QSEN Competencies include graduate, pre-licensure, and safety competencies targeted at developing skills and knowledge for future nursing graduates (QSEN, 2014). They include safety, quality improvement, patient-centered care, evidence-based practice, informatics, collaboration, and teamwork (QSEN, 2014). NLN competencies for nursing education include competencies for both nurse educators and graduates. For graduates, core competencies include the spirit of inquiry, human flourishing, nursing judgment, and professional identity (NLN, 2017a).
For nurse educators, core competencies include facilitating learning, development, and socialization, using evaluation and assessment strategies, participation in curriculum design, functioning as a change leader, engaging in scholarship (NLN, 2017b). AONE competencies are broad and were designed to help nurse executives to practice their leadership skills in a variety of areas such as communication and relationship building, knowledge of the healthcare environment, leadership, professionalism, and business skills.
QSEN competencies align the best with the practicum project of reducing door-to-ballon time in STEMI patients because they are relevant for addressing preventable errors in health care (Sherwood & Zomorodi, 2014) through interaction between healthcare providers and patients. The six competencies defined by QSEN encompass a range of practices and procedures that can potentially benefit the operational environment in the healthcare facility, especially when it comes to the goal of improving the quality of care and reducing door-to-balloon time among STEMI patients.
Patient-centered care is a crucial competency to implement in the context of reducing door-to-balloon time because the success of the project significantly depends on patient outcomes. The importance of incorporating QSEN competencies into the identified practicum project is explained by the need for nurses to have appropriate knowledge, attitudes, and skills targeted at improving the quality of care and subsequently reducing door-to-balloon time. Moreover, QSEN competencies have proven to be effective in establishing a foundation for future nurses to be proficient in their quality improvement and patient safety efforts (Cronenwett, Sherwood, & Gelmon, 2009) that have a positive impact on redefining existing practices in a healthcare setting and developing cohesive action plans for solving issues that negatively impact patient outcomes.
It is important to mention that QSEN competencies (safety, quality improvement, patient-centered care, evidence-based practice, informatics, collaboration, and teamwork) affect nurses the same way that they affect educators and administrators. The all-encompassing nature of the competencies allows every member of an interdisciplinary team to draw skills and knowledge necessary for reaching the set objective. The Kendall Regional Medical Center can utilize these competencies in the course of designing an action plan for reducing door-to-balloon time in STEMI patients. For example, the collaboration and teamwork competency can be utilized for developing a chain of steps for effective communication between teams in cases of clinical emergencies. Also, the informatics competency may be used for incorporating innovative information technologies into the process of reducing door-to-balloon time.
American Nurses Association is a regulatory body, to which the Kendall Regional Medical Center reports with regards to the key quality improvement procedures since the organization has set a mission to improve the quality, safety, and effectiveness of care for all citizens. Because the end goal of reducing door-to-balloon time at the facility is associated with improving patients’ outcomes, collaborating with the American Nurses Association with regards to the utilization of QSEN competencies can contribute to the project’s success.
Blog Post on the QSEN competency
Among the six competencies defined by QSEN, teamwork, and collaboration are the most relevant when discussing the reduction of door-to-balloon (D2B) time in a care setting. The competency is the most relevant because it encompasses a broad range of practices and procedures targeted at enhancing collaboration between emergency medical service providers, the emergency department personnel, the cardiovascular lab personnel, and interventional cardiologists (Mehta et al., 2009). Without the coordination of efforts and proper communication among the key players of a STEMI intervention, no quality improvement plan or informatics procedures will be successful. Moreover, as found by Mehta et al. (2009), the efficiency of D2B procedures was positively correlated with better teamwork. Measuring teamwork effectiveness in a healthcare setting can be a beneficial practice for identifying what procedures contribute to the reduction of door-to-balloon time and which procedures prevent the interdisciplinary team from reaching its goals.
It is also important to mention that collaboration and teamwork is a competency that enhances in the course of a project implementation because healthcare providers learn from their mistakes and make changes to improve their operation. The competency of collaboration and teamwork is intertwined with other QSEN competencies because the provision of quality care or safety relies on the knowledge and skills of health care providers. Therefore, without teamwork, the reaching of the goal to reduce door-to-balloon time in STEMI patients will be impossible.
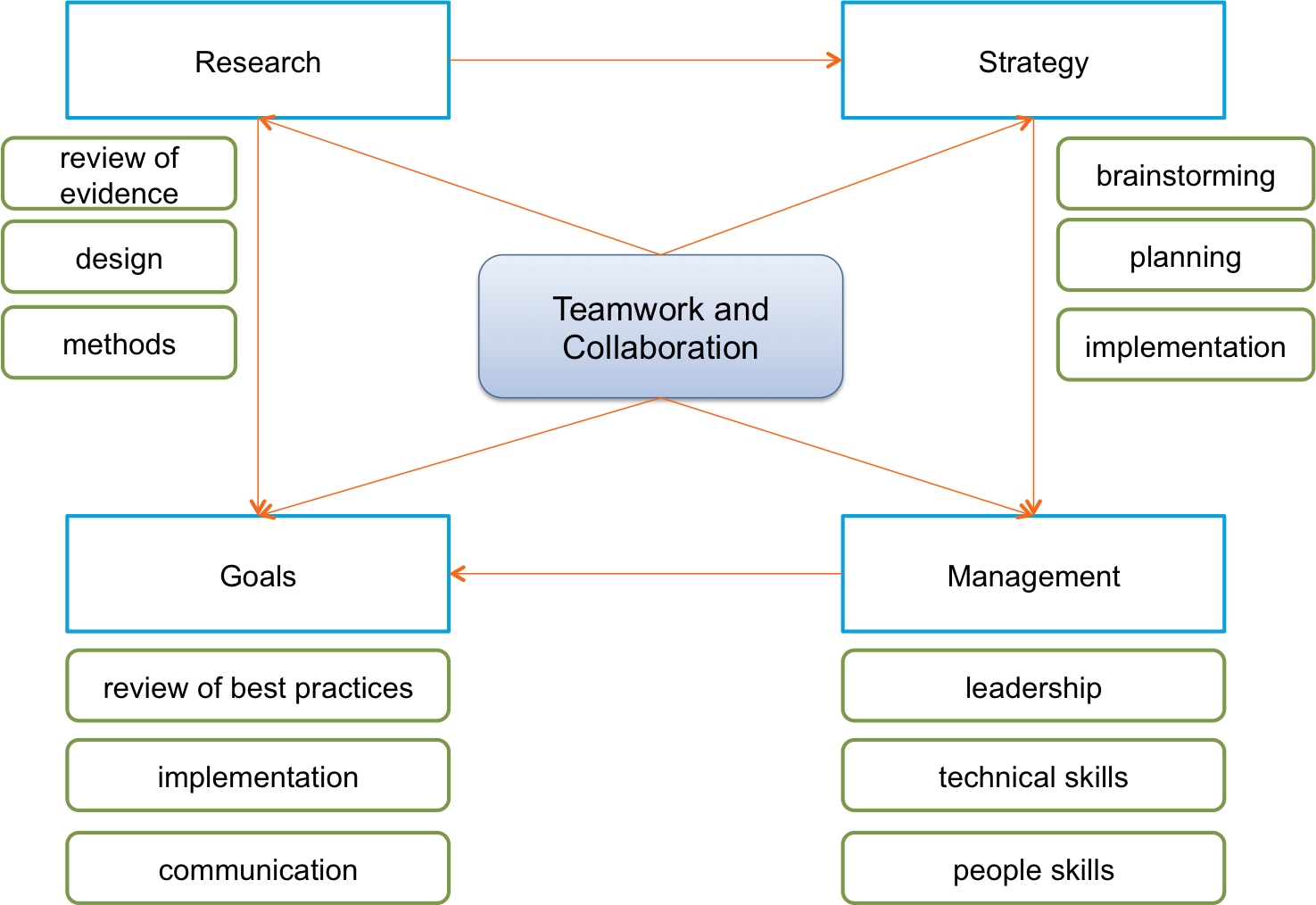
Mind Map
The mind map presented below demonstrates key components of teamwork and collaboration competency as well as how they are interconnected. To effectively implement teamwork and competency in a healthcare setting, research, strategy, management, and the establishment of goals should be included in the operations of the interdisciplinary team.
Blog Posts Stemming from the Original Blog Post
- As it has already been identified, teamwork and collaboration competencies can facilitate the successful implementation of a project of reducing door-to-balloon time. To further examine the topic of teamwork in healthcare, it is worth mentioning the key implications of collaboration in a health facility. First, clinical care is becoming more complex, which forces the medical staff to perform complicated services where collaboration is essential. Second, working together as a group helps decrease the number of clinical errors and increase patient safety (HRH, n.d.). Third, solid communication among team members and their patients contributes to improved health outcomes and patient satisfaction.
- It is important to provide an example of a successful D2B time reduction intervention within the context of teamwork competency implementation. The success of the ACC’s QI Program targeted at reducing the door-to-balloon time and sustaining long-term results was largely attributed to the interdisciplinary team that collaborated beyond the walls of healthcare facilities and included EMS; teams cooperated to determine the best practices for achieving the set goal (ACC, 2016). The team included physicians and non-physicians who were encouraged to share skills and knowledge to decrease D2B time and sustain the improved results long-term.
References
ACC. (2016). Door-to-balloon 10 years later: Successful model sets the stage for the next generation of ACC’s QI programs.
Cronenwett, L., Sherwood, G., & Gelmon, S. (2009). Improving quality and safety education: The QSEN learning collaborative. Nursing Outlook, 57(6), 304-312.
HRH. (n.d.). Why is teamwork in health care important?
Mehta, S., Oliveros, E., Alfonso, C., Falcao, E., Shamshad, F., Flores, A., & Cohen, S. (2009). Optimizing door-to-balloon times for STEMI interventions – Results from the SINCERE database. Journal of the Saudi Heart Association, 21, 229-243.
NLN. (2017). NLN competencies for graduates of nursing programs. Web.
NLN. (2017). Nurse educator core competency. Web.
QSEN. (2014). Competencies.
Sherwood, G., & Zomorodi, M. (2014). A new mindset for quality and safety: the QSEN competencies redefine nurses’ roles in practice. Nephrology Nursing Journal, 41(1), 15-22.