Introduction
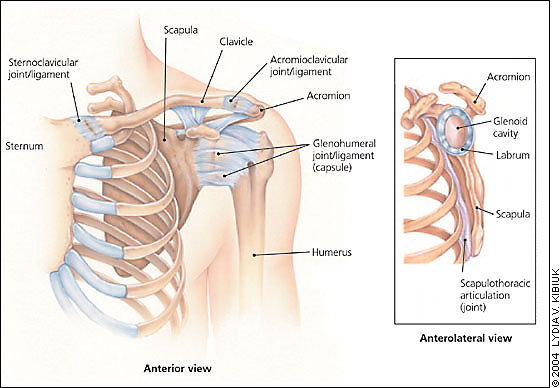
The pectoral girdle or the shoulder girdle is in essence made up of three major bones namely; scapula, clavicle and the proximal humerus and this include the two core joints acromioclavicular joint as well as glenohumeral joint. These features are interrelated in that they link the upper extremities with the thorax and are critically linked to the traumatic injuries which can be defined as dislocations and fractures in any given individual. However, to determine the nature and degree of the damage on the concerned shoulder segment diagnostic radiology is needed for it plays a central role in establishing either the affected area or the cause of the damage .
Radiology is one of the key branches of medical science concerned with medical imaging. This may involve such devices as X-ray machines or other radiation related devices. Radiology also encompasses procedures that do not entail radiation, such as ultrasound or MRI. Basically, as a key medical specialty this discipline touches on two crucial subfields namely diagnostic and therapeutic radiology. Diagnostic radiology is concerned with the dynamics of diverse imaging aspects in diagnosis of diseases. This branch is also divided into various specialties. On the other hand, therapeutic radiology is more employed in treating such ailments as cancer through a form of unique treatment classified as radiation therapy.
Generally, diverse modalities are employed in radiography and they involve plain radiography, magnetic resonance imaging (MRI), nuclear imaging techniques, computed tomography (CT), and ultrasound.
However, these modalities do have their own unique strengths and weaknesses which determine their significance in the course of diagnosis.
From such observation it ought to be noted that shoulder trauma is one of the most common feature allied to the shoulder injuries. These injuries encompass injuries caused by falls onto the shoulder and this may either touch or fracture the clavicle (collar bone) or equally fracture the scapula (shoulder blade). Basically, the shoulder is a composition of three bones namely;
Scapula, clavicle, and the humerus (arm bone). These shoulder bones are boded by supple tissues such as the muscles, tendons, joint capsules and ligaments, to form a suitable domain for the arm to function. Hence, some of the joint found within the shoulder include; Glenohumeral joint, Acromioclavicular joint, and Sternoclavicular joint.
The shoulder sustains one of the key articulations, that is, the relationship concerning scapula and the chest wall. All in all, the shoulder is commonly covered by a number of layers which are classified as soft tissues. The uppermost layer is known as deltoid muscle and this is the layer that gives the shoulder its unique rounded appearance. This layer is essential in that it helps to bring the arm overhead.
Types of shoulder injuries
Shoulder injuries are many and diversified. Fractures, for instance, are broken bones, while dislocations take place or occur when the alternating bones fail to line up. Hence, dislocations entail three core joints, that is: a dislocation of acromioclavicular joint or as commonly known as separated shoulder. Another common injury involves the dislocation of sternoclavicular joint and this regards the interruption of the link touching the clavicle and the sternum (breastbone). The other shoulder related injury involves the dislocation of the glenohumeral joint. This takes place when the joint is dislodged and tends to lean inwardly or outwardly.
Causes
Direct blow to the clavicle or the proximal humerus may result in fracture and this could as a consequence of direct collision, accident or fall. However, scapula fractures are more correlated with injuries of the chest.
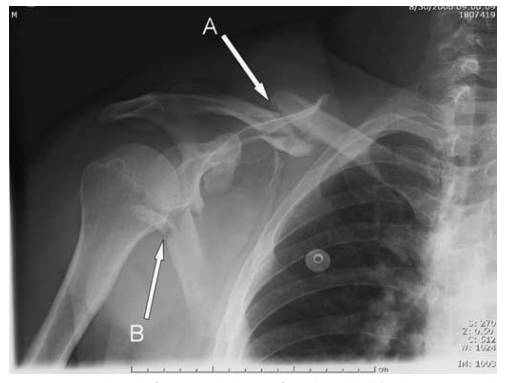
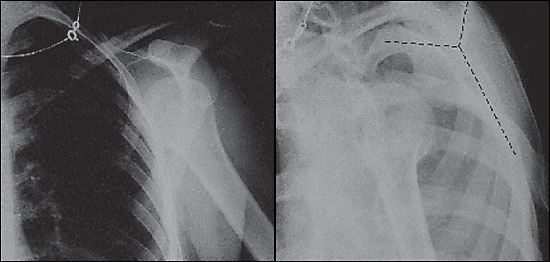
A-clavicle fractures are commonly defined by location and this is done with clavicle being divided into solid thirds: distal, proximal and the middle. B denotes a scapular fracture. As is in the above diagram.
Thus, shoulder trauma can be said to be caused by three elements that is, shoulder dislocation, shoulder separation, and fractures.
Significance of diagnostic radiology
From time to time doctors do use diagnostic radiology in examining body in such way that they cannot do so from the outside observation. Diagnostic radiology involves the use of diverse electronic procedures as well as medical equipments to generate images that expose or reveal what is wrong or is happening inside the patient’s body. Though, a number of the diagnostic tests have been established to be uncomfortable, majority of them are known to be painless and equally noninvasive. More so, the device the doctor opts to use depends with the nature of the patient needs. Some of the commonly preferred tests include MRI, CT , mammography, as well as ultrasound 3. These tests are carried out by radiologists. One of the basic significance of diagnostic radiology lies in its use in detecting any anomalies in the body.
By carrying out molecular imaging doctors are empowered to examine the body from a cellular level and equally pick out the disease before the diseases reaches a critical level. These inclusive tests expose the structures and the function of such features as the shoulder, chest as well as the function of the heart allowing the doctor to detect the abnormalities in the manner they function 4. One of the most typical diagnostic imaging or radiography tests entails digital mammography. This examination does allow the electronic image to be generated in order to determine or reveal existence of any variations regarding the normal and abnormal human tissues. Thus, diagnostic radiography is essential in detecting any changes in the human bone structures.
Analysis
Most of these anomalies are diagnosed by using x-rays as well as carrying out physical examination of the affection area. And this may sometime entail additional imaging procedures such as CT which is necessary. In essence, diagnostic radiology and in particular the plain radiology is the most popular choice in regard to examination of upper extremity.
And this is typically illustrated by the presence of acute shoulder trauma in the upper area of the body. This region harbors the shoulder, wrist, humerus and the forearm which forms a critical diagnostic pattern in detecting any acute fracture. Basically, such imaging procedures as CT, MRI, and ultrasound are not commonly exploited in the course of handling acute trauma, but are essential in dealing with the soft tissue pathology. When dealing with the upper extremity and in particular the shoulder, it would be essential to point out that the major pointer for plain radiography in regard to the shoulder is acute trauma . This is due to the fact that through radiography a number of abnormalities such as fractures of the scapula, humerus, scapula as well as the shoulder dislocation such as glenohumeral or shoulder separation (acromioclavicular) could be detected.
In such a situation most patients may present mixed signs of sub-acute, chronic, or non-traumatic pain, the use of plain radiographic films in such a situation is commonly insignificant. However, where chronic and non traumatic pain is suspected, plain radiographic film is employed to expose if the patient requires either prereduction or postreduction radiography or both.
Diverse studies have established that plain radiographic films used in diagnostic radiology do not show or expose any pathological findings. However, in such a situation most doctors opts to utilize MRI in order to detect any injuries correlated to ligaments such as the rotor cuff which are rarely indicated in the normal setting.
Some of the shoulder injury regards the fracture of the humerus. Humerus as is seen from the following image is the upper segment of the bone linking the shoulder with the elbow. Basically, their exists three major variations of the fractures that can be detected from this diagram;

From this diagram it is evident that there are a number of features allied to the defects spotted on the bone. These include:
- Fractures allied to the upper end of the bone-this anomaly touches both the head as well as the neck of the bone
- Fractures center piece of the bone.
- Fractures tied to the elbow as well as the bone and are commonly referred as supra-condylar fractures. This is due to the fact that they typically occur at the upper or above the condyles. These features are highly likely to affect the juveniles more than adults.
The initial two commonly comes as a consequence of express trauma relating to humerus, that is, a heavy fall or equally a direct collision with a blunt or weighty object. Shaft fractures specifically occur where bending forces are exerted. While supracondylar fractures are collated to the upper transfer of force which breaks affects the lower humerus and this forces the supracondylar to be affected or break. Also these observations touch on the upper humeral fractures. It ought to be noted that these fractures do persistently affect the neck of the concerned bone 9. However, the most essential aspect is to determine whether the fracture concerns dislocation, or is equally in stable position or not. This is due to the fact hat most stable fractures do not require any serious radiography. Also surgery is not commonly needed in such a situation. More or less displaced fractures do in some cases call for reduction that is, pulling under the anesthetic so as to make the bone fragments to be put together.

Exploring the core aspects of diagnostic radiology, it is widely accepted that these injuries are quite painful.
And in some instances they do tend to cause severe damages to the radial nerve. However conservative medication is known to be effectual, but it cannot guarantee that the bones could be fully restored to their normal position.
Summary
Basically, radiographic examination as is allied to the shoulder trauma happens to be one of the most occurring and frequently performed within the medical divisions.
The key objective being to examine the trauma patients, but in some cases it has been established to be providing unreliable and incorrect outcomes. Hence, a radiographic study allied to the shoulder thus requires two or more radiographs and this would entail having dissimilar projections, that is, fore Anteroposterior perspective or view as well as extra projections placed at right angles to each other. The shoulder radiograph of the patient investigated for acute trauma do reveals that the former examination lacked adequate both lateral and oblique view in unear6hing the shoulder fractures and this was due to the fact that they lacked anteroposterior perspective. It ought to be noted that antero-posterior view is the most effective projection in regard to diagnostic radiography, the reason this is seen to be can be allied to the fact that it helped in detecting over 90 % of the suspected injuries.
However, according to the radiographic images acquired it is evident that both the oblique apical as well as the lateral views were not fully sensitive as is with the antero-posterior view which aided in detecting 80% and 75% of the injuries. The glenohumeral dislocations whether with either the fracture including the clavicular fractures were basically exposed through the oblique apical approach, while in the same manner fractures linked to the body as well as the coracoid procedures of the scapula were highly exposed by the lateral view.
This demonstrates that for the diagnostic radiology to be of great value to the patient the radiologist may opt to work hand in hand with the orthopedist so as to make the right decisions in regard to the projections anticipated to be used for each and every patient on the basis of physical examination.
Limitations
Though acute shoulder injuries may be adequately and highly assessed through the use of a standard or average two-view shoulder procedure, posterior dislocation can be subtle or in the same manner hard to detect or diagnose. If posterior dislocation is detected or suspected as per the available examination, physical or the average radiographic as well as extra specialized views which may include both axillary’s as well as oblique view becomes essential. All in all, most of the radiographic views can be adequately acquired even where the concerned patient has a limited or restricted mobility. However, the axillary’s view has been established to require diverse degree of abduction and this may prove to be difficult in some instances.
Conclusion
Diagnostic radiography is paramount in regard to the medical profession. Despite the diverse challenges which have over the time been associated with this practice, diagnostic radiography have proved to be effective in as far as dealing with the trauma of the shoulder is concerned. It ought to be noted that by applying diverse imaging techniques doctors have over the time managed to examine or investigate any fractures or injuries affecting the entire shoulder. According to the available medical evidence it is highly recommended that shoulder dislocations do not necessarily need to be x-rayed before they are put back into place. Radiology does provide a number of benefits for both patients and physicians. It ought to be noted that general radiology such as x-ray do allow the doctors to examine the bones surrounding specific body parts such as the shoulder dislocations in order to make the suitable diagnosis. Also radiology helps in that it allows the concerned doctors to monitor any changes in regard to the changes in injury and equally make the right decision concerning the best way to follow.
Despite the advantages of diagnostic radiology there are also risk factors which are to be considered in the course of dealing with the aspects of imaging. This is due to the fact that unlike any other form of diagnosis radiology id predominantly anchored in the use of radiation, and this indicates that risks linked to exposure do exist. However, the risk of acquiring cancer due to radiology is predominantly low.
Works cited
Banh, Kenny and Hendley, Gregory. Plain Radiography. 2011. Web.
Brant, William and Helms, Antony., Fundamentals of Diagnostic Radiology, 2nd ed, Williams & Wilkins, Baltimore, MD, 1999.
Daffner, Richard. Clinical Radiology: The essentials. Baltimore, MD: Lippincott Williams & Wilkins, 2007.
Greenspan, Andy. Orthopedic Radiology: A Practical Approach, 3rd ed., Lippincott Williams & Wilkins, Philadelphia, PA, 2000
Gunderman, Richard. Clinical presentation, Pathophysiology and imaging. New York, NY: Thieme Medical Publishers, 2000
Herman, Gray. Fundamentals of computerized tomography: Image reconstruction from projection, 2nd edition. Springer, 2009
Kaplan, Patrick and Helms, Antony. Musculoskeletal MRI, Saunders, 2001.
MedlinePlus. Diagnostic Imaging. 2011. Web.
Mehta, Amit and Beall, Douglas. Radiology. Totowa, NJ. Humana Press, 2006
Novelline, Robert. Squire’s Fundamentals of Radiology. Harvard University Press. 5th edition, 1997
Articles and journal used
Broken Collarbone
A broken collarbone (fractured clavicle) is a common injury among two very different groups of people: children and athletes. Many babies are born with collarbones that broke during the passage down the birth canal. A child’s collarbone can easily crack from a direct blow or fall because the collarbone doesn’t completely harden until a person is about 20 years old. An athlete who falls may break the collarbone because the force of the fall is transmitted from the elbow and shoulder to the collarbone.
The collarbone is considered part of the shoulder and helps connect the arm to the body. It lies above several important nerves and blood vessels. However, these vital structures are rarely injured when the collarbone breaks. The collarbone is a long bone, and most breaks occur in the middle section.
Signs of a break:
- Sagging shoulder (down and forward).
- Inability to lift the arm because of pain.
- A grinding sensation if an attempt is made to raise the arm.
- A deformity or “bump” over the fracture site.
- Although a fragment of bone rarely breaks through the skin, it may push the skin into a “tent” formation.
Diagnosis
Although a broken collarbone is usually obvious, your orthopaedist will do a careful examination to make sure that no nerves or blood vessels were damaged. An X-ray is often recommended to pinpoint the location and severity of the break.
Treatment
Most broken collarbones heal well with conservative treatment and surgery is rarely necessary.
- A simple arm sling can usually be used to immobilize the arm. A child may have to wear the sling for 3 to 4 weeks; an adult may have to wear it for 6 to 8 weeks.
- Depending on the location of the break, your physician may apply a figure-of-eight strap to help maintain shoulder position.
- Analgesics such as acetaminophen or nonsteroidal anti-inflammatory medications such as aspirin or ibuprofen will help reduce pain.
- A large bump will develop as part of the healing process. This usually disappears over time, but a small bump may remain.
- Range of motion and strengthening exercises can begin as soon as the pain subsides. However, you should not return to sports activities until full shoulder strength returns.
- In rare cases, depending on the location of the break and the involvement of shoulder ligaments, surgery is needed. Surgery usually gives good results.
Fracture of the Scapula
Triangular, mobile and protected by a complex of surrounding muscles, the shoulder blade (scapula) is rarely broken. Scapula fractures represent less than 1 percent of all broken bones. High-energy, blunt trauma such as a motorcycle or car crash or falling from significant height can fracture the scapula and cause other major injuries such as broken ribs or damage to the head, lungs or spinal cord. Symptoms include:
- Extreme pain when you move the arm.
- Swelling around the back of the shoulder.
- Skin abrasions.
Without treatment, a fractured scapula can result in chronic shoulder pain and disability.
Classification and evaluation
To give you appropriate treatment, your doctor will probably need to take X-rays of your shoulder and chest to describe and classify the location(s) of fracture to the scapula. In some cases, your doctor may also need to use other diagnostic imaging tools such as CT scan (computerized tomography).
One or more parts of the scapula may be fractured:
- Scapular body (50-60 percent of cases).
- Scapular neck (25 percent).
- Glenoid.
- Acromion.
- Coracoid.
Your doctor will evaluate the position and posture of the shoulder and treat any soft tissue damage (i.e., abrasions, open wounds, and muscular trauma). Your doctor may want a detailed neurovascular examination, which may not be possible if you have other severe injuries.
Treatment
Nonsurgical treatment with a simple sling works for most fractures of the scapula. The immobilization devices holds your shoulder in place while the bone heals. In many cases, your doctor may want you to start early range of motion exercises within the first week after the injury. Other fractures may need 2 to 4 weeks of immobilization. Your shoulder may feel stiff when the doctor removes the sling. Begin limited active use of your shoulder immediately. Continue passive stretching exercises until complete shoulder motion returns. This may take 6 months to a year.
If you have an isolated scapular body fracture, your doctor may want you to stay in the hospital. Certain types of scapular fractures may need further evaluation:
- Fractures of the glenoid articular surface (shoulder joint) in which bone has moved out of place (displaced) significantly.
- Fractures of the neck of the scapula with severe angular deformity.
- Fractures of the acromion process with impingement syndrome.
In these cases, you may need surgery in which the doctor uses plates and screws to hold together the bone.
Acute Shoulder Injuries
DAVID M. QUILLEN, M.D., MARK WUCHNER, M.D., and ROBERT L. HATCH, M.D., M.P.H., University of Florida School of Medicine, Gainesville, Florida Am Fam Physician. 2004 Nov 15;70(10):1947-1954.
The shoulder is the most mobile joint in the human body. The cost of such versatility is an increased risk of injury. It is important that family physicians understand the anatomy of the shoulder, mechanisms of injury, typical physical and radiologic findings, approach to management of injuries, and indications for referral. Clavicle fractures are among the most common acute shoulder injuries, and more than 80 percent of them can be managed conservatively. Humeral head fractures are less common and usually occur in elderly persons; 85 percent of them can be managed nonoperatively. Common acute soft tissue injuries include shoulder dislocations, rotator cuff tears, and acromioclavicular sprains. Acromioclavicular injuries are graded from types I to VI. Types I and II are treated conservatively, types IV to VI are treated surgically, and there is debate about the best approach for type III. Eighty percent of shoulder dislocations are anterior. Diagnosis of this injury is straightforward. The injury usually can be reduced by employing a number of nonsurgical techniques. Traumatic or acute rotator cuff tears can be managed conservatively or surgically, depending on the patient and the degree of injury.
Strength of Recommendations
The shoulder includes the proximal humerus, the clavicle and the scapula, and their connections to each other, to the sternum (clavicle), and to the thoracic rib cage (scapula). Together, these elements form the most mobile joint in the human body (Figure 1). It allows the upper extremity to rotate up to 180 degrees in three different planes, enabling the arm to perform a versatile range of activities. This mobility comes at a cost: it leaves the shoulder prone to injury. Family physicians often encounter patients with shoulder injuries. It is important to understand the anatomy of the shoulder, mechanisms of injury, evaluation and management of injuries, and indications for referral.
Clavicle Fractures
The only bony connection between the axial skeleton and the upper extremity occurs through the clavicle, which is held securely in place by ligaments at the sternum and acromion. The clavicle overlies and protects the brachial plexus, pleural cap, and great vessels of the upper extremity. Clavicle fractures are among the most common injuries, accounting for one in 20 adult fractures.1 The injury usually is caused by a fall on the lateral shoulder or, less commonly, by a direct blow or by falling on an outstretched arm.
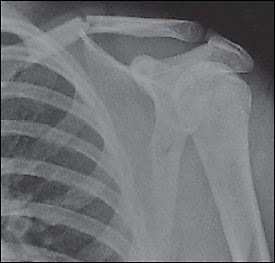
The clavicle is relatively superficial and easily palpable along its entire length. Clavicle fractures usually can be diagnosed by careful inspection and palpation. Acute complications are uncommon, although pneumothorax, hemothorax, and injuries to the brachial plexus or subclavian vessels have been reported.2 Neurovascular and lung examinations should be performed to screen for these complications. A routine anteroposterior view usually is the only radiograph needed to confirm the fracture and specify its location. Nondisplaced fractures, however, may be difficult to detect on an anteroposterior view, particularly in children. In such cases, a 20-degree (Zanca view) or 45-degree cephalic tilt view usually demonstrates the fracture.
Clavicle fractures are classified by Allman1 into three groups by dividing the clavicle into thirds. Group 1 (middle one third of the clavicle) is the most common type of break (Figure 2)3 and represents 80 percent of clavicle fractures.1 Group 1 fractures are treated conservatively with an arm sling for comfort, even if significant displacement is present. Historically, a figure-of-eight bandage was applied, but they are uncomfortable, have a higher incidence of complications, and do not improve functional or cosmetic results.4 Ice and analgesics are helpful in the initial treatment. Elbow range-of-motion exercises should be started as soon as pain permits. Shoulder range-of-motion and strengthening exercises should begin once the fracture heals.
Nondisplaced group 2 (lateral one third of the clavicle) fractures usually can be treated conservatively. Group 2 fractures that extend to the articular surface, even if nondisplaced, often lead to osteoarthritis of the acromioclavicular (AC) joint.5 Displaced group 2 fractures generally require operative treatment because they are unstable and have a high incidence of nonunion. Surgical treatment generally results in good function.6
Displaced group 3 fractures (medial one third of the clavicle) and sternoclavicular dislocations require orthopedic referral. These injuries have a fairly high rate of significant intrathoracic or neurovascular injury that may require emergency surgery. Nondisplaced group 3 fractures without associated injuries can be treated conservatively with a sling for comfort.
Proximal Humerus Fractures
Proximal humerus fractures occur most commonly in elderly persons. They usually result from a fall onto an outstretched arm. In young adults, direct blows are a more common cause. Up to 85 percent of proximal humerus fractures can be treated nonoperatively.2 Evaluation of a patient with a proximal humerus fracture starts with a careful and focused physical examination. Neurologic and vascular examinations of the upper extremity should be completed and documented. Occasionally, the axillary nerve or axillary artery may be injured; rarely, the brachial artery, brachial plexus, or another nerve may be injured. Identification of an anterior or posterior bulge may suggest a dislocation. Tenderness and swelling often are diffuse, making it difficult to detect clear point tenderness.
Appropriate radiographs are an important part of diagnosing and evaluating proximal humerus fractures. A standard shoulder series includes anteroposterior, transscapular (Y—Figure 3), and axillary views.3 Instead of a true shoulder series, radiologic technicians sometimes obtain only internal and external rotation views of the humerus. Although these views may demonstrate the fracture, they are suboptimal for detecting associated fractures and shoulder dislocations.
Because of its bony structure and the insertion of the rotator cuff tendons, the proximal head of the humerus generally fractures with four predictable cleavage lines (Figure 4).3 Regardless of the number of fragments, proximal humerus fractures are classified by the displacement and degree of angulation.7 Neer 1-part fractures have no more than 1-cm displacement of any fragment and no more than 45 degrees of angulation. More than 80 percent7 of proximal humerus fractures are nondisplaced (i.e., Neer 1-part fractures) and can be treated conservatively, if stable.2 Open fractures and fractures with neurologic or vascular deficits require emergent orthopedic referral. Patients with displaced proximal humerus fractures should be referred because surgical intervention appears to improve the outcome.8 Fracture-dislocations and fractures of the anatomic neck (indicated by the line just below the humeral head in (Figure 4)3 also should be referred.
Treatment of Neer 1-part fractures includes a sling for comfort and early range-of-motion exercises, which should be started as soon as tolerated (about five to 10 days after the injury). Patients should begin with pendulum exercises with the injured arm in the sling. They perform this movement by bending at the waist, allowing the arm to fall toward the floor, and rotating it in a circle. With time, the size of the circle is increased, and the sling is removed during the exercise.
After two to three weeks, abduction (progressively walking fingers up the wall) and internal rotation (first touching hip, then progressing to mid-back) exercises are added. Elderly patients tend to lose elbow range of motion rapidly. To avoid this, patients should be encouraged to remove the sling and flex and extend the elbow as soon as this movement can be tolerated. To speed recovery and avoid iatrogenic loss of elbow range of motion, use of the sling should be discontinued completely by four to six weeks after injury. Formal physical therapy can be helpful in maximizing future function of the shoulder.
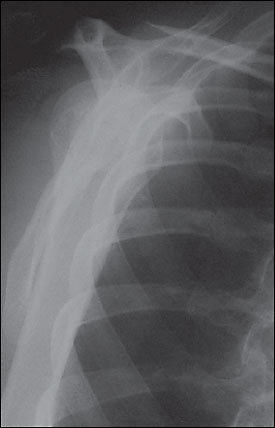
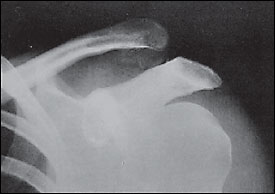
Glenohumeral Dislocation
The glenohumeral joint is one of the most commonly dislocated joints. Ninety percent of shoulder dislocations are anterior (Figure 5),3 with most of the others being posterior.9 Inferior dislocations (luxatio erecta) are rare and often are accompanied by neurovascular injury and fracture. In younger patients, most shoulder dislocations are caused by direct trauma and sports injuries. In elderly persons, falls are the predominant cause, and the dislocation often is accompanied by a fracture. An excessive external rotation or abduction force usually causes anterior dislocations, while posterior dislocations usually occur when the humeral head is driven posteriorly with great force.
Patients with shoulder dislocations typically are unwilling to move the affected arm and tend to cradle it with the other arm. The diagnosis of an anterior dislocation often is suggested by simple inspection. A bulge may be noticeable where the humeral head rests, with emptiness beneath the acromion where the humeral head should be.
Management begins with a careful examination to rule out neurologic or vascular deficits. The standard three-view shoulder series should be obtained to ascertain or confirm the diagnosis and to rule out associated fractures. Muscle spasm sets in shortly after dislocation, making reduction more difficult. Therefore, reduction should be performed promptly after radiographs are obtained and interpreted. When evaluating patients in the field (e.g., at a sports event), many physicians perform the reduction before obtaining radiographs. This step provides prompt, dramatic relief from pain. Early reduction also requires less force, which should reduce the risk of iatrogenic injury. These benefits should offset the disadvantages of delaying radiographs. This is particularly true for recurrent dislocations, which are much less likely to have associated fractures. Radiographs should be obtained after reduction to rule out associated fractures that might demand specific treatment. In patients with chronic dislocations, radiographs may not be necessary.
Numerous reduction techniques are available.10 There is the self-reduction technique,11 in which the patient interlaces his or her fingers and places them around the flexed ipsilateral knee. The patient then leans backward, and the reduction occurs. This technique is similar mechanically to the traction against countertraction method (called the hippocratic method if done by a single physician). In this method, the physician grasps the patient’s affected arm by the wrist and applies traction at a 45-degree angle, while providing countertraction by placing a foot on the patient’s chest wall or by having an assistant wrap a sheet around the patient’s torso.
In the gravity method (modified Stimson’s method), the patient is placed prone with the affected shoulder supported and the arm hanging over the examination table with a weight attached to the hand. A weight of 2.25 kg (5 lb) usually is sufficient, but greater weight may be needed for larger or more muscular patients. Gravity slowly stretches the spasmed muscles, and the reduction occurs. Unless performed immediately after injury (on the field or by using self-reduction), all of these methods require significant analgesia, such as a narcotic plus benzodiazepine, with appropriate monitoring. Failure to reduce the dislocation successfully using these methods necessitates reduction under general anesthesia.
Treatment after reduction traditionally includes immobilization of the shoulder for four weeks followed by rehabilitation. The possible drawback of conservative treatment is a high incidence of recurrent dislocation (67 to 97 percent), with patients younger than 30 years being at highest risk.11 Multiple studies have shown that early surgical intervention, rather than conservative treatment (especially in the younger athletic population), provides a better outcome.12–15 Unfortunately, anterior shoulder dislocations generate a variety of injuries, making any general intervention recommendations inappropriate. The choice of surgical treatment depends on the soft tissue injury. Referral to an orthopedist is probably a good choice, particularly for younger or athletic patients. If conservative therapy is pursued, range of motion should be addressed in the same way as it is in patients with a humerus fracture. As range of motion improves, strengthening exercises should be added.
Acromioclavicular Sprains
The AC joint is a common site of injury in athletes and active persons. The classic cause of an AC joint injury is a direct blow to the acromion with the humerus in an adducted position. This force drives the acromion medially and inferiorly. AC joint injuries also may be caused by indirect trauma, such as falling on an outstretched arm or elbow. The ligaments that hold the AC joint together include the acromioclavicular, coracoclavicular, and deltotrapezial fascia. These ligaments can be sprained, disrupted, detached, or separated, depending on the severity of the injury.
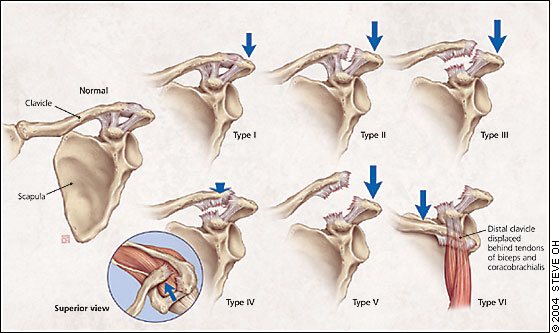
The first ligament to be damaged is the AC ligament. With enough force, the coracoclavicular ligaments also will be torn, and the deltotrapezial fascia injured or detached. When all support is disrupted or detached, the distal clavicle loses all ligamentous connection, allowing it to rise superiorly. Associated fractures of the coracoid process or the lateral one third of the clavicle may occur, necessitating an orthopedic referral. The Rockwood classification for AC joint injuries includes six categories (Figure 6), depending on which ligaments were damaged and the position of the clavicle.
Patients with AC joint injuries should receive a physical examination and evaluation for radiographs. As with all acute injuries, neurovascular assessment should be included. If radiographs are obtained, the uninjured side also should be imaged for comparison. Weighted radiographs have been a part of the traditional work-up, but the need for them has come into question.16 Patients with type I injuries should have tenderness over the AC joint, no visible deformity of the distal clavicle, and normal radiographs. They also will have a positive cross-arm test (sharp pain at the AC joint if the patient holds the arm out straight and brings it across the chest).
With type II injuries, the distal clavicle may be slightly more prominent on inspection, and the patient may have pain at the distal end of the clavicle from the sprained coracoclavicular ligament. Radiographs usually are normal but may show slight widening of the AC joint. Type III injuries usually present with obvious visible prominence of the distal clavicle. Radiographs (Figure 7) should demonstrate an obvious separation of the AC joint and an increase of the coracoclavicular distance of 25 to 100 percent compared with the normal side.17 Types IV to VI have grossly abnormal radiographs, and patients with these injuries should be referred immediately.
There is a general consensus that type I and II injuries are treated nonoperatively, while types IV, V, and VI are treated surgically. The treatment of type III injuries remains an area of controversy, and patients with these injuries should be referred to an orthopedist for evaluation and possible surgical repair.
Treatment of type I and II injuries focuses on symptomatic relief and includes use of a sling for one to three weeks, ice, and nonsteroidal anti-inflammatory drugs (NSAIDs). Once the acute pain is alleviated, range-of-motion and general strengthening exercises are started. Athletes may return to sports when pain-free function is restored. Most patients are able to return to sports, but some may complain of nuisance symptoms such as clicking and pain with push-ups. Nonoperative treatment of type III injuries is similar to that for types I and II, except that rest in a sling lasts for two to four weeks.
Rotator Cuff Tears
The rotator cuff comprises four muscles, the supraspinatus, infraspinatus, teres minor, and subscapularis (Figure 8). The rotator cuff is the support structure for the shoulder joint. When a tear occurs, patients experience pain and difficulty in abducting or rotating the arm. The incidence of traumatic rotator cuff tears is unknown,18 but it is thought to be relatively uncommon in younger athletes. Rotator cuff tears cover a spectrum of injuries. At one end are relatively high-force injuries to a healthy rotator cuff that typically produce full-thickness tears. The degree of trauma usually required would be a significant fall, motor vehicle crash, or shoulder dislocation. Lesser degrees of trauma can cause partial-thickness tears. On the other end of the spectrum are overuse injuries. Traumatic rotator cuff tears can occur at any age. Overuse injuries generally occur in athletes and increase in frequency with advancing age.19
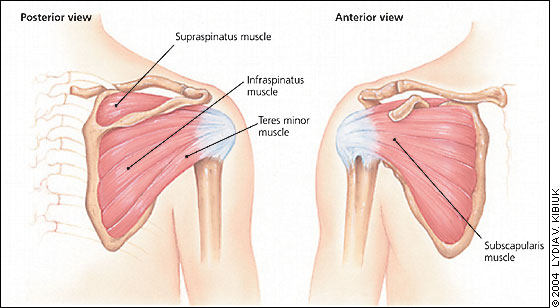
The diagnosis of an acute rotator cuff tear is based on the history of the injury, the physical examination findings, and magnetic resonance imaging (MRI) when necessary. Pain and weakness usually are made worse by overhead activities and are present in abduction and external rotation. MRI has become the imaging standard and has replaced invasive arthrography to assist in the diagnosis.20
Initially, conservative treatment is acceptable for rotator cuff tears, but the choice of an operative versus nonoperative approach should be individualized for each patient. Young active patients with acute full-thickness tears and severe functional deficit should be referred quickly to an orthopedic surgeon for possible operative repair.19 Competitive athletes generally do better with surgical repair, no matter what their age.13 A Cochrane review of surgical, nonsurgical, conservative, and pharmaceutical (oral and injection) treatments for rotator cuff tears provides little evidence to suggest which treatment course is best.21
Conservative treatment starts with relative rest and restriction of movement; in particular, limiting the possibility of repeating the initial injury by avoiding athletic activities. The rest period should be short (one to two weeks) and should include icing, NSAIDs, and, occasionally, subacromial steroid injections. Gentle range-of-motion exercises (pendulum exercises) should be initiated during the rest period to retard loss of range of motion. After the pain has subsided, a monitored stretching and strengthening program should be started. This program should be supervised by a physical therapist or a sports trainer with substantial knowledge of shoulder rehabilitation.
The success rate of conservative treatment is unclear.19 There are concerns that delaying repair of a rotator cuff tear makes the eventual repair harder or impossible, and that initial surgical repair generally has a good outcome.13 The choice of treatment is clearly an individual one that should be made with input from the patient.
The Authors
DAVID M. QUILLEN, M.D., is assistant professor in the Department of Community Health and Family Medicine at the University of Florida School of Medicine, Gainesville. He received his medical training at the University of North Carolina at Chapel Hill, and completed a family medicine residency and a faculty development fellowship at Duke University School of Medicine, Durham, N.C.
MARK WUCHNER, M.D., is chief resident in the Department of Community Health and Family Medicine at the University of Florida School of Medicine in Gainesville. He received his medical degree from the Universidad Autonoma de Guadalajara, Guadalajara, Mexico, and completed a one-year externship through the New York Medical College, Valhalla, N.Y.
ROBERT L. HATCH, M.D., M.P.H. is associate professor in the Department of Community Health and Family Medicine at the University of Florida School of Medicine in Gainesville. He received his medical and master of public health degrees from David Geffen School of Medicine, University of California, Los Angeles, and completed a family medicine residency and a faculty development fellowship at the Medical College of Virginia School of Medicine in Charlottesville.
Address correspondence to David M. Quillen, M.D., Dept. of Community Health and Family Medicine, University of Florida Health Science Center, P.O. Box 103588, Gainesville, FL 32610-3588 (e-mail: [email protected]). Reprints are not available from the authors.
The authors indicate that they do not have any conflicts of interests. Sources of funding: none reported.
Figure 7 was provided by Robert L. Hatch, M.D., M.P.H.
References
Allman FL Jr. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg [Am]. 1967;49:774–84.
McKoy BE, Bensen CV, Hartsock LA. Fractures about the shoulder: conservative management. Orthop Clin North Am. 2000;31:205–16.
Eiff MP, Hatch RL, Calmbach WL. Fracture management for primary care. 2d ed. Philadelphia: Saunders, 2003.
Andersen K, Jensen PO, Lauritzen J. Treatment of clavicular fractures. Figure-of-eight bandage versus a simple sling. Acta Orthop Scand. 1987;58:71–4.
Clarke HD, McCann PD. Acromioclavicular joint injuries. Orthop Clin North Am. 2000;31:177–87.
Webber MC, Haines JF. The treatment of lateral clavicle fractures. Injury. 2000;31:175–9.
Craig EV. Fractures of the clavicle. In: Rockwood CA, Green DP, eds. Rockwood and Green’s Fractures in adults. 4th ed. Philadelphia: Lippincott-Raven, 1996:1116.
Misra A, Kapur R, Maffulli N. Complex proximal humeral fractures in adults—a systematic review of management. Injury. 2001;32:363–72.
Blake R, Hoffman J. Emergency department evaluation and treatment of the shoulder and humerus. Emerg Med Clin North Am. 1999;17:859–76.,vi.
Rockwood CA Jr, Wirth MA. In: Rockwood CA Jr, Green DP, eds. Rockwood and Green’s Fractures in adults. 4th ed. Philadelphia: Lippincott-Raven, 1996:1247–51.
Burra G, Andrews JR. Acute shoulder and elbow dislocations in the athlete. Orthop Clin North Am. 2002;33:479–95.
Davy AR, Drew SJ. Management of shoulder dislocation—are we doing enough to reduce the risk of recurrence?. Injury. 2002;33:775–9.
DeBerardino TM, Arciero RA, Taylor DC, Uhorchak JM. Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes. Two- to five-year follow-up. Am J Sports Med. 2001;29:586–92.
Bottoni CR, Wilckens JH, DeBerardino TM, D’Alleyrand JC, Rooney RC, Harpstrite JK, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576–80.
Larrain MV, Botto GJ, Montenegro HJ, Mauas DM. Arthroscopic repair of acute traumatic anterior shoulder dislocation in young athletes. Arthroscopy. 2001;17:373–7.
Yap JJ, Curl LA, Kvitne RS, McFarland EG. The value of weighted views of the acromioclavicular joint. Results of a survey. Am J Sports Med. 1999;27:806–9.
Garretson RB 3d, Williams GR Jr. Clinical evaluation of injuries to the acromioclavicular and sternoclavicular joints. Clin Sports Med. 2003;22:239–54.
Brunelli MP, Gill TJ. Fractures and tendon injuries of the athletic shoulder. Orthop Clin North Am. 2002;33:497–508.
Mantone JK, Burkhead WZ Jr, Noonan J Jr. Nonoperative treatment of rotator cuff tears. Orthop Clin North Am. 2000;31:295–311.
Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg [Am]. 1991;73:17–29.
Ejnisman B, Andreoli CV, Soares BG, Fallopa F, Peccin MS, Abdalla RJ, et al. Interventions for tears of the rotator cuff in adults. Cochrane Database Syst Rev. 2004;(2):CD002758.
Plain Radiography of the Upper Extremity in Adults
Kenny Banh and Gregory W. Hendey
Plain radiography remains the imaging study of choice for most applications in the upper extremity. Far and away, the most common indication for plain radiography in the upper extremity is acute trauma. The shoulder, humerus, elbow, forearm, wrist, and hand are common radiographic series that are useful in diagnosing an acute fracture. Other imaging modalities such as CT, ultrasound, and MRI are not generally indicated in acute trauma, but have an important role in diagnosing soft tissue pathology.
Another common indication for plain radiography of the upper extremity is the search for a foreign body in a wound. Plain films are an excellent modality for the detection of common, dense foreign bodies encountered in wounds, such as glass and rock, but they are much less sensitive in the detection of plastic or organic materials (1). Other imaging modalities such as CT, ultrasound, and MRI are superior for the detection of organic and plastic foreign bodies (2). The principles of using plain films for foreign body detection are similar regardless of the location in the body and are not discussed in further detail here.
In this chapter, the upper extremity is divided into three sections:
- the shoulder,
- the elbow and forearm,
- the wrist and hand.
Within each section, the indications, diagnostic capabilities, and pitfalls are discussed, followed by images of important pathological findings.
The Shoulder
Indications
The main indication for plain radiography of the shoulder is acute trauma. There are a number of acute injuries that may be discovered on plain radiography after acute trauma, including fractures of the clavicle, scapula, and humerus, as well as shoulder (glenohumeral) dislocation or acromioclavicular (AC) separation. Although many patients may present with subacute or chronic nontraumatic pain, the utility of plain films in that setting is extremely low. In the setting of chronic, nontraumatic shoulder pain, plain films may reveal changes con- Anterior Shoulder. A = Acromion, B = Clavicle, C = Coracoid process, D = Neck of scapula, E = Scapular notch, F = Greater tuberosity, G = Anatomical neck, H = Surgical neck sistent with calcific tendonitis or degenerative arthritis, but it is not necessary to diagnose such conditions in the emergency setting.
Several studies have focused on the issue of whether all patients with shoulder dislocation require both prereduction and postreduction radiographs (3). Some support an approach of selective radiography, ordering prereduction films for first time dislocations and those with a blunt traumatic mechanism of injury, and postreduction films for those with a fracture dislocation. It is also important to order radiographs whenever the physician is uncertain of joint position, whether dislocated or reduced. Therefore, it may be appropriate to manage a patient with a recurrent dislocation by an atraumatic mechanism with out any radiographs, when the physician is clinically certain of the dislocation and the reduction.
Diagnostic Capabilities
In most settings, if the plain films do not reveal a pathological finding, no further imaging is necessary. MRI is an important modality in diagnosing ligamentous injury (e.g., rotator cuff tear), but is rarely indicated in the emergency setting.
With the possible exception of the scapula, most fractures of the shoulder girdle are readily apparent on standard plain films, without the need for specialized views or advanced imaging. The shoulder is no exception to the general rule of plain films that at least two views are necessary for adequate evaluation. The two most common views in a “shoulder series” include the anteroposterior (AP) and the lateral or “Y” scapula view. Other views that are sometimes helpful include the axillary and apical oblique views. In the axillary view, the film cassette is placed superior to the shoulder and the beam is directed up into the axilla, with the humerus in a slightly abducted position. In the apical oblique, the cassette is posterior to the shoulder and the beam is directed from a position 45 degrees superior to the shoulder. The point of both additional views is to enhance visualization of the glenoid and its articulation with the humeral head. These views may be particularly helpful in diagnosing a posterior shoulder dislocation or a subtle glenoid fracture.
Another specific radiographic series that is sometimes used is the AC view with and without weights. Although the intent of these views is to augment the physician’s ability to diagnose an AC shoulder” and can be classified as grade 1 (AC ligament and cora-coclavicular [CC] ligaments intact, radiographically normal), grade 2 (AC ligament disrupted, CC ligament intact), or grade 3 (both liga- ments disrupted, resulting in a separation of the acromion and clavicle greater than half the width of the clavicle). separation, they are not recommended for the following reasons:
- the views might occasionally distinguish a second from a first degree separation, but that difference has little clinical relevance because both are treated conservatively;
- third-degree AC separations are usually obvious clinically and radiographically, without the need for weights or additional views.
Imaging Pitfalls/Limitations
Although most acute shoulder injuries may be adequately evaluated using a standard two-view shoulder series, posterior shoulder dislocation can be surprisingly subtle and is notoriously difficult to diagnose. When posterior dislocation is suspected based on the history, physical, or standard radiographic views, additional specialized views such as the axillary and apical oblique can be very helpful. Most radiographic views of the shoulder may be obtained even when the injured patient has limited mobility, but the axillary view does require some degree of abduction and may be difficult.
Clinical Images
Following are examples of common and important findings in plain radiography of the shoulder:
- Clavicle fracture (fx)
- AC separation
- Anterior shoulder dislocation
- Posterior dislocation (AP)
- Posterior dislocation (lateral scapula)
- Luxatio erecta
- Bankart fx
- Hill-Sachs deformity
- Humeral head fracture
The Elbow and Forearm
Indications
Similar to the shoulder, the most common use of elbow and forearm plain radiography is in the setting of acute trauma. There are numerous fractures and dislocations that can be easily visualized with plain films. Chronic pain in these areas is often secondary to subacute repetitive injuries of the soft tissue such as epicondylitis or bursitis. Many of these soft tissue diseases such as lateral “tennis elbow” and medial “golfer’s elbow” epicondylitis are easily diagnosed on clinical exam and generally require no imaging at all. Plain films may reveal such soft tissue pathologies as foreign bodies and subcutaneous air.
No well-established clinical decision rules exist for the imaging of elbows and forearms in the setting of acute trauma. Patients with full range of flexion-extension and supination-pronation of the elbow and no bony point tenderness rarely have a fracture, and they generally do not require imaging (4). Midshaft forearm fractures are usually clinically apparent, and deformity, swelling, and/or limited range of motion are all indications for obtaining radiographs.
Plain Radiography of the Upper Extremity in Adults
Diagnostic Capabilities
In most cases, if no pathology is found in the plain films of the forearm or elbow, no further imaging is required. Although obvious fractures are easily visualized on plain film, some fractures leave more subtle findings. Radiographs of the elbow in particular may yield important indirect findings. The elbow joint is surrounded by two fat pads, an anterior one lying within the coronoid fossa and a slightly larger posterior fat pad located within the olecranon fossa. In normal circumstances, the posterior fat pad cannot be visualized on plain films, but a traumatic joint effusion may elevate the posterior fat pad enough to be visualized on a 90-degree lateral radiograph. The anterior fat pad is normally visualized as a thin stripe on lateral radiographs, but joint effusions may cause it to bulge out to form a “sail sign” (5). Traumatic joint effusions are sensitive signs of an intraarticular elbow fracture (6).
Imaging Pitfalls/Limitations
The two standard views of the elbow are the AP view and the lateral view with the elbow flexed 90 degrees. The majority of fractures can be identified with these two views, but occasionally supplementary views may be obtained to identify certain parts of the elbow and forearm. The lateral and medial oblique views allow easier identification of their respective epicondylar fractures. The capitellum view is a cephalad-oriented lateral view that exposes the radial head and radiocapitellar articulation. The axial olecranon is shot with a supinated and flexed forearm and isolates the olecranon in a longitudinal plane. Despite these supplementary views, pediatric fractures sometimes reveal no findings on plain radiographs, so a low threshold must be kept to conservatively splint or use more advanced imaging techniques.
Clinical Images
Following are examples of common and important findings in plain radiography of the elbow and forearm:
- Posterior fat pad
- Radiocapitellar line
- Elbow dislocation, posterior
- Monteggia fracture
- Galeazzi fracture (AP)
- Galeazzi fracture (lateral)
The Wrist and Hand
Indications
As with the rest of the upper extremity, the major indication for imaging of the wrist and hand is in the setting of acute trauma. It is one of the most difficult areas to differentiate between soft tissue and skeletal injury on history and physical examination alone. Imaging is necessary even with obvious fractures because the extent of the fracture, displacement, angulation, and articular involvement are important to determine if the patient needs closed reduction in the ED or immediate orthopedic referral for possible open reduction and surgical fixation.
There are still settings where imaging of the hand and wrist is not indicated. Carpal tunnel disease and rheumatologic and gouty disorders are chronic diseases that usually do not involve acute trauma and can be diagnosed based on a good history and physical exam alone.
Diagnostic Capabilities
Besides searching for acute bony fractures and dislocations, plain films can reveal other important pathology. In the setting of highpressure injection injuries to the hand, subcutaneous air is a marker for significant soft tissue injury, and often an indication for surgical exploration. Many carpal dislocations and ligamentous injuries are readily visualized on radiographs of the wrist and hand. Perilunate and lunate dislocations usually result from hyperextension of the wrist and fall on an outstretched hand or “FOOSH” injury. They may be poorly localized on physical exam and films, and a good neurovascular exam, especially of the median nerve, is indicated.
Imaging Pitfalls/Limitations
Because of the size and number of bones, complete radiographic sets of hand and wrist films are often acquired. The minimum standard views of the hand and wrist involve a posterior-anterior, lateral, and pronated oblique. This third view helps assess angulated metacarpal fractures that would normally superimpose on a true lateral. Accessory views of the hand such as the supination oblique or ball catcher’s view can help view fractures at the base of the ring and little finger, while a Brewerton view, which dorsally places the hand down and shoots the film at an ulnar oblique angle, allows better visualization of the metacarpal bases. The wrist accessory films include a scaphoid view, a carpal tunnel view that looks at the hook of the hamate and trapezium ridge, and a supination oblique view that isolates the pisiform. These accessory films should be ordered whenever there is localized tenderness or swelling in these areas.
Unlike the proximal upper extremity, fractures in the wrist and hand may not always be readily apparent on plain films. Scaphoid fractures often result from a FOOSH injury. About 10% to 20% of scaphoid fractures have normal radiographs on initial presentation to the ED. Therefore, it is extremely important to not disregard these clinical signs of scaphoid fracture:
“anatomical snuff box” tenderness, pain with supination against resistance, and pain with axial compression of the thumb. Bones of the Wrist: Palmar View. A = Scaphoid, B = Lunate, C = Triquetrum, D = Pisiform, E = Hamate, F = Capitate, G = Trapezoid, H = Trapezium
More advanced imaging modalities of the wrist and hand such as CT, MRI, and high-resolution ultrasound are much more sensitive for identifying fractures, bone contusions, and ligamentous injury that would be missed on plain radiography.