The Market Failure
An ideal market assumes fair competition between market participants and the free choice of consumers. The problem is that the healthcare market works in both economic and social fields. Market failures occur, leading to barriers and discrimination in access to medicine. Such failures are the main argument for government intervention when the authorities adjust the market to strike a balance between market interests and the public good.
An example of a market correction is the expansion of the Affordable Care Act. The reason for government intervention was the failure of the market due to barriers to accessing Medicaid for people with incomes below the federal level (Crowley et al., 2019). There were also discriminatory insurance practices for young people who had previously sought health care and racial and ethnic minorities (Crowley et al., 2019). Adopting the law in 2010 was a step towards affordable medicine for all.
Help and Harm Expanding the Affordable Care Act
The document helped poor and middle-income citizens who previously did not have access to insurance. The act expanded Medicaid to anyone with an income below 138 percent of the federal poverty level in the states involved (Campbell & Shore-Sheppard, 2019). Citizens with high incomes are not eligible for subsidies. Until 2019, they were given access to the minimum insurance standard on government exchanges and were encouraged to take advantage of it at the expense of a tax penalty for not having insurance (Campbell & Shore-Sheppard, 2019). For the last three years, no fines have been collected.
The ACA expansion has helped states secure federal funding for healthcare development. A set of measures allowed hospitals to increase revenues significantly (Gruber & Sommers, 2019). In addition, the expansion has reduced the number of uninsured people of color (Campbell & Shore-Sheppard, 2019). However, the law has been criticized for the harm it will cause to market participants. An economic report for President Trump called market failures overvalued and the negative impact of government intervention profound (President Council of Economic Advisers, 2020). Thus, according to the report, private exchanges, market players, and consumers suffered (President Council of Economic Advisers, 2020). State intervention created additional barriers to innovation development, reduced competition, and free choice for consumers.
ACA Unintended Consequences
Government intervention has had evident and unintended health consequences. For instance, the researchers found that the states involved in expanding Medicaid improved consumers’ financial health in several ways, including credit scores, delinquent balances as a percentage of total debt, and the likelihood of new medical collections (Campbell & Shore-Sheppard, 2019). The impact on the labor market has been limited, although people were expected to change jobs more often due to new insurance conditions.
Analysis of Changes Since the ACA Inception
The U.S. healthcare costs are rising every year. This applies both to the personal expenses of citizens and to the costs of the federal and state budgets. In 2020, healthcare spending accelerated its growth rate due to the COVID-19 pandemic (National Center for Health Statistics, 2023). Figure 1 shows the level of healthcare spending since the adoption of the ACA.
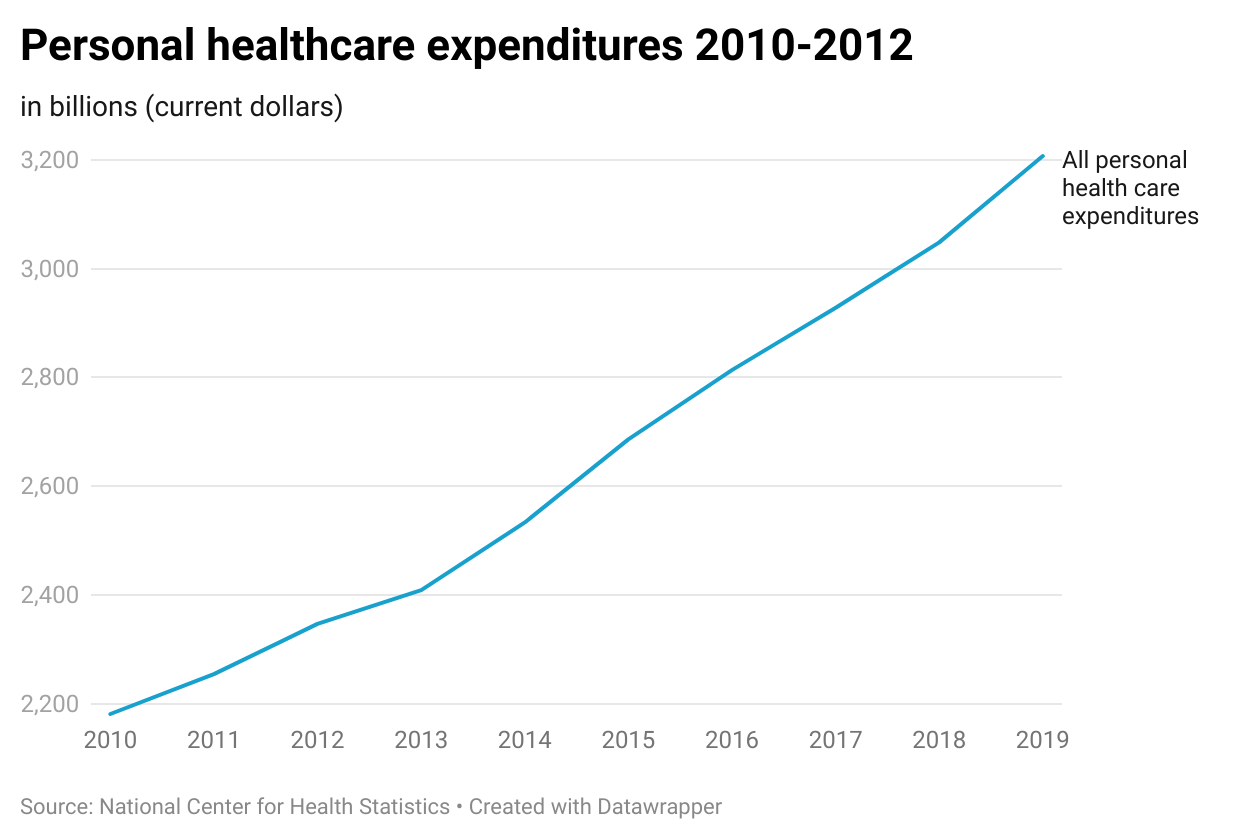
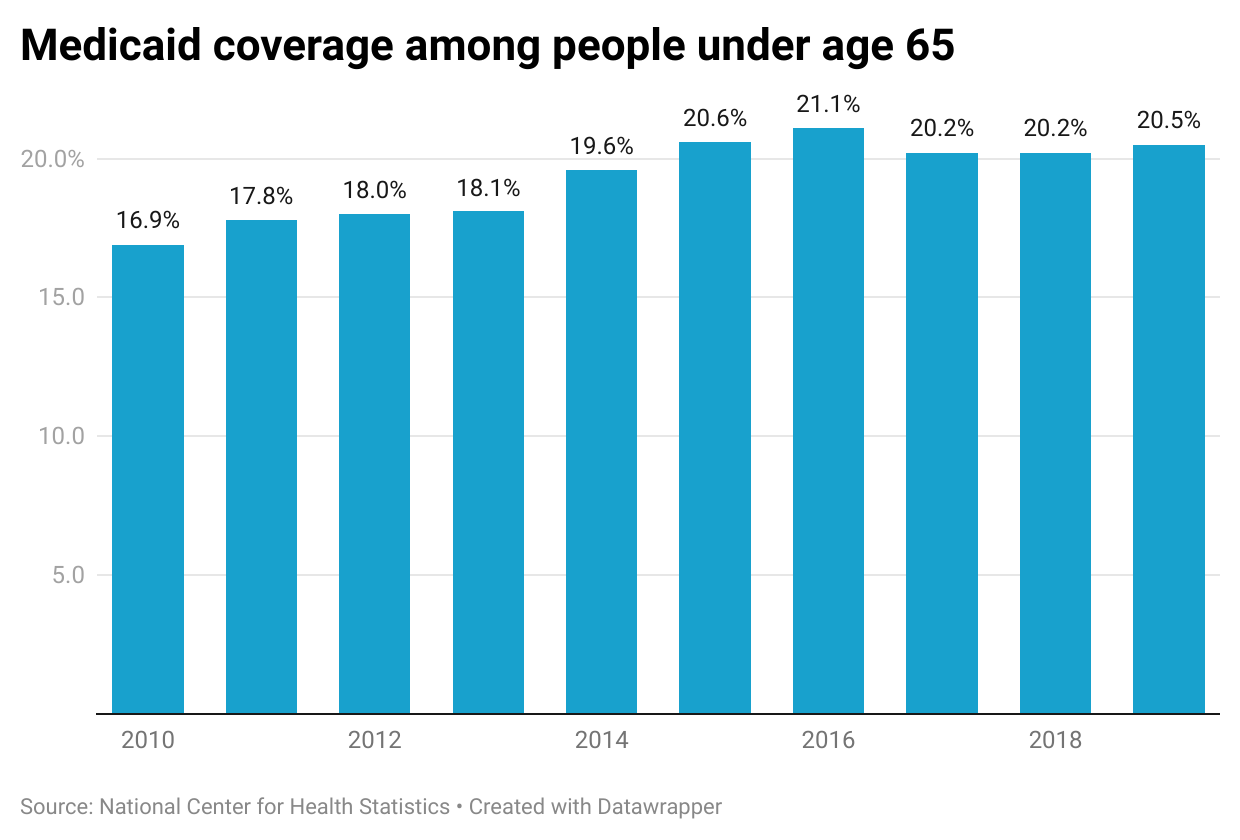
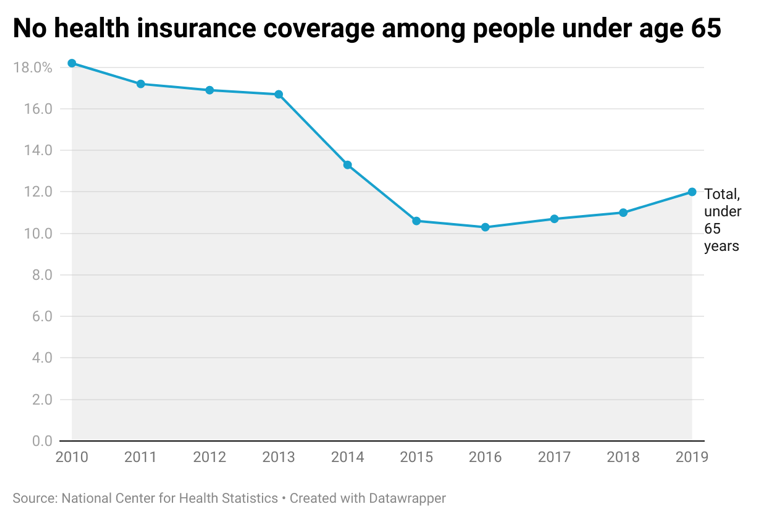
Figure 2 shows the change in Medicaid enrollment from 2010 to 2019. Since its inception and implementation, the population receiving Medicaid has increased from 16.9 to 20.5 percent, with a peak in 2016 of 21.1% (National Center for Health Statistics, 2023). Since 2017, the U.S. has seen a decline in insurance expansion activity due to rates that have remained relatively high. In 2020, many states decided to ease conditions for low-income families, which has improved the situation. By 2021, a quarter of Americans had some form of public insurance in states with Medicaid. In states that did not go for expansion, only one in seven citizens have insurance (National Center for Health Statistics, 2023). Figure 3 shows that the number of people who do not have any health insurance tends to decrease.
Economists’ Opinions
The ACA was passed over ten years ago and has been a primary subject of repeal controversy ever since. Gruber and Sommers (2019) found that most economists (81%) believe that the individual mandate that people pay penalties for refusing insurance is essential to success. ASA did not fully live up to expectations to involve a more working-age population, young people, and national and ethnic participants (Gruber & Sommers, 2019). Baicker et al. argue that the state spends too much on ineffective treatments and does not pay enough attention to innovation (2023). They warn that sweeping tax reforms could devastate the employer-sponsored insurance regime (Baicker et al., 2023). In general, economists recognize the benefits of the ASA and are in favor of further expansion.
Recommendations
As health matters not only for the citizens but also for the state, people should have access to healthcare to prevent severe illness. Further expansion and government intervention will reduce emergency and intensive care expenditures and increase the working age. Healthcare spending should be reviewed to determine the basic package of medical services. It should also be possible to select additional packages. This approach will increase the efficiency of spending and create competitive conditions in the market.
References
Baicker, K., Chandra, A., & Shepard, M. (2023). Achieving universal health insurance coverage in the United States: Addressing market failures or providing a social floor? National Bureau of Economic Research, 1-25. Web.
Campbell, A. L., & Shore-Sheppard, L. (2020). The social, political, and economic effects of the Affordable Care Act: introduction to the issue. RSF: The Russell Sage Foundation Journal of the Social Sciences, 6(2), 1-40. Web.
Crowley, R. A., Bornstein, S. S., & Health and Public Policy Committee of the American College of Physicians (2019). Improving the patient protection and Affordable Care Act’s insurance coverage provisions: A position paper from the American college of physicians. Annals of Internal Medicine, 170(9), 651-653. Web.
Executive Office of the President Council of Economic Advisers (2020). Chapter 4. Enabling choice and competition in healthcare markets. Economic Report of the President, 1-52. Web.
Gruber, J., & Sommers, B. D. (2019). The Affordable Care Act’s Effects on patients, providers, and the economy: What we’ve learned so far. Journal of Policy Analysis and Management, 38(4), 1028-1052. Web.
Maclean, J. C., & Webber, D. (2022). Government regulation and wages: Evidence from continuing coverage mandates. Labour Economics, 78. Web.
National Center for Health Statistics. (2023) Health, United States, 2020–2021: Annual perspective. Hyattsville.