Case Summary
A 35-year old female patient reported to the nursing office, complaining about “bad headaches,” which have been present for the past two years, right after the birth of her first child. The headaches interrupt the patient’s sleeping patterns and cause enough pain to make the patient cease all activity and seek medication and rest. Additional symptoms include vomiting. The primary medication used in the event of a headache is Tylenol. The condition had been worsening over the past 6 months, forcing the woman to visit a healthcare specialist.
Additional Questions to Ask
The data provided in the case study is not sufficient to place an accurate diagnosis. Additional questions regarding the patient’s status are as follows (Ashina & Gepetti, 2015):
- Could you describe the location of the headache? (would help determine if it is bilateral or unilateral);
- Could you describe how does the headache feels? (throbbing motions, constant aches, sharp pulses, etc.);
- Could you estimate the duration of the headache?
- Could you rate the pain on a scale of 1 to 10?
- Do you see any auras around individuals or objects? Is the headache triggered by light or sound?
- Do the headaches occur around a specific time of the month? (Possible relation to the menstrual cycle);
- Additional information about current medications, food choices, allergies, and family history of headaches (Mitsikostas & Paemeleire, 2016).
- Information about the patient’s current occupation.
Classification of Headaches
Headaches are classified based on their type. There are two kinds of headaches: essential and auxiliary. Migraines, tension, cluster pains, sinus infections, and hormonal disorders cause essential headaches, which constitute around 90% of all cases of headaches (Ashina & Gepetti, 2015).
Trauma, metabolic changes, neurological issues, and substance abuse typically cause auxiliary headaches. This type of headache can also be attributed to infection and intracranial pressure. The number and severity of headaches determine the course of action, as an onset of sharp headaches may indicate life-threatening conditions, such as the transient ischemic attack (TIA), post-lumbar puncture, or subarachnoid hemorrhage (Ashina & Gepetti, 2015).
Old and New Headaches
The primary parameters for determining if the headache is an old or new one are the duration and frequency of the condition. Essential headaches, such as migraines, last between four and 72 hours, whereas a cluster headache lasts between 15 minutes and up to three hours (Gurr, 2018). The patient from the case study seems to suffer from a chronic condition that lasted for 2 years, with the issue becoming worse over the past 6 months. The fact that the situation is getting worse is a cause for concern, indicating underlying physical and neurological degradation.
Making a Definite Diagnosis
Utilizing open-ended history and asking focused questions would help determine the type of headache the patient is suffering from. Typical diagnoses for essential headaches include migraine, tension, cluster, and other kinds of afflictions. Auxiliary headaches are much harder to diagnose. A final assessment should be made only after the physical and neurological examinations as well as laboratory tests have been completed. Particular attention should be paid towards cranial nerves 2 to 10 (Gurr, 2018). It is important to pay attention to the patient’s head and neck, as some headaches are caused by skeletomuscular disorders.
Distinguishing Between Benign and Serious Headaches
The interview and history of the patient can provide vital subjective data that would enable the completion of physical and neurological assessments and determine the severity of the issue. Typically, a severe headache in need of urgent medical attention has some of the following symptoms (Ashina & Gepetti, 2015):
- High levels of pain (6-10 out of 10);
- Papilledema (optical disk swelling);
- Altered mental status (the headache is actively affecting the patient’s capabilities of perceiving and interacting with the environment);
- High fever (a common symptom to many conditions, often associated with infections);
- Muscle rigidity (also associated with infections);
- Nuchal rigidity (common in headaches originating from the neck and back);
- Symptoms of a cerebrovascular accident (CVA), or TIA.
While many of these symptoms could be associated with numerous causes, they help determine the state of urgency and the seriousness (or benignity) of the headache. In the case study, the descriptions indicate that the headache translated from benign to serious in the last 6 months.
Diagnostic Tests
Several tests need to be taken to ensure the accurate final diagnosis for the female patient. These tests include the following (Ashina & Gepetti, 2015):
- Blood tests;
- Hormone level tests;
- Thyroid level tests;
- Analysis of the patient’s urine;
- Computed tomography scan (CTS);
- Magnetic resonance imaging (MRI);
The first four tests would help determine if the headaches were caused by hormonal changes that occurred after the end of the pregnancy. Infection is possible, but unlikely, as the headaches persisted for over 2 years. CTS and MRI would help detect any potential abnormalities within the brain.
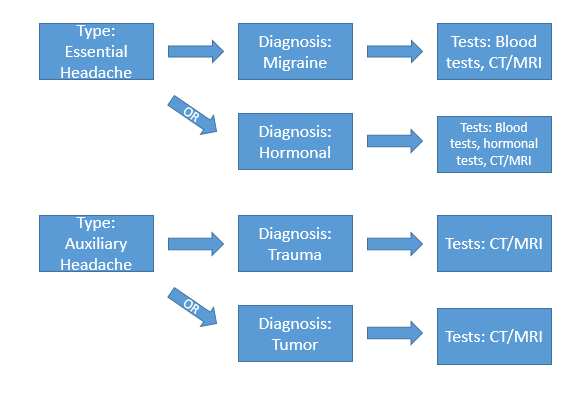
Diagnosis Flow Sheet
Figure 1 demonstrates the potential diagnosis that the patient from the case study might have as well as the diagnostics related to the differentials:
References
Ashina, M., & Geppetti, P. (2015). Pathophysiology of Headaches. Bern, Switzerland: Springer International Publishing.
Gurr, B. (2018). Headaches and brain injury from a biopsychosocial perspective: A practical psychotherapy guide. London, UK: Routledge.
Mitsikostas, D. D., & Paemeleire, K. (Eds.). (2016). Pharmacological management of headaches. Bern, Switzerland: Springer International Publishing.