State Oversight of Managed Care Organizations (MCOs)
The Ohio care sector is fully privatized since private corporations provide managed care. The State Department of Medicaid is responsible for monthly payments to specific healthcare providers. This situation arose due to contracting with private corporations to administer Medicaid benefits.
The validity and terms of contracts at the state level may vary depending on a particular governor’s campaign. Previously, only medical companies were considered drug suppliers, limiting the normal functioning of pharmacy contracts (Schladen, 2021). However, later, the Ohio General Assembly passed a resolution that allowed medical organizations to receive payment for expanded services (Schladen, 2021). This has significantly improved the quality of services provided in the state.
Pharmacies also began to be considered suppliers, significantly improving the quality of the goods produced and their legal distribution. The receipt and distribution of any benefits for any population group occur due to the administration of the MCO. Thus, the state spends considerable resources to maintain the program. In other words, the MCO is the state’s most significant investment in healthcare development.
The state will reimburse the cost of services in accordance with a specific rate plan. That is, it is necessary to determine the value of the medical services provided. Usually, the specialization and urgency of medical intervention determine a higher tariff plan (Anthes, 2019).
It is also important to note that the ability to manage benefits is also in the hands of medical organizations. Previously, we used a different system fee for service. It is still presented in MCO, consisting of approximately ten percent (Anthes, 2019). Maintaining this scheme is less beneficial for the state but more acceptable for suppliers. Various concepts, such as per capita payment and medical loss ratio, are also prescribed under the contract. Therefore, the state controls managed care through contracted commercial company incentives.
Federal Oversight of Managed Care Organizations
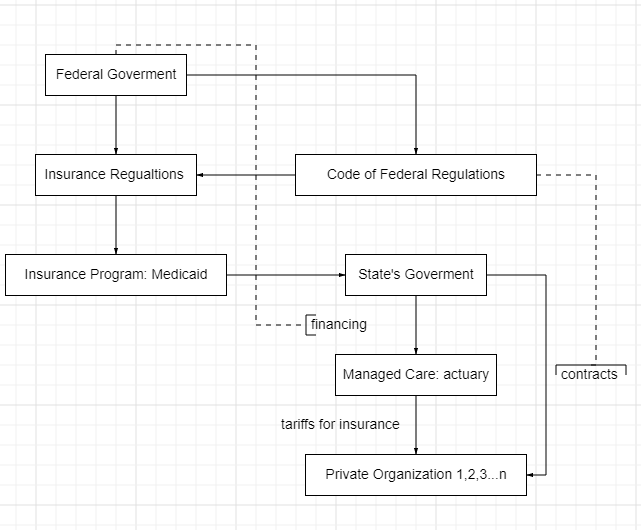
The state has an agreement with the federal government regarding the financial resources needed to adapt medical care plans. The federal government manages private-sector employers’ health plans (Anthes, 2019). Any extensions or possible changes to the insurance programs are under the federal government’s jurisdiction. In other words, the state can only participate in the existing insurance program. Thus, Ohio participates in the Medicaid program while many other possibilities exist (Anthes, 2019). The state regulates the local insights, which are the program’s options.
In other words, the insurance regulations are wholly federalized. The fee-for-service insurance pattern, which Ohio utilizes, is also advanced by the federal government. Thus, the state can establish the contract conditions. These data should comply with the generally established patterns the federal government provides. Contracts are also directly dependent on federal requirements (Anthes, 2019).
However, such factors as the state’s expectations and mutual responsibilities of the medical organizations are also addressed in the contracts. The gained data, the question of payment, and the quality of services are the mutual responsibility of the contract participants. A particular federal document called the Code of Federal Regulations outlines the structure of procedures during contract signing and design (Anthes, 2019).
Generally, the state’s activities are subordinated to federal law. Any MCO performance assessments or changes are held in the corners of federal law. Figure 1, shown below, shows a schematic visualization of Ohio’s state and federal oversight of managed care organizations.
References
Anthes, L. (2019). Engineering outcomes managed care value based design Ohio Medicaid. The Center for Community Solutions. Web.
Schladen, M. (2021). Ohio pharmacists, care provider say program is a national model. Ohio Capital Journal. Web.