Introduction
The use of ultrasound in the field of medicine is one of the myriads of examples of the practical applicability of physics principles. Its use in this field actually began in the early 1930s and it has continued to advance in leaps and bounds. Ultrasound is actually a high-frequency cyclic sound that cannot be heard by the human ear and is estimated to be 20 KHz though1.
The medical uses of ultrasound are:
- Pregnancy confirmation and progress monitoring
- Analysis of foetal abnormalities
- Diagnosis of various complications of the gall bladder
- Examination of the flow of blood
- Examination of glands such as the thyroid gland
- Heart assessment for cardiac abnormalities
- Checking for infections in certain body parts
- Evaluation and inspection of abnormal growths and tumours
- Evaluation of reproductive organs
The above are some of the external uses of ultrasound. More recent scientific breakthroughs now allow for internal use where a device known as a transducer is inserted in some of the body openings to reveal the internal state of surrounding areas. This invasive technique can now be used to view mens’ prostrates when inserted via the rectum, to view the female internal reproductive organs when inserted through the vagina and to view the heart when the transducer is placed into the oesophagus2.
Having examined these uses of ultrasound, we now focus on three modalities in medicine that involve the use of ultrasound. These three are, CW Doppler and M-Mode Imaging. We shall now discuss briefly giving the operating principles and operations attached to each modality.
Colour Flow Doppler
Colour flow Doppler imaging is a recent exciting use of ultrasound. It is actually an improvement of the conventional pulsed wave Doppler imaging technique (Conventional PW). Doppler imaging is the use of an ultrasound device to noninvasively view blood flow in the heart and subsequent display of data in a two-dimensional image.
The use of color flow improves greatly on earlier versions since color assists to differentiate between various parts of the image such as inflow and outflow. This enables doctors to identify in a much shorter time, any valvular, congenital, or other heart complications. To an inexperienced user, color flow Doppler makes easier understanding3.
The color coding of the image is enabled by the detection of changes in blood flow velocity. The color red is used to denote blood flowing towards the transducer while blue shows blood flowing in the opposite direction (Fig 1.1). It is also possible to verify the velocity of red blood cells thus through imaging, quantification of blood levels is possible. This also helps in pressure examination within the atria, ventricles, and also the volume of blood per stroke.

The above diagram displays the use of color flow imaging to show mitral regurgitation4. The color bar in the top right corner indicates the direction of blood flow and is enhanced below.
Red And Blue Colours Show Opposite Flow. Black Represents Absence Of Flow And The Various Shades Of Red And Blue Denote Increased Or Decreased Velocity.
Color flow Doppler can also be used in laparoscopy to quickly identify valves and ducts in the viscera thus enabling giving spatial information on various tumors or other abnormalities in the liver and pancreas. Colorectal metastases of the liver are also easily viewed on color flow as compared to conventional PW techniques that involve complex spectra.
So how does color flow Doppler work? Since it is not possible to conduct a high-quality image simultaneously with a high-frequency pulse wave, the color flow technique employs a separate processor to form a color image which is then integrated into the subsequent anatomic image. Color flow images are produced from return frequency shift data from the scanner that traditionally had been ignored. Data from the scanner is thus color flow data or anatomic and both are alternated to produce the final image. Fig 1.3 is a simple explanation of this.
CW Doppler
Continuous Wave Doppler, popularly known as CW Doppler is a simpler but older version of the conventional Pulse Wave Doppler (PW Doppler). It is an ultrasound technique that measures the velocity of blood flow. CW Doppler works through the continuous transmission of high-frequency ultrasound by a piezoelectric crystal employed in a transducer while another crystal systematically picks up echoes of the ultrasound to form a pattern that can be translated to have medical meaning.
Through continuous transmission, it is impossible to differentiate different depths since the echoes are received simultaneously. This acts as a disadvantage but the reason for conversion from a PW Doppler to a CW Doppler is to enjoy the advantage of measuring higher velocities. This is achieved through the precision setting of the piezoelectric crystals to sensitize the transducer. Aliasing which refers to incorrect estimation of frequency due to smaller samples is avoided in CW Doppler due to high sensitivity even to low frequencies and thus CW it is definitely a more accurate ultrasound technique6 compares to PW Doppler.
CW Doppler can be referred to as a stand-alone ultrasound method since it does not yield anatomic information thus making it one of the most difficult ultrasound techniques to interpret. Complexity is furthered if the sonic beam falls on more than one chamber or vessel. Advances in technology however have assisted in the interpretation through a program that produces a two-dimensional image while performing CW Doppler functions. This is normally done by switching the transducer from one function to the other but since it happens at very fast speeds, the viewer gets the impression that both are continuous and in real-time8.
When the image is being formed quasi simultaneously, no data is actually being gathered so preceding data helps in generation of an estimate. This is the displayed data at the collection period resulting into a poorer quality image and unreliable data. Some of these setbacks are what has led to adoption of PW Doppler which though may be inaccurate in frequencies; it makes up for this during tabulation by giving an accurate account of the data.
M-Mode Imaging
M-mode imaging usually employs an ultrasound beam to produce very high resolution (over 1000fps) of body tissue and vessel walls. It is mostly used for cardiovascular tests so as to evaluate valve and myocardium movements. It can also be used to study movements in vessel walls. M-mode utilizes software tools to quantify various cardiac parameters such as fractional shortening, cardiac output and ejection fraction9.
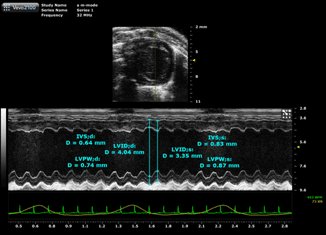
The imaging allows the viewer to witness both systole and diastole.
The M in M-mode stands for motion since the imaging aims at capturing motion. Fast sequences of B-mode (the two dimensional image) produce a pattern that can be interpreted as motion. It is from the sequence that the range of motion can be measured. M-mode imaging like other kinds of imaging has several distinct advantages and disadvantages.
The benefits are that it enables “live” viewing of the organ movements thus a diagnosis can be drawn on the spot. These live images enable ultrasound guided injections and biopsies that are somewhat difficult to achieve using other modalities. It can differentiate in high resolution between bone, soft and muscle tissue and doctors can get to draw a line between solid and fluid gaps.
Additionally, m-mode imaging does not have any known side effects or complications. It is much cheaper than computer tomography (CT) and MRI but still achieves high spatial resolution. Finally, the imaging scanners are smaller, portable and more widely available than any other modalities.
The disadvantages of m-mode imaging are that it does not penetrate bone tissue in a clearer manner as other modalities such as computer tomography that uses x-rays. It also has poor results when affected by air (gases). Results may vary depending on the frequency of imaging and finally, body habitus such as obesity causes it to produce poorer quality images. It does not also give what is known as a scout image that informs the viewer what part of the body is being depicted10.
Conclusion
The use of ultrasound as a modality for cardiovascular research and other internal diagnostics has grown from inception in the early 20th century. Technological advancements have aided growth in this area that has been termed as one of the safest and non-invasive modalities of clinical study. The advantages of Colour Flow, CW and M-Mode Imaging are but some of the few benefits that come with the use of ultrasound. Other types of sonography do exist such as A-mode, B-mode and Duplex that involve use of ultrasound in clinical study.
The most important factor is the relevance of these methods in the study where employed. As stipulated, all the three modalities apply to cardiovascular research and their effectiveness has had varying results. While technology may have come up with novel modalities such as CT and MRI, the use of ultrasound still remains relevant in clinical studies. Though there may be some disadvantages as highlighted in the essay, technology will over time correct them but the use of ultrasound will remain efficacious for a very long time.
Bibliography
Bio effects Committee of the American Institute of Ultrasound in Medicine, “American Institute of Ultrasound in Medicine Consensus Report on Potential Bio effects of Diagnostic Ultrasound: Executive Summary”. Journal of Ultrasound in Medicine 27 (4) (2008) 6-12.
Bunce, Stephen, Alan Hough, and Ann Moore. Measurement of abdominal muscle thickness using M-mode ultrasound imaging during functional activities. Eastbourne: Elsevier Science Ltd, 2004.
Cochrane organization. Ultrasound for foetal assessment in early pregnancy. 2010. Web.
Dion, J. L, A. Malutta and P. Cielo, “Ultrasonic inspection of fiber suspensions”, The Journal of the Acoustical Society of America 72 (5) (1982).
Duke University Medical Centre, Echo intext online. 2010. Web.
Hangiandreou, Naams. “Physics Tutorial for Residents: Topics in US: B-mode” US: Basic Concepts and New Technology-Radiographics 23(4) (2003).
Kisslo, Joseph and David Adams. Doppler Colour Flow Imaging. New York: Charles Livingstone, 1988.
Medindia Health Network. Medindia Health Online. 2010. Web.
Robertson, Valma and Kerry G Baker. “A Review of Therapeutic Ultrasound: Effectiveness Studies” Physical Therapy Journal 81 (2001)46-56
Takeda, Said. Morioka, Miyashita, A. Okumura, Yoshida and Koda, Matsumoto. “Age variation in the upper limit of hearing” European Journal of Applied Physiology 65 (5) (1992).
Footnotes
- Encyclopaedia Britannica, Encyclopaedia Britannica Online. 2010, sv “ultrasound”.
- Medindia Health Network: Medindia Health Online. Web.
- Joseph Kisslo & David Adams, Doppler Colour Flow Imaging (New York: Charles Livingstone, 1988), 1.
- Joseph Kisslo et al 3
- Joseph Kisslo et al 3
- Medicyclopaedia, Medicyclopaedia Online. 11 October 2010. Sv “CW Doppler imaging”
- Duke University Medical Centre, Echo intext online. Web.
- Duke University Medical Centre7
- Steve M. Bunce, Alan D. Hough and Ann P. Moore, Measurement of abdominal muscle thickness using M-mode ultrasound imaging during functional activities (Eastbourne: Elsevier Science Ltd, 2004) 41-44.
- Valma J Robertson and Kerry G Baker, “A Review of Therapeutic Ultrasound: Effectiveness Studies” Physical Therapy Journal 81 (2001).