The Pathophysiology of Chronic Venous Insufficiency
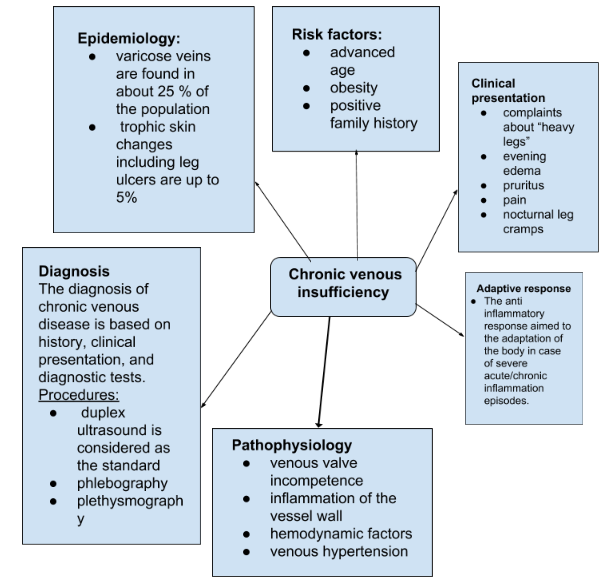
According to Santler and Goerge (2017), chronic venous insufficiency (CVI) is a well-known disorder associated with a variety of symptoms in later disease stages, which is reported to be considered common within the population of the U. S. Most notably, varicose veins with or without edema are the primary manifestation of the disease as they are found in about 25 % of the population (Santler & Goerge, 2017, p. 538). Concerning pathophysiology of the disease, it is possible to notice that its nature is not fully understood; however, it is possible to mention that the primary pathogenesis contributors are venous valve incompetence, inflammation of the vessel wall, hemodynamic factors as well as venous hypertension (Santler & Goerge, 2017; Eberhardt & Raffetto, 2014).
The Pathophysiology of Deep Venous Thrombosis
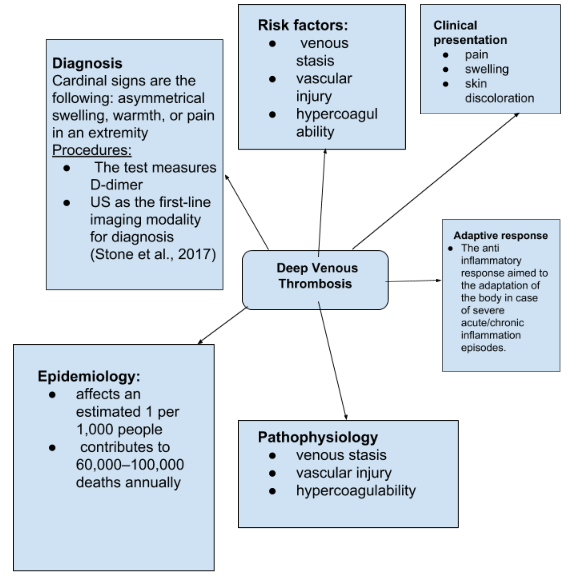
Deep venous thrombosis (DVT) is a well-recognized disease in the scholarly nursing literature that has numerous negative consequences (Stone et al., 2017; Mazzolai et al., 2017; Wu, Luo, & Zhang, 2016; Bouman, Cate‐Hoek, Dirksen, & Joore, 2016). Stone et al. (2017) observe that this disease is one of the primary causes of morbidity and mortality worldwide as it “affects an estimated 1 per 1,000 people and contributes to 60,000–100,000 deaths annually” (p. S276). Concerning the pathogenesis of DVT, it tends to occur in areas decreased or mechanically altered blood flow that causes the oxygen tension to decrease, which results in a coincident increase in hematocrit (Stone et al., 2017).
The Comparison of Similarities and Differences between CVI and DVT
Regarding the comparison of these two diseases, it is essential to notice that they have considerably similar pathophysiology, symptoms, and clinical presentation. It is evident from the articles utilized in this paper that one of the core causal aspects of the development of both disorders is the malfunction of venous valves (Santler & Goerge, 2017; Stone et al., 2017). However, it could be stated that CVI and DVT are different in the following way: CVI is characterized more as a venous reflux, caused by inflammation of veins, while DVT is determined primarily by the obstruction of veins provoked by venous stasis, vascular injury, and hypercoagulability (Stone et al., 2017; Wu et al., 2016).
How Venous Thrombosis is Different from Arterial Thrombosis
As it is mentioned by Poredoš (2017), venous and arterial thrombosis has been treated as a completely different condition over the history of medicine. However, the author argues that recent discoveries indicate that etiopathogenetic mechanisms of both diseases could be considered similar (Poredoš, 2017). Therefore, it could be concluded that these conditions could be treated in a relatively same manner.
The Impact of the Patient Factor on the Pathophysiology of CVI and DVT
For the purposes of this paper, the “behavior” patient factor is chosen, and this section aims to discuss how this factor impacts the pathophysiology of CVI and DVT. Eberhardt & Raffetto (2014) mention that such practices as prolonged standing and perhaps a sitting posture at work are related to behavioral factors associated with CVI. Additionally, it is appropriate to mention that patients with higher education usually display more healthy behavioral patterns compared to patients with lower levels of education (Bouman et al., 2016). After the diagnosis, which is based on such symptoms as pain, swelling, increased skin veins visibility, erythema, and cyanosis, it is possible to prescribe treatment: Apixaban 10 mg bid for 7 days, Dabigatran 150 mg bid preceded by LMWH for 5-10 days, and several other medications (Mazzolai et al., 2017, p. 1320). On the following two pages, mind maps for both diseases will be provided in order to structure the essential aspects of the conditions properly.
Mind Map: Chronic Venous Insufficiency
Mind Map: Deep Venous Thrombosis
References
Bouman, A. C., Cate‐Hoek, T., Dirksen, C. D., & Joore, M. A. (2016). Eliciting patients’ preferences for elastic compression stocking therapy after deep vein thrombosis: Potential for improving compliance. Journal of Thrombosis and Haemostasis, 14(3), 510-517.
Eberhardt, R. T., & Raffetto, J. D. (2014). Chronic venous insufficiency. Circulation, 130(4), 333-346.
Mazzolai, L., Aboyans, V., Ageno, W., Agnelli, G., Alatri, A., Bauersachs, R.,… & Konstantinides, S. (2017). Diagnosis and management of acute deep vein thrombosis: A joint consensus document from the European society of cardiology working groups of aorta and peripheral vascular diseases and pulmonary circulation and right ventricular function. European heart journal, 39(15), 1316-1330.
Santler, B., & Goerge, T. (2017). Chronic venous insufficiency–a review of pathophysiology, diagnosis, and treatment. JDDG: Journal der Deutschen Dermatologischen Gesellschaft, 15(5), 538-556.
Stone, J., Hangge, P., Albadawi, H., Wallace, A., Shamoun, F., Knuttien, M. G.,… & Oklu, R. (2017). Deep vein thrombosis: Pathogenesis, diagnosis, and medical management. Cardiovascular Diagnosis and Therapy, 7(3), S276-S284.
Poredoš, P. (2017). Interrelationship between venous and arterial thrombosis. International angiology: a journal of the International Union of Angiology, 36(4), 295-298.
Wu, M. K., Luo, X. Y., & Zhang, F. X. (2016). Incidence and risk factors of deep venous thrombosis in asymptomatic iliac vein compression: A prospective cohort study. Chinese medical journal, 129(18), 2149.