Introduction
Human papillomavirus (HPV) is the most common sexually transmitted infection. More than 79 million Americans, both men and women, live with this infection today (Luna & Upadhyay, 2022). About 150 types of HPV are known, but new types are constantly emerging due to various homologous characteristics (Xu et al., 2020). Nurses encounter this pathogen and must understand its interactions, transmission details, and other contributing factors. The description of HPV will be given, with special attention to its virulence, immunity, epidemiology, prevention, treatment, and clinical relevance.
Description of the Microorganism
HPV is a viral infection belonging to the Papillomavirus family and is transmitted through skin-to-skin contact. It is “an icosahedral, uncoated particle composed of double-stranded DNA [deoxyribonucleic acid] of approximately 8,000 nucleotide base pairs” (Xu et al., 2020, para. 2). The diameter of this circular, double-stranded genome composed of 72 capsomeres is about 55 nm (Xu et al., 2020). In eight protein-coding genes, the genome is divided into three regions: early (E1 to E7 non-structural proteins), late (major and minor capsid proteins), and long control (L1 to E6 gene, 1000 bp in size) (Blanco et al., 2021). Clinicians use a colposcope or a dual-stain test on Pap test samples, which reveal two critical proteins (brown p16 and red Ki-67).
Virulence Factors
The main virulence factors of HP are early proteins (E6 and E7) that cause cervical lesions. These proteins inactivate the host’s tumor suppressor protein (p53) and retinoblastoma (Rb) tumor suppressor and enable the cells to replicate (Blanco et al., 2021). The number of cells after inactivation is hard to regulate, and malignant transformations proliferate. The amplification of viral genome copies is observed, and the expression of late genes is induced (Blanco et al., 2021). Cervical cancer is a common outcome of such genetic changes.
Immunity
The host’s innate immune response is one of the first-line defenses against HPV. When HPV reaches the epithelial layers, physical barriers like defensins or mucoproteins prevent the virus from affecting the keratinocytes (Gutiérrez-Hoya & Soto-Cruz, 2021). If this defense is ineffective and HPV penetrates the body, such cells as natural killer cells, macrophages, dendritic cells, and Langerhans (Gutiérrez-Hoya & Soto-Cruz, 2021). The specific immune response creates a strong inflammatory environment without visible changes or additional physiological needs.
Infectious Disease Information
Regarding the existing variety of HPV types, this pathogen can cause many diseases. According to Yousefi et al. (2022), HPV is the cause of about 5% of all cancers across the globe, including cervical cancer, genital cancer, and cancer in such organs as the vagina, penis, anus, and vulva. The incidence of oropharyngeal cancer and head and neck cancer also increases with such presenting symptoms as neck masses, a sore throat, and dysphagia (Timbang et al., 2019). Still, many HPV cases remain asymptomatic and latent infections, and individuals do not consider such signs as genital warts or cervical dysplasia as a warning. It may be a comorbid opportunistic pathogen only with human immunodeficiency virus infection in the sex organs or fluids.
Epidemiology
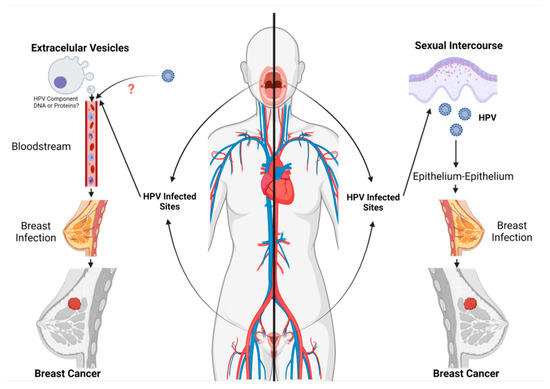
People get exposed to HPV when they have sex with someone who has already had the virus because it spreads through skin-to-skin or skin-to-mucosa contact. Humans are the only natural reservoirs for the virus, leading to such statistics as 13,800 new cases of HPV-related cancer in the United States and more than 5,000 deaths in one year (Luna & Upadhyay, 2022). One of its transmission routes is direct contact with an infected epithelium and the mammary epithelium when the virus enters through microlesions, as illustrated in Figure 1 (Blanco et al., 2021). Another transmission vector is also indicated in Figure 1 when the virus is released into the bloodstream and transferred to the breast (Blanco et al., 2021). At the same time, HPV can be transmitted to a child from an infected mother during childbirth.
Prevention
Vaccination is a highly recommended form of preventing HPV infections. Children aged between 13 and 17 receive the first dose of the HPV vaccine and the second dose in 6-12 months (Timbang et al., 2019). These prophylactic vaccines may be of several types: bivalent (Cervarix), tetravalent (Gardasil), and nonvalent (Gardasil 9) (Gutiérrez-Hoya & Soto-Cruz, 2021). Pediatricians and family therapists are responsible for educating patients about the importance of vaccination and protected sex to prevent HPV.
Treatment
HPV does not have a cure, and people have to live with the disease caused by this virus. Multiple chemotherapeutic interventions, surgery, and radiotherapy are recommended in the early stage. For example, cisplatin-based chemotherapy can be offered due to its binding capacity in the N7 reactive center, which allows the agent to destroy cancer cell DNA and prevent cell division (Gutiérrez-Hoya & Soto-Cruz, 2021). Warts and other skin problems may be treated with creams and other medications to freeze areas and remove them if possible.
Clinical Relevance
Many critical multidrug-resistant strains of HPV have been identified. Despite its genetic variety, including HPV 31, 33, 35, 58, 68, etc., the infection mechanism is almost identical (Kombe et al., 2021). HPV 16 and 18 are common and high-risk types that provoke cervical cell abnormalities and put healthcare providers, such as gynecologists, at risk during primary assessments. Antibiotics are ineffective for treating HPV strains; vaccination and safe contact are the only recommendations.
Conclusion
HPV is a dangerous pathogen that can be asymptomatic in people for an extended period. Its skin-to-skin transmission, various strains, and the absence of a cure make this virus dangerous for humanity. HPV may provoke many diseases, including cancers of all organs and tissues. Healthcare providers need to underline the importance of vaccination and safe sexual relationships to prevent HPV-related problems and reduce the number of deaths.
References
Blanco, R., Carrillo-Beltrán, D., Muñoz, J. P., Corvalán, A. H., Calaf, G. M., & Aguayo, F. (2021). Human papillomavirus in breast carcinogenesis: A passenger, a cofactor, or a causal agent? Biology, 10(8). Web.
Gutiérrez-Hoya, A., & Soto-Cruz, I. (2021). NK cell regulation in cervical cancer and strategies for immunotherapy. Cells, 10(11). Web.
Kombe, A. J. K., Li, B., Zahid, A., Mengist, H. M., Bounda, G. A., Zhou, Y., & Jin, T. (2021). Epidemiology and burden of human papillomavirus and related diseases, molecular pathogenesis, and vaccine evaluation. Frontiers in Public Health, 8. Web.
Luna, M., & Upadhyay, S. (2022). Trends in the utilization of human papillomavirus vaccines and the incidence of malignant cervical cancer in women and teenagers: A secondary analysis. Healthcare, 10(7). Web.
Timbang, M. R., Sim, M. W., Bewley, A. F., Farwell, D. G., Mantravadi, A., & Moore, M. G. (2019). HPV-related oropharyngeal cancer: A review on burden of the disease and opportunities for prevention and early detection. Human Vaccines & Immunotherapeutics, 15(7-8), 1920–1928. Web.
Xu, X., Kong, R., Liu, X., He, P., & Dai, Q. (2020). Prediction of high-risk types of human papillomaviruses using reduced amino acid modes. Computational and Mathematical Methods in Medicine. Web.
Yousefi, Z., Aria, H., Ghaedrahmati, F., Bakhtiari, T., Azizi, M., Bastan, R., Hosseini, R., & Eskandari, N. (2022). An update on human papilloma virus vaccines: History, types, protection, and efficacy. Frontiers in Immunology, 12. Web.