Background
Patient safety is typically viewed as the number one priority in nursing, aside from the focus on patients’ recovery. Therefore, addressing the factors that define the degree of threat to which patients are exposed in the clinical setting is especially important to discuss. Among the essential factors upon which the well-being of patients hinges, nurse satisfaction takes a crucial spot since the extent of stress and fatigue that a nurse experiences due to a vast amount of workload determines the nurse’s ability to meet a patient’s needs adequately. Studies show that the percentage of burnouts and instances of fatigue in the workplace setting defines the percentage of medical errors made while addressing patients’ needs (Woodhead, Northrop, & Edelstein, 2016). Therefore, locating the strategies that will help to reduce the range of stress that nurses face is critical for keeping the quality of care at the proper level.
Problem Statement
Due to the increasingly high levels of nurse shortage and the subsequent increase in workload, as well as the lack of appropriate stress reduction techniques, the rise in workload leads to an increase in workplace errors and poor quality of nursing services. As a result, both nurses and patients suffer greatly, the latter taking more time to recover, while the former develop mental health issues that run the gamut of anxiety and depression disorders (Johnson, Butler, Harootunian, Wilson, & Linan, 2016; Sagherian, Clinton, Abu-Saad Huijer, & Geiger-Brown, 2017). Therefore, creating and testing a strategy that could help alleviate the devastating experiences of nurses in the hospital setting is an absolute necessity. For this purpose, an innovative program for handling workplace difficulties such as time management issues and conflicts in the workplace will be required (Akbar, Elahi, Mohammadi, & Khoshknab, 2016; Hevezi, 2016). For this purpose, the BREATHE: Stress Management for Nurses program was selected (Hersh et al., 2016). Accessible as a digital framework, the proposed approach will lead to better management of the nurse shortage problem and the related concerns.
Purpose of the Change Proposal
The goal of this proposal is to evaluate the effects of the BREATHE program as the method of handling the current issue of nurse shortage caused by workplace burnouts and lack of time. Simultaneously, the issue of healthcare quality improvement will be considered by comparing patient outcomes in the scenario that involves the BREATHE framework to the one that includes traditional approaches to time and stress management. It is believed that the specified assessment will lead to insights that will shed light on the opportunities for reducing workplace burnouts and stress in healthcare workers, thus preventing mental health issues from taking place among staff members. At the same time, the dynamics of nosing services’ quality will be analyzed to infer
PICOT Question
In nurses working in the clinical setting under extensive time and workload pressure, does the application of the BREATHE framework have a better effect on the problem of burnouts and fatigue compared to the traditional approach to time management and workload arrangement?
Literature Each Strategy Employed
The approaches to the problem of burnouts, fatigue, and similar mental health issues in nurses operating in the staff shortage settings have an impressive history in nursing literature. For instance, the concept of self-care, which has been perpetuated in the healthcare setting for decades, has been widely discussed as one of the most basic frameworks for handling burnout and fatigue in healthcare workers. However, the proposed technique does not allow handling the concern on a more profound level, specifically, by reconsidering the methods of addressing external factors instead of changing a nurse’s attitude to them (Adimando, 2018). Similarly, the BREATHE framework, while being comparatively new, has already been registered on the radars of several academic studies that have tested it successfully. Nonetheless, locating the effects of the program in the long term will be needed to prove its significance for managing burnouts and fatigue in nurses.
Evaluation of the Literature
The current literature that studies the subject matter offers a sizeable amount of information and quite clear directions for further research. While the universal applicability of the BREATHE program has not been proven yet, there are indications that it is likely to cause positive change. Moreover, studies show that the traditional approach toward fatigue and burnouts in the nursing setting has become barely of any use for nurses due to the rapidly increasing amount of information and tasks that they have to manage when tending to patients’ needs. Combined with a rapidly declining nurse-to-patient ratio, the specified factor is shown to have become a large problem in the present-day nursing environment. The literature from which the key data was obtained is relevant and credible, coming from recent peer-reviewed studies.
However, during the analysis of the literature, a gap in the existing research was located. The exact effects of the BREATHE program on the improvement in the levels of burnout in the workplace and especially the changes in service quality requires further scrutiny. While the effects on nurses’ health have been seen as generally positive, the effects that the program has on them developing resilience, time management abilities, and the skill of prioritizing tasks, at the same time retaining empathy as the basis for communication with patients still require further analysis. This study, in turn, will offer an insight into the outcomes of the BREATHE model application in the nursing setting.
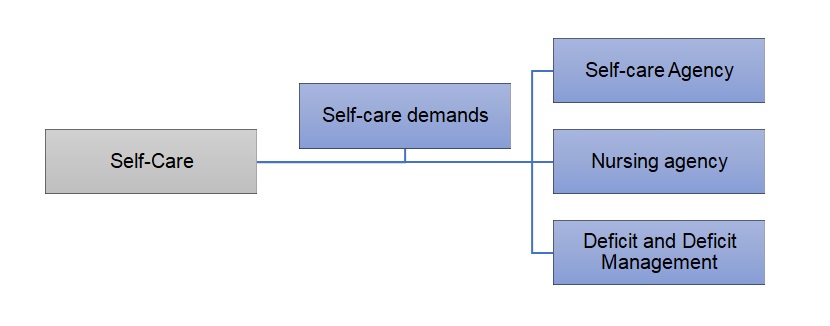
Nursing Theory Utilized
In order to approach the problem at hand, a combination of two theories will have to be applied. The nursing theory of Self-Care Deficit will have to be applied to the case under analysis since there is an evident lack of awareness about coping methods among nurses (see Figure 1). Created by Dorothea Orem, the Self-Care Deficit Theory suggests that people should be actively taught to address their personal health-related needs and locate threats to their well-being (Arman & Hök, 2016). By educating nurses about basic methods of self-care to prevent burnout and reduce stress, will prompt gradual change. At the same time, the Conservation of Resources theory will have to be utilized to assist nurses in developing the most appropriate strategy for managing time and workload (Prapanjaroensin, Patrician, & Vance, 2017). Thus, the work-life balance will be restored for nurses, and they will face less pressure in the hospital setting.
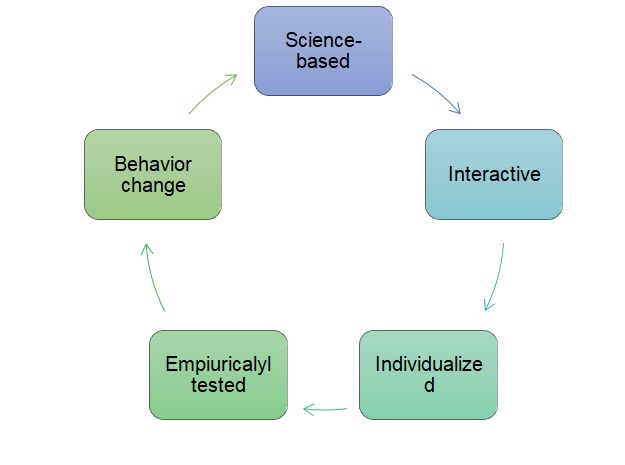
Proposed Implementation Plan with Outcome Measures
It is suggested that the promotion of fatigue and burnout management in nurses should start with the introduction of the BREATHE framework into the organizational environment (see Figure 2). Starting with a transfer of the dialogue concerning workload and burnouts with nurses to the digital environment, the process should continue with the introduction of nurses to each module at a time. As nurses progress to the next module, they will be offered an opportunity to engage in a discussion and consider the effects that the program will have had on them. Alterations in behaviors and attitudes will be the key talking point during the discussions since it will be crucial that nurses should build a profound understanding of their personal needs and abilities. As a result, nurses will gain better control of their emotions and, thus, will cope with workplace stress and challenges with greater success. The program will end with the evaluation of progress and the discussion of further directions for increasing self-control and management skills.
Identification and Discussion of Potential Barriers to Plan Implementation
While the plan seems quite basic in its essence, several barriers toward its implementation are expected to appear. Resistance to change may become an issue since some nurses may feel uncomfortable with the use of digital technology of which they have little knowledge. In addition, the costs associated with the integration of the BREATHE program into the target healthcare setting may be quite high, especially given the current drop in quality associated with the reduction in nurses’ productivity. However, the specified limitations can be addressed by refocusing the company’s financial policy and investing in nurses’ well-being and motivation. The described step will also help to manage the issue of reluctance toward change among the target demographic. By proving to the hospital staff that managers care about their employees, the former will encourage nurses to acquire new skills and focus on the creation of a healthy workplace.
References
Adimando, A. (2018). Preventing and alleviating compassion fatigue through self-care: An educational workshop for nurses. Journal of Holistic Nursing, 36(4), 304-317. Web.
Akbar, R. E., Elahi, N., Mohammadi, E., & Khoshknab, M. F. (2016). What strategies do the nurses apply to cope with job stress? A qualitative study. Global Journal of Health Science, 8(6), 55. Web.
Arman, M., & Hök, J. (2016). Self‐care follows from compassionate care–chronic pain patients’ experience of integrative rehabilitation. Scandinavian Journal of Caring Sciences, 30(2), 374-381. Web.
Hersch, R. K., Cook, R. F., Deitz, D. K., Kaplan, S., Hughes, D., Friesen, M. A., & Vezina, M. (2016). Reducing nurses’ stress: A randomized controlled trial of a web-based stress management program for nurses. Applied Nursing Research, 32, 18-25. Web.
Hevezi, J. A. (2016). Evaluation of a meditation intervention to reduce the effects of stressors associated with compassion fatigue among nurses. Journal of Holistic Nursing, 34(4), 343-350. Web.
Johnson, W. G., Butler, R., Harootunian, G., Wilson, B., & Linan, M. (2016). Registered nurses: The curious case of a persistent shortage. Journal of Nursing Scholarship, 48(4), 387-396. Web.
Prapanjaroensin, A., Patrician, P. A., & Vance, D. E. (2017). Conservation of resources theory in nurse burnout and patient safety. Journal of Advanced Nursing, 73(11), 2558-2565. Web.
Sagherian, K., Clinton, M. E., Abu-Saad Huijer, H., & Geiger-Brown, J. (2017). Fatigue, work schedules, and perceived performance in bedside care nurses. Workplace Health & Safety, 65(7), 304-312. Web.
Woodhead, E. L., Northrop, L., & Edelstein, B. (2016). Stress, social support, and burnout among long-term care nursing staff. Journal of Applied Gerontology, 35(1), 84-105. Web.