Abstract
Somatic and dissociative symptoms are associated with the past traumatic experience. Preliminary evidence suggests that their consideration should include a variety of individual factors to provide high-quality treatment to such patients. The importance of this study is conditional upon the fact that the failure to efficiently address these symptoms results in the extended hospital stay, increase in expenses, and inappropriate planning of interventions. Therefore, this paper examines the impact of an individualized approach on the frequency of complications in the specified conditions. For this, 50 female and male adults recruited by linear snowball sampling via social media are asked to fill in the DSM-5: Level 2 – Somatic Symptoms – Adult and DSM-5: Severity of Dissociative Symptoms – Adult questionnaires. The results demonstrated a relatively low frequency of somatic and dissociative symptoms in patients provided with individualized care. These findings highlight the importance of the adoption of this approach by healthcare providers for the provision of high-quality medical services.
Introduction
A traumatic experience is a principal condition, which triggers the emergence of somatic and dissociative symptoms (Luoni, Agosti, Crugnola, Rossi, & Termine, 2018). These issues are typical for most children and adolescents seeking psychiatric attention (Luoni et al., 2018). Moreover, they are frequent in older people and derive from lifetime abuse or similar occasions (Eslami et al., 2019). Such a wide range of various patients suffering from these health problems defines the necessity to examine their situations on the ground of personal characteristics and other specificities. In this case, the generalization would indicate the non-compliance of hospital services with their needs and the neglect of critical circumstances affecting the overall outcome of treatment.
The paper describes the conditions leading to the emergence of somatic and dissociative symptoms. Moreover, it distinguishes the frequency of health issues with such an outcome in patients of different age groups. This initiative is extremely vital for elaborating preventive measures and treatment procedures with regard to the affected persons’ circumstances. The failure to do so would indicate the absence of the required medical assistance for psychiatric patients due to the non-use of an individualized approach. Meanwhile, the negative impact of the specified symptoms on people’s well-being will lead to an extended hospital stay and an increase in expenses. This outcome would be complemented by medical specialists’ inability to adequately plan treatment due to the neglect of medical history, which adds to the necessity to examine these conditions.
Need for an Individualized Approach to Maintain Quality
The experience of patients suffering from somatic and dissociative symptoms varies depending on their personal characteristics and life circumstances. Thus, childhood trauma is the main factor contributing to their development in adolescents, and it increases the chances of exhibiting them in subsequent years (Luoni et al., 2018). As for older adults, especially for women, the emergence of the specified conditions is generally connected to psychological or sexual abuse (Eslami et al., 2019). Nevertheless, these factors are not limited to people’s gender and age.
The previous studies also suggest that there are other aspects of the consideration of somatic and dissociative dysfunctions, which affect the emergence of these issues. They are primarily related to the country of residence and socioeconomic status of persons or their families (Eslami et al., 2019). Hence, it is vital to evaluate each individual case with the inclusion of numerous factors rather than the two most common characteristics, which are gender and age. This step would allow avoiding complications resulting from the improper treatment of the specified health issues.
Extended Hospital Stay and Increase in Expenses
The neglect of individual characteristics alongside other circumstances when planning therapy for psychiatric patients with somatic and dissociative symptoms might result in a prolonged hospital stay and increase their expenses. According to Lyssenko et al. (2018), dissociation is characterized by poorer treatment response and similarity with other conditions, which makes it difficult to distinguish. As for somatic symptoms, the main issue connected to it is a wide range of physical experiences attributed to it (Liu, Zhao, Fan, & Guo, 2019). Therefore, when not assessed properly, these conditions might result in a financial burden and become more time-consuming.
Since there is an apparent resemblance of the health issues under consideration to other psychiatric problems, the optimal way to avoid the complications specified above is to pay particular attention to diagnostics. This decision would also eliminate the risks of the low quality of rendered medical services due to the increased accuracy. In this way, the measures intended to address this aspect would efficiently complement the individualized approach, especially with the inclusion of medical history.
Proper Planning of Treatment with Regard to Medical History
Preparing treatment plans for psychiatric patients should also involve such an aspect of the matter as the previous conditions of a person who needs healthcare specialists’ assistance. Pick, Mellers, and Goldstein (2017) argue that the people who had experience with dissociative seizures and somatic symptoms are more likely to be the ones who also faced posttraumatic stress in the past. Hence, the attention to this area will help in suggesting therapy to them.
The assessment of the medical history of patients with somatic and dissociative symptoms is an efficient method allowing to ensure that they receive the required medical services. It will help plan necessary interventions and contribute to more accurate predictions and demonstrate the connection between prior conditions and the current problems. Thus, it is hypothesized that the use of an individualized approach, together with the consideration of previous health issues and other essential factors, positively correlates with a successful treatment outcome.
Method
Participants
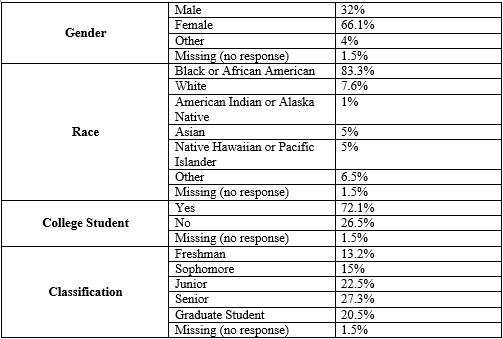
The study implied the participation of 50 female and male patients being treated in the hospital setting (see Table 1). However, the sample was characterized by its diversity since it included representatives of various population groups, both college students and adults (see Table 1). In this way, it helped provide divergent results regarding the impact of personal characteristics on somatic and dissociative dysfunctions and their precondition.
Materials
The instruments used for this purpose included DSM-5: Level 2 – Somatic Symptoms – Adult and DSM-5: Severity of Dissociative Symptoms – Adult measures. The former is designed to assess somatic symptoms and their frequency during the past seven days, and the latter is different only in the orientation on dissociative symptoms. DSM-5: Level 2 – Somatic Symptoms – Adult consists of fifteen questions, and the scores are interpreted with the help of a table with levels of symptom severity from 15 to 45.
DSM-5: Severity of Dissociative Symptoms – Adult measure includes eight items rated on a scale. In this study, the independent variables will be the treatment proposed by the facility and its correspondence to the individualized approach, and the dependent variable will be its outcome for patients. Thus, the procedure will include interviewing, receiving information in specialized forms, and analyzing it as related to the hypothesis.
Procedure
The participants for the study were recruited by linear snowball sampling via social media beneficial for the selected research design since it allows receiving comprehensive qualitative information. Thus, the researchers identified one person suffering from somatic and dissociative symptoms and contacted him on Facebook. He agreed to assist in referring to other people with similar conditions. In this way, the sample was formed from patients who know one another from the medical facility.
Results
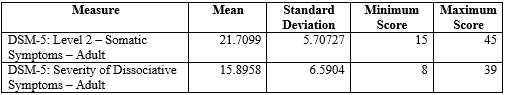
The study reports the relations between somatic and dissociative symptoms statistically significant for their comparison. According to it, the treatment in the hospital setting with the use of an individualized approach indicates their frequency below average for the patients (see Table 2). The mean indicator reflects that the scores corresponding to the issues under consideration, 21.7 out of 45 and 15.89 out of 39, positively correlate with the numbers of events. The standard deviations are 5.7 and 6.6, respectively, and, the correlation is significant at the 0.01 level. Hence, the independent variables, the individualized approach and corresponding treatment, and the dependent variable, its outcome, indicate this method’s efficiency.
Discussion
This study examines the interrelations between an individualized approach to the treatment of somatic and dissociative symptoms and corresponding complications. It demonstrates the correlation between this method and the lower frequency of such events since their average number reflects patient stability and thereby proves the hypothesis. The previous research only allowed for a possibility of the specified interrelations. It is suggested to consider different age groups for precision since the results might differ. This fact presents the study’s limitation but its outcome demonstrates the need to adopt this approach. Thus, the research is important for the provision of high-quality services.
References
Eslami, B., Di Rosa, M., Barros, H., Torres-Gonzalez, F., Stankunas, M., Ioannidi-Kapolou, E., Lindert, J., Soares, J. J. F., Lamura, G., & Melchiorre, M. G. (2019). Lifetime abuse and somatic symptoms among older women and men in Europe. PloS One, 14(8). Web.
Liu, Y., Zhao, J., Fan, X., & Guo, W. (2019). Dysfunction in serotonergic and noradrenergic systems and somatic symptoms in psychiatric disorders. Frontiers in Psychiatry, 10. Web.
Luoni, C., Agosti, M., Crugnola, S., Rossi, G., & Termine, C. (2018). Psychopathology, dissociation and somatic symptoms in adolescents who were exposed to traumatic experiences. Frontiers in Psychology, 9. Web.
Lyssenko, L., Schmahl, C., Bockhacker, L., Vonderlin, R., Bohus, M., & Kleindienst, N. (2018). Dissociation in psychiatric disorders: A meta-analysis of studies using the dissociative experiences scale. American Journal of Psychiatry, 175(1), 37-46. Web.
Pick, S., Mellers, J. D. C., & Goldstein, L. H. (2017). Dissociation in patients with dissociative seizures: Relationships with trauma and seizure symptoms. Psychological Medicine, 47(7), 1215-1229. Web.