IPC in Nursing
Infection prevention and control (IPC) is a critical issue in nursing. Entering hospitals puts patients at risk of getting an infectious disease, usually higher than in a non-medical environment. More than 10% of patients in medical institutions acquire infections while in care, and about a third of surgical patients develop post-operative infections (“Infection prevention and control,” 2023). Nurses are generally responsible for implementing IPC practices.
IPC Definition
Infection prevention and control in hospitals is an approach that aims to stop the spread of infections in medical settings, including when nurses are the source of infection and when patients are infected. The Joint Commission (US) broadens the IPC purposes, identifying areas of IPC application in Coronavirus Antimicrobial Stewardship, Hand Hygiene, Infectious Disease Outbreaks and Response, Catheter-Associated Urinary Tract Infections, and Surgical Site Infections (SSI), as well as Vaccination (“Approach to standards compliance,” 2022).
The CDC adds to the definition, stating that IPC practices should be performed in all clinical facilities, such as hospitals, dialysis centers, outpatient clinics, and long-term care facilities, as well as among traditional practitioners (“COVID-19 Overview,” 2023). Unlike the CDC, the WHO defines the roles of active agents, including service recipients, healthcare workers, facility managers, and policymakers, thereby adopting a more inclusive approach (“Infection prevention and control,” 2023). Significantly, neglecting IPC practices can seriously harm and even kill. Therefore, adequate healthcare is impossible without the responsible implementation of IPC.
IPC and Nursing Code
The UK Nursing and Midwifery Council Code states that nurses should be aware of potential harm associated with their practice. Section 19 states that nurses should also reduce the risk of harm (“The Code,” 2018). Sections 19.3 and 19.4 provide that nurses must “keep to and promote recommended practice in relation to controlling and preventing infection,” and “take all reasonable personal precautions necessary to avoid any potential health risks to colleagues, people receiving care, and the public” (“The Code,” 2018, p. 20). The UK nursing code is more explicit in this regard, while the US ANA Code does not mention IPC at all. At the same time, US nurses are guided by the CDC’s Hand Hygiene guide, which is likely insufficient for appropriate interactions across all healthcare settings.
Creating a Mind Map
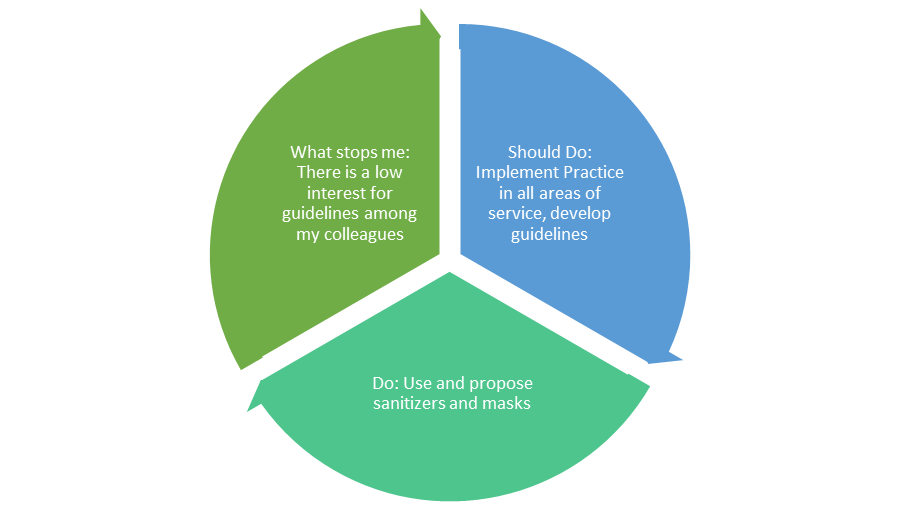
Importantly, given the above, the nursing codes do not necessarily cover all areas of IPC implementation, as suggested by the IPC definition. As a healthcare professional, I should be attentive to personal hygiene, like using sanitizers, gloves, new syringes, and disposable masks. I should also follow instrument sterilization procedures during surgical operations and implement the IPC policy at my workplace, spreading knowledge among patients. The latter can be performed by creating posters and leaflets, while guidelines describe disinfection procedures for each area providing services.
Currently, I try to adhere to my own hygiene rules and carefully monitor hand disinfection and mask use. I also offer sanitizer and masks to patients and inform them about the dangers of infectious diseases. However, some barriers can prevent me from performing some IPC activities, such as getting sick with a cold, when I objectively become a dangerous source of infection. As an active professional, I can seem a bit pushy when I offer patients sanitizers and masks, although it is an integral part of the practice. In other words, some patients take it personally when I suggest they use masks and sanitizers, which often stops me from performing IPC practices that require me to ensure patients are safe in the potentially dangerous environment of the clinic.
References
Approach to standards compliance (2022). The Joint Commission.
Infection prevention and control (2023). WHO.
COVID-19 Overview and Infection Prevention and Control Priorities in non-U.S. Healthcare Settings (2023). CDC.
The Code (2018). Nursing and Midwifery Council.