2006 to determine what was needed for the initiative to succeed (Jefferson County, 2009). The purpose of this paper is to outline how Black and Healthy will implement a 4-intervention program to reduce sustained domestic transmission of primary and secondary syphilis among African American females between the ages of 18 and 24 by 60 percent.
Literature Review
Syphilis among African American Men and Women
Syphilis has disproportionately impacted on men and women of African American descent in the US. This is in spite of the fact that they only consist of 13% of the nation’s total population (Mojola & Everett, 2012). Reports have shown that close to 58 percent of all the primary and secondary (P&S) cases of syphilis in the US occur among African Americans.
In spite of the fact that African American women constitute only about 12% of the American population, studies show that their rate of sustained domestic transmission of primary and secondary syphilis is very high when compared to that of other races (Sutton et al., 2009). For instance, data from CDC shows that in 2010, sustained domestic transmission of primary and secondary syphilis among female African Whites was twenty times that of their Caucasian counterparts. At the same time, the rate of congenital syphilis among infants of African Americans was fourteen times that of Caucasian infants (Baffi et al., 2010).
Moreover, the rate of primary and secondary syphilis among African American men aged between 15 and 24 years was on the rise between 2005 and 2009. This is as shown in Table 1 below:
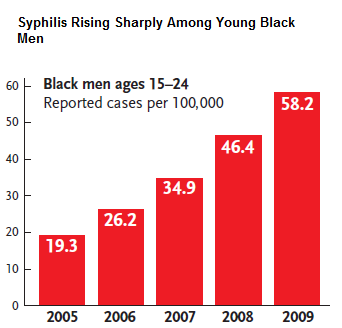
Within the same period, 63 percent of all the P&S syphilis cases among African American males occurred among those who have sex with other men. Consequently, the CDC proposed that men who have sex with other men (MSM) should be tested for syphilis at least once every year. This is very essential because extensive research has continued to draw correlations between syphilis and increased HIV infections (Helion et al., 2008).
Syphilis Complexities among Young African American Women
Baffi et al. (2010) are of the opinion that the combination of psychosocial determinants and behavioral factors increase the vulnerability of African American women to syphilis infection. In order to reduce sustained domestic transmission of primary and secondary syphilis among African American females, it is essential to take these issues into consideration. Figure 2 below shows a syndemic model of the factors that have contributed to the increased syphilis burden among African American women in the US. These include low literacy levels, unintended teen pregnancy (UTP), increased risks to STD and HIV.
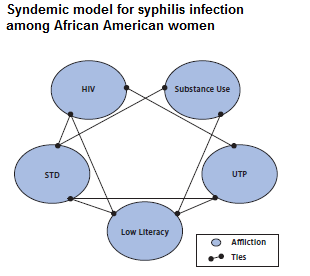
Surveillance data and epidemiological studies have shown that female African Americans must be taken into consideration when implementing P&S syphilis elimination initiatives. The organizations that are involved in the formulation and implementation of programs that are aimed at reducing P&S syphilis among young African American women have to come to terms with the syphilis infection complexities. This would go a long way towards addressing the cultural and social issues that put these women in this situation. Additionally, these women should have easy access to facilities that offer treatment for substance abuse, HIV, mental disorders and others that stem from sexual abuse (Chesson et al., 2011).
African American Women’s Relationship Dynamic
Endyke-Doran et al. (2007) are of the view that African American women in the US have the least likelihood of getting married. For example, a 2002 study found that 42% of female African Americans were unmarried. There is gender imbalance between the males and females of African American descent which has resulted in fewer partners available for the ladies. Because of such realities, the interpersonal power of women in relationships is minimal because men have more options.
Endyke-Doran et al. (2007) add that African Americans have the highest probability of being in overlapping (concurrent) relationships. This has resulted in increased rates of syphilis infection. This high rate of ‘concurrence’ has been attributed by some researchers to the low rate of marriages. The imbalance has also made it more difficult for these women to discuss and negotiate for the use of condoms with their male partners. It has been found that intimate relationships (without threats and conflicts) and sexual communication highly determine the effectiveness of condom as an STI and STD prevention tool.
Interventions
Screening for Syphilis Infection
Mojola & Everett (2012) posit that medical practitioners should screen persons who are at a high risk of being infected by syphilis. African American females aged between 18 and 24 years fall under this category of persons. Although there is no empirical evidence to show that screening for syphilis infection enhances health outcomes among those who are at a high risk, it has been evidenced that screening for the disease accurately detects the organism and that when antibiotics are appropriately administered, the patient is cured.
Heffelfinger, Swint, Berman & Weinstock (2007) point out that a study conducted between 1994 and 2004 did not come up with direct evidence that screening for syphilis reduces mortality or morbidity. Generally, there is need to screen female American African patients for syphilis. However, the screening process has various demerits. Nonetheless, various studies have recommended the screening of African American women for syphilis.
Behavioral Counseling
In addition to screening, African American women should have access to the relevant behavioral counseling services to reduce sustained domestic transmission of primary and secondary syphilis. In spite of advanced screening, diagnosing, and treating of syphilis and other STIs, these illnesses still remain the major cause of mortality and morbidity in the nation. Medical practitioners have the capacity to identify young women whose behavior predisposes them to syphilis (Sutton et al., 2009). There is evidence showing the effectiveness of behavioral counseling when addressing STIs among young people. There are no biological or behavioral side effects associated with behavioral counseling for risk reduction.
All young African American women (aged between 18 and 24 years) and who are at a high risk of contracting syphilis should be offered behavioral counseling. This should also include married adolescents who can be regarded as adults. Advance practice nurses and other professionals in the health fraternity should take into consideration the characteristics of the population within which they intend to offer counseling. This includes conducting a research to determine the STI rate in the population. In case of a high rate of infection, all adults who are sexually active and involved in sexual relations with more than one partner should be regarded as being at an increased risk (Sutton et al., 2009).
The most effective form of counseling intervention is delivered using multiple group sessions over a period of between 3 and 9 hours. Most of the research available suggests that single counseling sessions that last for less than an hour are quite ineffective in reducing STI incidences. Adults who are at a lower risk of being infected with STIs have a corresponding lower incidence. The benefits of counseling for such a population may be minimal as compared to the one for those who are at a higher risk. This is for example the group addressed in this paper (Sutton et al., 2009).
Cohen et al. (2012) are of the view that high intensity counseling on sexual behavior can be done in any sector of the health care system, but mainly in primary care. Moreover, counseling for risk reduction can also be offered by other organizations in the community. Collaboration between primary care providers and the community improves the effectiveness of high intensity behavioral counseling. One study that involved six trials to determine the effectiveness of behavioral counseling among young African American women found that in six months, the number of confirmed STI cases among the target population had reduced significantly (Williams et al., 2009).
In this particular study, the rate of reduction in the trials ranged between 3% and 11% with the highest reduction recorded among teenagers. One of the studies also found that when a person is offered two 20 minutes-long counseling sessions after being tested for HIV, this reduced the rate of STIs (gonorrhea, chlamydia, HIV and syphilis) infection (Williams et al., 2009).
Comprehensive Risk Reduction
Comprehensive risk reduction is effective in addressing prevalence of STIs. Some of these interventions are listed below:
- Promoting reduction of sexual risk and abstinence while placing emphasis on any of them.
- Promoting reduction of sexual risk, solely or primarily.
Such interventions can be executed in the community and in schools for female African Americans aged between 18 and 24.
This paper suggests the use of CRR because of the empirical evidence showing its effectiveness. This includes:
- Reducing risky behaviors that are reported by young people such as engaging in premarital sex, the number of times they have sex, number of people they have sex with, and the number of times they have sex without protection.
- Increasing the use of protection against STIs.
- Reducing the number of clinically-documented and self-reported STIs.
However, it is important to note that this is an intervention that can be targeted at boys only, girls only or boys and girls together. It can be delivered in groups both in the community and in school. It can be led by peer educators or other adults and can be tailored to individuals or groups and implemented as multicomponent or single programs (Helion et al., 2012).
One study that was conducted in fifty different regions in the US found that CRR was favorable and had statistical significance in reducing sexual activity, number of times the subjects had sex, number of people they had sex with and number of times they had sex without protection. This is together with a decrease in the number of STIs and increased use of condoms and contraceptives. However, the study found that although CRR had a favorable impact on the use of oral contraceptives and reduction in rate of pregnancies, the findings did not have statistical significance. The results also indicated that CRR can be used as an effective intervention against STIs by all major races in America. This is in community and school settings by persons aged between 14 and 24 years (Helion et al., 2012).
Youth Development and Behavioral Interventions
These are programs that endeavor to positively and holistically influence the wellbeing and health of the youth (Cohen et al., 2012). Such initiatives can be aimed at reducing the incidence of STIs or may include other broader initiatives. The emphasis of these interventions is on:
- Cognitive, emotional and social competence training that aims to promote norms that enhance societal productivity and wellbeing.
- Better decision making
- Better communication skills
- Self-determination
- Positive and productive bonding between young people including role models who are not parents.
The group that is addressed in this study can be involved in various community services in diverse community settings like homeless shelters, hospitals, and nursing homes (Lautenschlager, 2006). Such community services would make it possible for young female African Americans to interact with other people leading to sexually responsible lives. They would have the opportunity of being part and parcel of a community that has explicit responsibilities and rules and one that derives fulfillment in enhancing the lives of others (Chesson et al., 2011).
Studies have outlined that the young people who engage in community development services are less likely to participate in risky sexual behaviors. One particular research involved 9 studies that were conducted in 9 different American cities (Chesson et al., 2011). These studies targeted young people between 16 and 23 years. Six of them reported a 50 percent reduction in pregnancy rate. 3 studies reported a reduction in the number of times that the young people were engaging in sexual activity. In 3 studies, the use of condoms and other birth control methods was inconsistent but all the studies recorded a decrease in the number of STI cases (Katz et al., 2008).
Implementation Plan
Various regions in California will have their own program managers who will be responsible for the implementation of the “Black and Healthy” action plan. During the course of the program, the local offices will keep in touch with the central office. The local program managers will submit monthly progress reports on the implementation to the central office. The main office will be charged with the responsibility of identifying additional resources that will be needed for the program. In the event that new needs (that had not been identified in the plan) arise, the local offices will duly inform the central office which will determine whether or not to change the initial plan.
All the four interventions will be rolled out at the same time. This is from January 5th 2013. Before the roll out, the team representatives will visit all collaborating organizations in California. These include schools, nursing homes, hospitals, nongovernmental organizations, state and federal government offices. The team will conduct a reconnaissance visit to the target population five months before the beginning of the program. During the visit, the target group will be provided with the details of the program.
Each year, the program will be implemented in two phases of six months. After the first six months, a study will be conducted to establish the effectiveness of each intervention. After the study, the central office will allocate resources depending on the outcomes of the interventions.
Expected Outcomes
The expected outcomes can be divided into short term, medium term, long term and collateral benefits:
- Short term: In the short term (the first year), it is expected that P&S case identification among the target group will increase as the four interventions are rolled out.
- Medium term: After two years, it is expected that the incidence of sustained domestic transmission of P&S syphilis will have reduced as follow-up continues.
- Long term: After the five years of the program, it is expected that the incidence of P&S syphilis will reduce by at least 60 percent.
- Long term: After the five years, it is expected that local communities will have adequate capacity to sustain the low incidence of the disease and finally eliminate it.
- Collateral benefit: The level of public awareness will increase and the disease will be easily diagnosed at the primary stage.
Outcome Measures
In the course of the program, one of the members will be submitting reports to the coordinator on the activities of the team. The coordinator will then submit the same to the program manager. The reports will contain information on performance and process evaluation indicators. These indicators will include:
- A summary of the cases, including risk factors, geographic distribution, and demographics.
- A summary of the control measures that were implemented.
- Analysis of successes, failures and reasons for failures.
- A plan on how the team can enhance monitoring in areas that are severely affected.
- An outline of the additional resources that are needed to reduce sustained domestic transmission of primary and secondary syphilis among the subjects in focus.
Afterwards, the program manager will send the compiled reports to the central office. The staff at the central office will then make necessary adjustments depending on the conclusions.
Evaluation of Outcomes
The plan will be continuously evaluated throughout the five years of implementation. Nonetheless, the local offices will submit written evaluations of the four interventions that will contain details of any new activities that should be included in the program. This report will be reviewed by the coordinator and program manager and will be forwarded to the central office later. The leadership at the central office will discuss the progress of the program and propose any changes on the plan. This report will also contain the aforementioned evaluation indicators.
Budget Justification
In 2007, CDC presented a report to Congress and pointed out that it would require at least 4 million dollars every year for a period of three years to fund a similar program that would reduce the incidence of P&S syphilis among MSMs in California by half (Jefferson County, 2009). It is not possible to come up with an exact figure of the monetary resources that are required in this exercise because of variables like infrastructural delays in the cities and epidemics of crack cocaine. Moreover, prevention programs for syphilis in some parts of California have been underfunded in the past. This has led to wide gaps in the provision of services, persistent transmission of syphilis and poor surveillance. In order to adequately implement this plan, the team will solicit funding from the state and the federal governments. It is quite clear that an annual budget of less than $4 million will not be enough to address the needs that are identified in this paper. Figure 3 below outlines the resources that the team will require from the government in order to meet its objectives. Usually, the local and state governments contribute about 35% of the amount required for STDs prevention initiatives while the remaining part is provided for by the Federal government.
Budget
Figure 3 below presents a tentative budget outlining how the government can allocate funds to meet this objective:
Figure 3. Resources Required (Million Dollars) for Eliminating Sustained Domestic Transmission of P&S Syphilis (2013-2017).
Conclusion
Female African Americans are at a high risk of being infected with syphilis. This is especially the case in California which is reported to have the highest prevalence rate and incidence of P&S syphilis in the US. In spite of the advances that have been made in the diagnosis and treatment of the disease, young African American women have been diversely and disproportionately affected by the burden of syphilis. There are multiple factors that contribute to this increased risk. In order to reduce sustained domestic transmission of primary and secondary syphilis, Black and Healthy takes into consideration the contributing factors and relationship dynamics among the members of the group. It will thus implement a 4-intervention program to reduce sustained domestic transmission of P&S syphilis by 60 percent.
References
Baffi, C. W., Aban, I., Willig, J. H., Agrawal, M., Mugavero, M. J., & Bachmann, L. H. (2010). New syphilis cases and concurrent STI screening in a Southeastern U.S. HIV clinic: A call to action. AIDS Patient Care & STDs, 24(1), 23-29. Web.
Chesson, H. W., Pinkerton, S. D., Voigt, R., & Counts, G. W. (2011). HIV infections and associated costs attributable to syphilis coinfection among African Americans. American Journal of Public Health, 93(6), 943-948.
Cohen, S. E., Chew, R. A., Katz, K. A., Bernstein, K. T., Samuel, M. C., Kerndt, P. R., & Bolan, G. (2012). Repeat syphilis among men who have sex with men in California, 2002-2006: Implications for syphilis elimination efforts. American Journal of Public Health, 102(1), e1-e8. Web.
Endyke-Doran, C., Gonzalez, R., Trujillo, M., Solera, A., Vigilance, P. N., Edwards, L. A., & Groves, S. L. (2007). The syphilis elimination project: Targeting the Hispanic community of Baltimore City. Public Health Nursing, 24(1), 40-47. Web.
Heffelfinger, J. D., Swint, E. B., Berman, S. M., & Weinstock, H. S. (2007). Trends in primary and secondary syphilis among men who have sex with men in the United States. American Journal of Public Health, 97(6), 1076-1083. Web.
Helion, A. M., Reddy, D. M., Kies, A. L., Morris, D. R., & Wilson, C. M. (2008). Influence of communicator’s race on efficacy of an HIV/STD prevention intervention among African American and Caucasian college students. Public Health Nursing, 25(5), 440-450. Web.
Jefferson County (2009). Primary and secondary syphilis 2002-2007. MMWR: Morbidity & Mortality Weekly Report, 58(17), 463-467.
Katz, R. V., Kegeles, S., Kressin, N. R., Green, B., James, S. A., Wang, M., & Claudio, C. (2008). Awareness of the Tuskegee syphilis study and the US Presidential apology and their influence on minority participation in biomedical research. American Journal of Public Health, 98(6), 1137-1142.
Lautenschlager, S. (2006). Cutaneous manifestations of syphilis: Recognition and management. American Journal of Clinical Dermatology, 7(5), 291-304.
Mojola, S. A., & Everett, B. (2012). STD and HIV risk factors among U.S. young adults: Variations by gender, race, ethnicity and sexual orientation. Perspectives on Sexual & Reproductive Health, 44(2), 125-133. Web.
Sutton, M. Y., Jones, R. L., Wolitski, R. J., Cleveland, J. C., Dean, H. D., & Fenton, K. A. (2009). A review of the Centers for Disease Control and Prevention’s response to the HIV/AIDS crisis among blacks in the United States, 1981–2009. American Journal of Public Health, 99(S2), S351-S359.
Williams, L. A., Klausner, J. D., Whittington, W. H., Handsfield, H., Celum, C., & Holmes, K. K. (2009). Elimination and reintroduction of primary and secondary syphilis. American Journal of Public Health, 89(7), 1093-1097.