Introduction
Tetraiodothyronine (T4) and triiodothyronine (T3) are the primary hormones the thyroid gland produces. The two hormones have similar roles in a normal body, but T3 is more potent. Specifically, their functions include regulating metabolism, enhancing the release of energy from carbohydrates and fatty acids, and increasing protein synthesis (Shahid et al., 2022). Moreover, the hormones determine the basal metabolic rate (BMR), the number of kilojoules needed to maintain function during inactivity. The two hormones ensure normal nervous system maturation, which is essential for normal growth and development.
The T3 and T4 have a permissive role, so they are needed for the rest of the hormones to function (Ellie Kirov, 2021). T3 and T4 act on the cell work when they dissociate from the binding transporter protein and enter cells through carrier-mediated transport or diffusion. There is a circulation of intercellular conversion in which T3 and T4 bind to the thyroid hormone receptor subtype alpha-1, beta-2, or beta-1 in the nucleus, regulating genetic transcription in a canonical pathway (Teixeira et al., 2020). They then bind to the tissue’s beta or nuclear alpha receptors to activate transcription, leading to cell-specific responses.
Graves’ Disease vs. Other Hyperthyroidism
Graves’ disease is one of the hyperthyroid conditions characterized by exophthalmos, a condition marked by bulging eyes due to the enlargement of the fat pads behind the eyeballs. Patients with this condition have elevated levels of T4 and T3 hormones and reduced levels of thyroid-stimulating hormone (TSH). Additionally, TSH-receptor antibodies can lead to the differentiation of adipocytes and the proliferation of orbital fibroblasts (Shahid et al., 2022).
Consequently, the production of glycosaminoglycan and hyaluronic acid increases, resulting in a high volume of muscle tissue and intraorbital fat (Ellie Kirov, 2021). Comparatively, other hyperthyroidism diseases in adults slow the metabolic state, leading to a slow heart rate and sluggish peristalsis, which causes constipation, low energy, weight gain, hair loss, and low body temperature.
Relation to the Patient’s Symptoms
The patient reports losing weight despite eating normally and sometimes more. Her boyfriend confirms that she has been feeling tired more frequently. Additionally, she has been experiencing excessive sweating, even in mild temperatures (Mayo Clinic, 2022). Her bowel movements have become more frequent, she experiences a fast heart rate without a cause, and she even made an appointment with the doctors due to a swollen throat (Mayo Clinic, 2022). The symptoms that the patient is presenting with are typical of Graves’ disease.
Hormonal Pathways
For a well-functioning human, the hypothalamus first produces the hypothalamic releasing hormone. Resultantly, it stimulates the secretion of TSH by the anterior pituitary gland. Next, the TSH causes the thyroid gland to secrete the hormones T3 and T4. The secretion continues until the thyroid hormone plasma levels sufficiently increase, which causes a negative feedback inhibition that prevents further production of TSH.
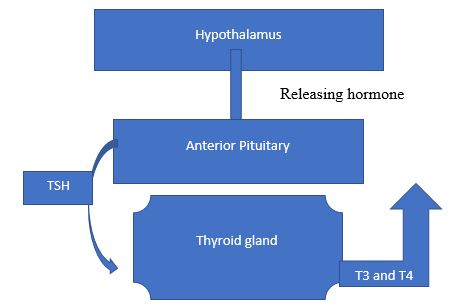
People with Graves’ disease have an autoimmune condition that results from the production of the TSH receptor antibodies. The antibodies, thyroid-stimulating immunoglobulins (TSI), stimulate the growth of the thyroid gland, leading to an abnormal and excessive increase in T4 and T3. While at the same time, the release of TSH decreases. The immunoglobulin works against the TSH-receptors to increase the growth and activity of the TSH-receptor. Having an excess of thyroid hormones causes hyperthyroidism.
Effects of Altered Thyroid Hormone Levels
Dysfunction of the thyroid hormone affects various tissues in the body, resulting in symptoms similar to those of Graves’ disease. Normally, energy expenditure through physical activity causes the production of heat. The pancreas is a retroperitoneal organ with both exocrine and endocrine functions. It produces various hormones needed for fat, glucose, and fat metabolism. The thyroid hormones help in the development and maturation of pancreatic cells and the expression of beta cells. Hyperthyroidism causes an increased metabolic rate resulting from excessive stimulation of thyroid hormones.
Resultantly, the patient experiences peripheral vasodilation, and the blood vessels widen. Moreover, the thyroid hormones uncouple phosphorylation oxidation, making more energy present as heat. Hyperthyroidism affects plasma glucose levels through the interference of BMR and other mechanisms in the liver. Notably, the T3 and T4 are also involved in directly controlling body temperature, sympathetic activity, and appetite (Teixeira et al., 2020).
The thyroid hormone antagonizes the liver, leading to increased hepatic output of glucose (Huether & McCance, 2020). The T3 and T4 may also favor catecholamine-induced lipolysis in the adipocytes, leading to insulin resistance. Regarding glucose, it stimulates the production of glucose and lipids and interferes with regulating the cardiovascular system. Hyperthyroidism causes hyperglycemia and can cause the liver to overproduce glucose.
Rationale for Losing Weight Without Exercise
The energy expenditure and intake influence whether a person gains or loses adiposity. Notably, the basal metabolic rate is only used in the cellular process to maintain life. When a person has Graves’ disease, the thyroid is overstimulated, causing the body to burn more energy during rest (Huether & McCance, 2020). The implication is that people may eat more. However, they still lose weight because their bodies continually break down fuel so fast that it cannot be replenished.
Moreover, there is an intricate relationship between the metabolism of the thyroid hormone and the liver. The TH controls lipid metabolism of cholesterol homeostasis, which can influence body weight (Cicatiello et al., 2020). Thus, a person with Graves’ disease has to eat more to compensate for the demand so that the body does not start consuming vital organs like the bones.
Complications of Graves’ Disease and Blood Pressure
The renin-angiotensin-aldosterone system (RAAS) is a significant component in normal blood pressure regulation. It increases systemic vascular resistance and blood volume when hormonal changes occur. The RAAS system begins with renin, which is released to respond to the high levels of salt in the blood, reduced renal blood flow, or nervous system stimulation when working on beta-1 receptors (Nocciolino, 2020). Next, the renin converts angiotensinogen to angiotensin-2, which increases salt reabsorption while increasing plasma volume. The actions cause vasoconstriction in the systemic circulation and renal microvasculature, leading to efferent arteriole constriction.
Conclusion
In Graves’ disease, the T3 induces erythroprotein synthesis, causing an increase in the mass of red cells. The thyroid hormone decreases resistance in the arterioles by directly affecting the vascular smooth muscle cells, causing arterial pressure (Ilie, 2019). The result is an increase in renal sodium absorption and activation of the renin-angiotensin-aldosterone (Arslan & Altay, 2021).
Notably, increases in thyroid hormones are among the top isolated reasons for systolic hypertension. In addition, Graves’ disease is associated with pulmonary hypertension because the thyroid hormone’s role in lowering the systemic vascular resistance may not happen in the pulmonary vasculature due to hyperthyroidism. Graves’ disease can then manifest as complications such as tricuspid regurgitation and right heart failure.
References
Arslan, A., & Altay, H. (2021). Graves’ disease and cardiac complications. Graves’ Disease. Web.
Cicatiello, A. G., Di Girolamo, D., & Dentice, M. (2018). Metabolic effects of the intracellular regulation of thyroid hormone: Old players, new concepts. Frontiers in Endocrinology, 9(1), 1-7. Web.
Ellie Kirov, B. (2021). Herlihy’s The Human Body in Health and Illness Study Guide, 1st ANZ edition. Elsevier Health Sciences.
Huether, S. E., & McCance, K. L. (2020). Understanding pathophysiology – Binder ready. Elsevier.
Ilie, I. R. (2019). Introduction to endocrinology. Springer Nature.
Mayo Clinic. (2022). Graves’ disease – Symptoms and causes. Web.
Nocciolino, M. (2020). Regulation of blood pressure. Geeky Medics. Web.
Shahid, M. A., Ashraf, M. A., & Sharma, S. (2022). Physiology, thyroid hormone. In StatPearls [Internet]. Web.
Teixeira, P. D., Dos Santos, P. B., & Pazos-Moura, C. C. (2020). The role of thyroid hormone in metabolism and metabolic syndrome. Therapeutic Advances in Endocrinology and Metabolism, 11(4), 1-33. Web.