Abstract
Despite reported cases of women undergoing hysterectomy without being sufficiently informed, only three states have enacted informed consent laws aimed at providing more information concerning any alternative treatments. In addition, there exists a deficiency in the study of hysterectomy, which would be required to inform changes in related policies and legislation to improve US healthcare. This study attempts to fill the gaps by exploring the perceptions and experiences of women who underwent hysterectomies in Mississippi in the absence of informed consent law. As its theoretical foundation, the work uses the health belief model to explain the behavioral aspects and beliefs. With its research questions, the paper examines the perceptions of the women, as well as the themes that emerge from their lived experiences. Because the main purpose of the study is to examine the beliefs and attitudes of women in Hinds County, the qualitative research approach guides the process of data collection and analysis.
Interviews were the main data collection technique. The sample included ten women from Hinds County who underwent a hysterectomy and were between 20 and 40 years of age at the time of the research. Demographic data were also collected in order to situate the research. The analysis of the latter data involved descriptive statistics; the interview results were analyzed with the help of thematic analysis. The findings demonstrate that the women who underwent a hysterectomy in the absence of an informed consent law could be subjected to the procedure without sufficient information. As a result, the perceptions and experiences of the majority of the interviewed women were not positive. They described the negative physiological, psychological, and emotional consequences of undergoing hysterectomy without sufficient information; many of them reported feeling deceived by their doctors. Overall, the women expressed the belief that care providers should be required to offer all the pertinent information about hysterectomies and alternative treatments prior to the procedure. The research investigates an under-researched area, and its results highlight the significance of informed consent, which is why it can be used to advocate for the introduction of informed consent laws, promoting the positive social change that would benefit the women of the US.
Acknowledgments
Foremost, my special thanks go to my immediate supervisor for the valuable and constructive suggestions from the planning to completion stages of this study. In particular, the willingness to offer time so generously has been highly appreciated. I would also like to express my deep gratitude to my research supervisors for their patient guidance, enthusiastic encouragement, and useful critiques of this research work. In addition, I would also like to thank the department for continuous advice and assistance in keeping my progress on schedule. I would also like to extend my thanks to the department library assistances for their help in my search for the secondary resources that were helpful in completing my study. Finally, I wish to thank my friends and relatives for their support and encouragement throughout my study
Introduction to the Study
The study focuses on women who have undergone a hysterectomy in Mississippi without comprehensive informed consent. The comprehensive informed consent law aims to provide women with an opportunity to understand the alternatives that are available for hysterectomy. Eysbouts et al. (2017) purported that the patient and surgeon should have shared decision making, which includes an understanding of the procedure, alternatives, potential risks, and complications. A comprehensive informed consent law is a method of ensuring appropriate and adequate patient knowledge with regard to hysterectomy during the decision-making process (Eysbouts et al., 2017). Hysterectomy is a complicated surgical procedure that may result in serious damage to a woman’s reproductive system (Meij & Emanuel, 2016). In some severe cases, fatalities can occur as a result of a hysterectomy (Meij & Emanuel, 2016). The comprehensive informed consent law is aimed at providing women with more information concerning various options for treatment (Burgart et al., 2017). This study is critical in understanding the feelings and experiences of women who have undergone the surgical procedure without the comprehensive informed consent law, not only in Mississippi but also across various states in the United States.
In this chapter, I provide a brief summary of the literature and describe the gap in knowledge on the concerned topic in the background. In addition, this chapter includes the research problem and provides a clear statement that connects the problem addressed and the focus of the study. Finally, the chapter includes the research questions as well as the theoretical or the conceptual framework on which the study is based.
Background of the Study
Clinical problems causing hysterectomy are the women’s major health issue (Meij & Emanuel, 2016). However, cases of hysterectomy are more prevalent among minority women. Researchers have indicated that about 23% of women of Native origin undergo hysterectomy, which is significantly higher than the corresponding rate among non-Hispanic white women (Collins et al., 2014). However, the cases of hysterectomy only minimally can be compared with other procedures for addressing women’s health problems, such as ovarian cancer surgery. Also, researchers have indicated that in the United States, women undergoing the surgical procedure are twice the number in the UK and Sweden (Abdulcadir, Tille, & Petignat, 2017). Further, researchers have indicated that about 25% of women in the United States have undergone surgery due to reproductive complications, such as severe vaginal bleeding, uterine fibroids, and cervical cancer (Abdulcadir et al., 2017). The reasons why women undergo a hysterectomy are diverse, ranging from the relief of pain to the removal of fibroids.
While hysterectomy is not new, it is widely applied without a legal framework for doctors to provide information concerning alternative and safer treatments (Sandberg et al., 2017). Only New York, Washington, and Pennsylvania have established comprehensive consent statutes that act as protection against potential dangers of hysterectomy (Rizk et al., 2014). Most U.S. states lack a policy framework offering physicians an increased opportunity to provide information and enhance the understanding of alternative and safer treatments.
Corona et al. (2015) provided alternative surgical procedures, of which women who undergo a hysterectomy are typically unaware. However, doctors are expected to provide patient education to ensure those female patients have the required knowledge. The comprehensive informed consent law mandates that doctors disclose all information on hysterectomies, including alternative treatment options. The disclosure would provide women with a wide variety of treatment choices (Corona et al., 2015). Using secure procedures can be used to encourage patient education, such as using encrypted emails which contain information about all therapeutic procedures regarding hysterectomy (Tapper et al., 2014).
The purpose of comprehensive informed consent is to authorize the U.S. Department of Health and Human Services (HHS) to issue a pamphlet containing information concerning hysterectomy and other therapeutic alternatives (Eysbouts et al., 2017). However, few studies have been conducted on women who undergo hysterectomy without information in relation to alternative treatments. Therefore, this study will fill the missing data on the study of hysterectomy as it relates to the lack of policy and comprehensive consent statutes that allow medical practitioners to provide information regarding safer treatment alternatives.
Problem Statement
One out of ten women who undergo a hysterectomy may suffer complications arising from the procedure (Eysbouts et al., 2017). Due to the high probability of complications associated with this procedure (approximately 13%), women should only undergo hysterectomies in life-threatening cases like uncontrollable bleeding, complications arising from childbirth, and severe infections (Eysbouts et al., 2017). A significant number of hysterectomy cases recorded in the United States annually are the result of localized illnesses (Eysbouts et al., 2017). Some states have instituted laws aimed at educating women about the potential risks of undergoing hysterectomies. New York has a documented informed consent law that seeks to protect millions of women who are potential candidates of the hysterectomy procedure (Lee, Gurr, & Van Wye, 2017). This study explores the lived experiences of women who have been given the hysterectomy recommendation and undergone the procedure in Mississippi, a state without an instituted comprehensive informed consent law.
Increased complications rates are associated with hysterectomy. In fact, researchers have indicated that a large number of women who undergo the procedure develop postoperative complications (Harris et al., 2017). However, this includes nongeneralizable information. The most common indications for hysterectomy are fibroid-related menorrhagia and uterine bleeding (Harris et al., 2017). Harris et al. (2017) also found that patients with the malignant disease are more likely to develop intraoperative complications compared to patients with benign growths. Postoperative complications are prevalent in abdominal surgery compared with vaginal surgery. Severe uterine complications normally exacerbate the problem (Antero, Shah, Burn, Hallisey, & Greene, 2016). Brown (2017) argued that despite the medical significance to women, hysterectomy is still a controversial issue. Further, Brown observed that the surgical procedure and its role in women’s healthcare are disputed. Despite the effects and advancements in medical practice, the procedural choice of a particular hysterectomy is not normally based on evidence, rather on the personal notion.
Despite the frequency of hysterectomy, 47 states have not enacted consent laws aimed at providing more information concerning various options to the surgical procedure (Meij & Emanuel, 2016). To that end, legal frameworks aimed at educating women concerning the potential safer alternative therapies are lacking. There exists a deficiency in the study of hysterectomy as it relates to the policy and comprehensive consent statutes (Pallett, Phippen, Miller, & Barnett, 2016). As a result, there is a lack of comprehensive informed consent law aimed at providing women with the opportunity to understand the alternatives that are available for hysterectomy.
Previous researchers have focused on issues concerning the consequences of the surgical procedure. Recently, researchers have indicated that the decisions of women undergoing the surgical procedure differ greatly between the states that have enacted the comprehensive informed consent statute and those that lack the law (Lubotzky, 2017; Meij & Emanuel, 2016). Even though the study focuses on the case of Mississippi, the research provides data that will be applied generally in all states that have not enacted the comprehensive informed consent law.
The Purpose of the Study
In this study, I explore the decision-making processes of women in Mississippi who have undergone a hysterectomy in the absence of comprehensive informed consent. In particular, I examine the attitudes and beliefs of women in Hinds County, Mississippi, who have undergone hysterectomy without any comprehensive law concerning their informed consent. Additionally, I identify the perceptions and new ideas emerging from the lived experiences of women who have undergone a hysterectomy in the absence of comprehensive informed consent law. In this study, I utilize the health belief model (HBM) to explain the behavioral aspects of patients based on the principles of individual perceptions. In addition, I primarily apply the phenomenological approach, which is utilized extensively to gather more information concerning individual perceptions through qualitative research methods (John, Malekpour, Parithivel, & Goyal, 2014). Because the main purpose of the study is to examine the beliefs and attitudes of women in Hinds County, the study fully utilizes interviews to gather the information. The interviews focus on the participants’ personal experiences and detailed accounts of the occurrences of women who have undergone a hysterectomy in the absence of comprehensive informed consent.
Research Questions
The following research questions guided this study:
- What are the perceptions of women who have undergone hysterectomy without prior awareness of comprehensive informed consent, which includes other treatment options?
- What are the themes that emerge from the lived experiences of women who have undergone a hysterectomy in the absence of comprehensive informed consent law?
Theoretical Framework
The theoretical framework of this study is based on the HBM. This model was originally developed to explain why patients fail to participate in preventive care and treatment (Rosenstock, 1974). The HBM is one of several behavioral theories that have been used to help explain individual health-related behavior based on several principles. The principles of this model imply an individual’s perception of their ability to manage the disease, their understanding of the magnitude of its effect, and the efforts required to alter their behavior respectively (Lambert, Azuero, Enah, & McMillan, 2017).
The HBM purports that an individual makes decisions regarding health behaviors (surgeries, preventive care, and follow-up treatment) based on perceptions. Adequate patient education aids in making an informed choice regarding health behaviors and is an important part of how the behavior is perceived (Goodman, 2016; Lambert et al., 2017). The HBM will help address the lived experiences of women who have undergone hysterectomies in Mississippi by exploring how the absence of the comprehensive informed consent law affected the participants’ decisions to undergo the surgery. The HBM is useful in answering the research questions and uncovering themes related to the common phenomenon experienced by the subjects.
The theory is based on the principle of individual perception of personal health-related issues. The model asserts that individuals make decisions based on perceived medical care (Corace et al., 2016). According to Huber and Tu-Keefner (2014), HBM has been widely applied in various fields within the health sciences to explain human behavior. The model is useful in answering the research questions and uncovering new areas that relate to the common incidents the participants experienced.
Nature of the Study
This study is qualitative in nature. Qualitative study approaches aim to investigate the interpretation individuals give to a social or human problem (Creswell & Creswell, 2017). Thus, this study is focused on the attitudes and beliefs of women in Hinds County, Mississippi who have undergone hysterectomies without the presence of comprehensive informed consent law. It has been necessary to recruit subjects who have at least a high school diploma (Creswell & Creswell, 2017). In this way, it can be assumed that the subjects have comparable perceptions of informed consent. They are more likely to act similarly in a medical setting. Much attention should be paid to the patients’ abilities to understand informed consent. In particular, one should ask several questions about the legal consequences of signing informed consent documents. This precaution can help the researcher to understand the perceptions and attitudes of respondents. Admittedly, the study may become more time-consuming; nevertheless, by asking these questions, one can gain better insights into the decisions of the patients (Creswell & Creswell, 2017).
The study design approach that best suits the study is the phenomenological approach. Phenomenological approaches are utilized to illuminate and identify phenomena by deciphering how they are viewed by individuals in a situation (Creswell & Creswell, 2017). It is applied in the human sphere to gather deep information and perceptions through qualitative research methods. The methods could be interviews, observations, and discussions among others (Creswell & Creswell, 2017). Specifically, the approach focuses on the study of experiences from the perspective of actors.
Due to its extensive application as a qualitative interview technique in the social and health sciences, this approach would allow the structuring of interviews with predetermined questions (Creswell & Creswell, 2017). A comprehensive interview protocol is administered to the study participants selected from members of a support group in Hinds County, Mississippi. The questions that are used to obtain crucial data are designed and administered with the help of face-to-face interviews. The interview questions were designed based on the reviewed research findings related to the topic and were intended to cover the prevailing identified themes and knowledge gaps including the awareness of alternatives to hysterectomy, effects of the procedure on women’s quality of life, perceived risks, and benefits, possible complications, and some other issues.
The questions that are used to acquire crucial information for further analysis would be modified when necessary to reflect the dynamics of the study. Creswell and Creswell (2017) assert that phenomenological research commences with detailed descriptions of lived circumstances, most often first-person accounts, organized in everyday language that avoids the use of scholarly and theoretical terms. The approach enables the researcher to gather a detailed account of the lived experience of women who have undergone hysterectomies. The approach aims to reduce the participants’ personal experiences with a phenomenon to a representation of the shared core (Creswell & Creswell, 2017).
Piloting the Questions
The interview questions have been piloted among a group of participants. Thus, the efficacy of the interview as the tool for obtaining the necessary data is defined. For instance, the possibility of overlooking essential information during the interview or focusing on the information that is not necessary for the research has been detected and addressed respectively. Thus, the questions may undergo certain changes based on the outcomes of the pilot.
Definitions
- Hysterectomy: A surgical procedure to remove the uterus (Lambert et al., 2017).
- Mortality: The state of being susceptible to death (DeJohn, 2014).
- Cyst: A pocket of human tissue (Zhang et al., 2014).
- Antisepsis: A medical practice of using antiseptics to eliminate disease-causing mechanisms (Zhang et al., 2014).
- General anesthesia: A medical treatment that puts patients into a deep sleep to help them avoid pain (Zhang et al., 2014).
- Informed consent: The approval given by a patient for a particular medical intervention implies that a patient provides a healthcare provider with the authority to make decisions regarding the management of the patient’s health (Lambert et al., 2017).
- Comprehensive Informed Consent Law: An all-embracive system of regulations providing women with an opportunity to choose whether to give permission for a hysterectomy, as well as a chance to learn about alternative treatment options (Zhang et al., 2014).
Assumptions
Interviews are the main data collection technique. Based on this research instrument, we assume that the respondents would answer the questions truthfully. Similarly, since a specific research sample is used, we assume that the sample would be representative of the views of women who have undergone a hysterectomy in Mississippi. However, to overcome this assumption, the methodology of this paper includes a snowball sampling technique to make sure that the sample chosen represents the desired demographic.
Scope and Delimitations
Delimitations of a study refer to issues that are within the researcher’s control. The geographical region covered by the study is a delimitation of this study. In this study, the experiences of Mississippi women who have undergone hysterectomy are covered. Another delimitation of the study is the selection of the respondents for the interviews as the main reference point for gathering information concerning the experiences of women who have undergone hysterectomy (Grove & Gray, 2015).
Limitations
Study limitations refer to issues that are out of the researcher’s control (Creswell & Poth, 2016). In this study, time is a significant limitation in particular, during the data collection process where the interviews may be restricted depending on the time allowed by the respondent. Another limitation is the demographic of the analysis. While the study would have been better conducted in large and diverse female populations, the study is restricted to only a few women in Mississippi. The study is mainly focused on sampling the views of Mississippi residents. Therefore, the findings of the study retain their generalizability.
Significance
This study is significant because it focuses specifically on the decision-making process of women in Mississippi who have undergone hysterectomies in the absence of comprehensive informed consent law. By focusing on the lived experiences of this population, this study brings insights into the perceptions of participants’ abilities to make patient-centered decisions related to their health outcomes. Hence, the study’s findings have the potential to bring about a positive social change in women (Grove & Gray, 2015).
This research can lead to the improvement of health services. In particular, medical workers such as nurses and physicians can better understand the experiences of women who underwent hysterectomies. Thus, healthcare professionals can better educate these women who may not easily cope with the effects of hysterectomy. These women often find it difficult to adjust to the problems originating from this surgery (Reis, Engin, Ingec, & Bag, n.d.). This is why the educational assistance of medical workers is of great value to them. This is one of the benefits that this study may bring.
Additionally, by understanding the challenges faced by these women, medical workers can better explain the options that are available to women who may need to undergo a hysterectomy. In particular, they should fully understand the effects of this surgery on the health of a woman. This is another example of a positive social change. Furthermore, this study can demonstrate what particular issues are most pertinent to women who may need to undergo a hysterectomy. By using the findings of the study, medical workers can help patients make informed decisions. This is one of the positive social changes that should be considered (Reis et al., n.d.).
Moreover, it may be necessary to provide counseling to women who underwent this surgery in the past. This type of assistance can also be viewed as one of many health services. In turn, the results derived in the course of this study can assist such counselors who will be able to work more effectively. Thus, one can say this research can eventually promote the practices which can improve the experiences of many individuals whose needs could have been previously overlooked by medical professionals (Reis et al., n.d.).
Data from this study may inform legislatures regarding the need for a comprehensive informed consent law that provides clear guidelines for both patients and physicians. Because some patients do not understand surgical procedures and associated risks, informed consent is fundamental in healthcare. It signifies the physician is speaking to a patient in simple terms that the patient understands, as well as disclosing all pertinent information and dangers. As a result, the patient understands that surgery is a choice (Pop-Vicas, Johnson, & Safdar, 2017). Standards of care are established in guidelines and in the medical evidence and patients have a right to know all reasonable alternatives consistent with high-quality medicine (DeJohn, 2014).
The findings of this study contribute to existing academic knowledge regarding hysterectomy and the absence of informed consent when undergoing such procedures. Policymakers and health practitioners would also find this information useful in developing policies and procedures that guide this health process. This way, they will have a proper guiding framework for the development of informed consent law in Mississippi and around the country. With law guiding informed consent, women will be able to undergo hysterectomy fully aware of the procedure and the consequences.
In addition, women will be capable of making decisions based on the disclosed information. As a result, women will have various treatment alternatives as indicated in the booklets.
Summary
This chapter highlights the nature of the study and sets the tone for the rest of the dissertation. It shows that the researcher explores the lived experiences of women who have undergone hysterectomy without informed consent. The findings of the study will add more knowledge to existing literature. Similarly, policymakers will use the study findings to understand the importance of informed consent law when undertaking medical procedure.
Literature Review
This chapter evaluates previous research studies that have explored the intrigues surrounding women who have undergone hysterectomy without informed consent. It highlights the key variables and concepts surrounding the medical procedure and the different ways that researchers have approached the issue. This way, it is easy to understand the major theoretical composition of the research issue and any major hypothesis that may arise from the same.
Literature Search Strategy
The information included in this study has come from credible sources primarily from previous studies. Most importantly, there has been a keen focus on previous studies published in books, journals, peer-reviewed articles, and credible websites. Some key databases consulted include emerald insight and sage journals. In addition, Cochrane menstrual disorders (CMD) and Subfertility Group Trials Register (December 2009 to January 2014) were searched. Besides, the following health sciences electronic databases were searched into including CENTRAL (The Cochrane Library 2013, Issue 12), CINAHL Plus (January 2009 to January 2014), MEDLINE (January 2009 to January 2014), Health and Medical Complete (January 2009 to January 2014), EMBASE (January 2009 to January 2014), and PsycINFO (2009 to January 2014). Key search terms included “hysterectomy,” “Mississippi,” “Health Belief Model,” and “informed consent.”
Theoretical Foundation
As highlighted in the first chapter, the HBM model outlines the main theoretical foundation of this paper. This framework guides the research process outlined in this paper by narrowing down our focus to behavioral responses and perceptual influences about hysterectomy. Researchers such as Loke, Davies, and Li (2015) have used this theory to investigate the behavioral patterns of patients based on perceptual responses to policy and environmental issues.
Literature Review Related to Key Variables and Concepts
Historical
Hysterectomy has its origin in prehistoric times, with the first operation performed as early as 120 AD by Soranus in Greece. Alsaharavius, a physician in the 11th century, made a commentary about a surgical excision of the uterus. Vaginal hysterectomies had been performed in the middle ages, as revealed by some medical writings (Deffieux, Vinchant, Wigniolle, Goffinet, & Sentilhes, 2017).
In 1809, Ephraim McDowell performed the first abdominal hysterectomy on Jane Todd Crawford, who had a massive ovarian cyst weighing 10.2 kilograms. It took McDowell 25 minutes to remove the left tube and the ovary, while outside his house townsfolk were building gallows for him in case the patient would die. Five days later, Jane Todd was well and up in McDowell’s house and after 20 days, she went home to Greensburgh, Kentucky. At that time, surgeons operated without anesthesia, antisepsis, or antibiotics, and the patient was allowed to recite the psalms to slightly ease the pain. McDowell performed 13 hysterectomies in the course of his practice, with only one death. It was an extraordinary feat considering that sepsis and peritonitis were complications after laparotomy (Deffieux et al., 2017).
Charles Clay came up with the word ovariotomy. On September 13, 1842, he removed a 17 pound, 5-ounce ovarian tumor, with the patient having brandy and milk for analgesia. When anesthesia was discovered, Clay did not want to apply it to his patients, as he considered it a distraction. He reasoned that patients who had the courage to undergo surgery without anesthesia were imbued with a strong will to live (Aarts et al., 2015; Morice, 2014). On January 3, 1863, Clay performed the first successful hysterectomy with oophorectomy and salpingo-oophorectomy (Aarts et al., 2015).
In 1853, Ellis Burnham successfully performed a subtotal hysterectomy and the patient survived. Another surgeon named Kimball performed a deliberate but successful hysterectomy due to a fibroid tumor. Chloroform as a form of anesthesia was used during the operation. Before this time, surgeons used opiates, which contained hyoscyamus and mandragora, mixed with alcohol to desensitize patients undergoing surgery. The nitrous oxide gas was introduced which could induce amusement and euphoria and reduce sensitivity to pain. In 1831, a combination of ether, nitrous oxide, and chloroform was later used as anesthesia. Dentists used ether as dental anesthesia, and it was Oliver Wendell Holmes who first coined the word anesthesia.
Many women undergo hysterectomy for noncancerous illnesses and as a preemptive measure for ovarian cancer. Gynecological problems and cancer are the primary causes of hysterectomy (Peng, Chen, Wu, Hu, & Li, 2017). Many hysterectomy cases in the United States are the result of localized sickness, which means the sickness does not spread to the uterus, and removal of the uterus is not necessary (Peng et al., 2017).
About a quarter of women in the United States may have undergone a hysterectomy by the age of 60, whereas in the United Kingdom, the ratio is one to five women. More than 90% of those surgeries were performed for benign tumors and symptoms for uterine fibroids, vaginal bleeding, and others that are non-life-threatening (Suwannarurk, Thaweekul, Mairaing, Poomtavorn, & Bhamarapravatana, 2014). However, some women undergo complex surgeries such as the peripartum hysterectomy. Gupta and Manyonda (2014) indicated that 40% of all women worldwide will have a hysterectomy by the time they reach 64 years of age, with the primary objective of relieving pain and enhancing the quality of life. With the introduction of alternative treatment, hysterectomy has become less prevalent in most countries (Fylstra, 2015). There are still doubts surrounding hysterectomy and why women should undergo a hysterectomy. Yusuf, Leeder, and Wilson (2016) have focused on the following aspects in their study: (a) Can hysterectomy provide essential treatment for diseases in women’s reproductive organs? (b) Should other less invasive treatments are considered first? (c) How informed are women of the legal aspects of hysterectomy, particularly the subject of informed consent?
Women have to be informed of treatment options other than hysterectomy, which has complications. A comprehensive informed consent law requires physicians to provide information concerning other alternative therapy (Seagle, Alexander, Strohl, & Shahabi, 2018). The benefits of the informed consent law will allow women to decide before any treatment is performed (Seagle et al., 2018). Women should properly understand this information and knowledge of the law (Diamond, 2014).
Hysterectomy is one of the most frequently used operative techniques among many gynecological procedures. However, it is significantly decreasing because there are alternative options, and patients have reported some complications after hysterectomy (Darwish, Atlantis, & Mohamed-Taysir, 2014). Theunissen et al. (2016) found that the complexities in the surgical procedure rise when pregnancies occur. A longitudinal study found that more women who belonged to the lower socio-economic class had undergone hysterectomies than those of the higher socio-economic status. Knowledge about, and access to, other treatment may not be available in specific areas, which is one of the reasons why those who are of the lower socioeconomic status mostly undergo hysterectomy (Ogburn, 2014). Mississippi Delta Region is one of the specific areas where the socio-economic status of women is lower and accessibility to other treatment options is limited (Collins et al., 2014). As a result of the prevailing situation, women also lacked education and experienced poor nutrition as well as healthcare (Collins et al., 2014). These factors could have resulted in the lack of valuable information for women who might have undergone hysterectomies, and there was a dearth of knowledge on cancer screening and other healthcare expenses (Croce, Young, & Oliva, 2014).
Every year, approximately 600,000 American women undergo hysterectomy for non-cancerous causes (Halder et al., 2015). The Centers for Disease Control and Prevention (2014), reported that there were 5.4 hysterectomies for every 1,000 women annually during the period 2000 to 2004. However, the hysterectomy rate is decreasing in Scandinavian countries and in the United Kingdom (Schollmeyer et al., 2014).
Ovarian and uterine cancers are primary causes of hysterectomy (Singh, Ryerson, Wu, & Kaur, 2014). In a study on cervical cancer, researchers found that hysterectomy did not reduce the survival rate but provided comfort in the pelvic region. Moreover, some doctors performed a hysterectomy on complaints of endometriosis, which can be treated with analgesic therapies and other non-invasive methods (Grigore, Ilea, Terinte, Sava, & Popovici, 2014; Heng, Stephens, Jobling, & Nie, 2016).
A study on endometriosis and its effects on the quality of life revealed that this sickness impacted women’s quality of life, particularly their work, education, and home and family life (Heng et al., 2016). The effect of endometriosis on work was more pronounced with 51% of the participants saying that endometriosis significantly affected their work life. Endometriosis also affected the women’s relationships with their husbands, with some participants saying that their sickness caused the divorce. The data collected in the study confirmed the negative effects of endometriosis on women’s quality of life (Heng et al., 2016). Uterine myomata or leiomyomas are some common causes of menstrual bleeding. Approximately 30% of hysterectomies are performed due to the diagnosis of fibroids (Heng et al., 2016). Myomectomy is an alternative to hysterectomy in removing fibroids, but it requires a longer recovery period.
Meaning and Causes
Hysterectomy is a surgical method to treat gynecological problems with the aim of removing the ovaries or the fallopian tube. The removal of the ovaries or the fallopian tube may result in a menopausal period, and the woman will be unable to become pregnant. Uterus amputations do away with uterine cancer. Conversely, oophorectomies get rid of the possibility of ovarian cancer (Collins et al., 2014). Gouy et al. (2017) indicated that bilateral salpingo-oophorectomy (BSO) could reduce the risk of ovarian cancer − the reason why it is performed bilaterally with some hysterectomies. While ovarian cancer can be circumvented, oophorectomy increases the threats of heart disease and lung cancer. Rimbach, Holzknecht, Nemes, Offner, and Craina (2015) also argued that the new methods of the surgical procedure could be used to avoid risks associated with the surgical procedure. Cardiovascular risks may be higher due to the reduced production of endogenous sex hormones (Hampton, 2014; Laughlin-Tommaso et al., 2016; Seki et al., 2014). A previous cohort study supported evidence on the relation of hysterectomy and cardiovascular disease in women who were less than 45 years of age during an operation (Hampton, 2014; Laughlin-Tommaso et al., 2016; Seki et al., 2014).
Relation of HRT and CHD
Some researchers have found that hormone replacement therapy (HRT), which is prescribed for women who have undergone hysterectomy, causes coronary heart disease (CHD) (Kurita et al., 2016). However, there were studies reporting that HRT users did not have cardiovascular risks, while some studies showed that the effects of HRT were not clear and overestimated (Kurita et al., 2016). Women with the uterus intact take prescribed estrogen and progestin as protection from cancer occurrence. HRT, which has a dose of progestin, can ease estrogen in controlling CHD, although there have been reported little increase in CHD in women who take the combined dosage. The study of Kurita et al. (2016) provided inconclusive evidence that HRT caused CHD but the findings also stated that HRT was associated with hysterectomy. Women who use HRT have lower levels of systolic blood pressure and low cholesterol (Kurita et al., 2016).
Techniques and types of hysterectomies
Techniques in hysterectomy include open surgery performed through the vagina or a method using laparoscopy, and the most modern, which is a robot-assisted operation (Tapper et al., 2014). Laparoscopic hysterectomy (LH) is usually applied in benign and malignant tumors. Vaginal hysterectomy is used in many cases while LH is usually performed in cancer cases (Seror et al., 2014). LH can be performed vaginally, accompanied by laparoscopic procedures, or where there is no vaginal component. The American Gynecologic Laparoscopists issued a statement in 2010 that hysterectomies for benign cases should use vaginal or laparoscopic procedures because of the benefits on women (Gupt & Manyonda, 2014). These benefits include lower costs, shorter hospital stays, and quick recovery (Gupt & Manyonda, 2014). However, in a later study in Ohio by the same authors, they found that this method was associated with higher charges than the other two techniques of hysterectomy. In this same study, Gupta and Manyonda (2014) found that the rate of hysterectomy decreased due to the introduction and constant use of laparoscopically-assisted vaginal hysterectomy.
Complete hysterectomy aims for the uterus along with the cervix, while partial hysterectomy does not aim for uterus removal. Supracervical hysterectomy is performed when complications during an operation necessitate completing the required surgery as early as possible. However, supracervical hysterectomy should be planned for patients who are perceived to have higher perioperative complications.
Vaginal hysterectomy is surgery performed through the vagina wherein the surgeon conducts an operation on the vaginal wall to be able to see the ligaments and tissues of the uterus, ovaries, and fallopian tubes (Zafar, Iqbal, Javed, Noor, & Niaz, 2017). These organs can be removed through the vagina. Findings in randomized trials have shown that vaginal hysterectomy allows producing the most beneficial outcomes, at the same time helping use available resources sparingly to allocate them in the most efficient manner and enhance the possibility of a positive outcome (Bilandzic, Fitzpatrick, Rosella, & Henry, 2016; Koleli, Ozdogan, Sariibrahim, Ozturk, & Karateke, 2014; Loke et al., 2015).
In the total hysterectomy, the portion called the top of the vagina is closed, creating a blind pouch. In this case, intestines are placed (instead of the uterus) in the blind pouch created due to hysterectomy (Armijo-Olivo et al., 2014). An abdominal hysterectomy is performed when the woman has acquired an enlarged uterus and cancer has been diagnosed or suspected. This procedure takes a vertical incision, about 4” to 6”, along the pubic section and the navel (Armijo-Olivo et al., 2014). With respect to morbidity and mortality, the research found complications in 44% for abdominal and 27.3% for vaginal hysterectomies. A Cochrane study found fewer infections and rapid recovery attributed to vaginal and laparoscopic hysterectomies than an abdominal hysterectomy (Armijo-Olivo et al., 2014; Gupta & Manyonda, 2014).
Hysterectomy is most necessary when pain cannot be controlled due primarily to fibroids, or pressure, and severe bleeding. It can be applied to postmenopausal women who might have malignant tumors and for symptoms of endometriosis that cause pelvic pain, pain during intercourse, and when there is extreme bleeding (Armijo-Olivo et al., 2014). Hysterectomy is an effective treatment for menometrorrhagia, leiomyoma, and symptoms associated with postmenopause. Women that have not been associated with the ovarian disease would not have their ovaries and fallopian tubes removed. In such women, the production of hormones would be normal even if they experience a lapse in their menstrual cycles. However, when they undergo hysterectomies, they will occasionally cease producing estrogen and experience the menopausal stage (Miyata et al., 2014).
Complications in Hysterectomy
Hysterectomy can lead to psychological or mental problems but some studies have found that hysterectomy provided comfort to women and improved their quality of life. However, women should seek other options before undergoing hysterectomy (Armijo-Olivo et al., 2014). The doctor and the patient should have ample discussion before proceeding, and the doctor must observe the highest ethical standards of medical practice (Miyata et al., 2014).
There are valid medical reasons for hysterectomy, but there are as many valid reasons for not performing it, which means there are other options rather than immediately subjecting the woman’s reproductive region to surgical procedures. Epidemiological studies showed that for two decades, approximately 90% of hysterectomies were done for only benign surgical reasons (Darwish et al., 2014; Laughlin-Tommaso et al., 2016). Women who undergo this surgical procedure must be informed of the reasons why it has to be done, how it should be done, including other medical options and complications in later life. Patients have to think of it and give their consent only on life-threatening conditions (Darwish et al., 2014).
Due to the results of the various studies, the medical profession has raised concerns over the long-term effects of hysterectomy. For example, there has been reported one complication for every 574 surgeries performed in the United States (Brohlet al., 2015). Additionally, studies have found that women who had bilateral oophorectomy had a 17% risk of having heart disease and a 28% risk of succumbing to death due to complications. Lung cancer was also one of the complications (Brohl et al., 2015). Moreover, it has been proven that hysterectomy with oophorectomy affects the development of menopause. Particularly, women have menopause 3-4 years earlier than expected, which is the reason for their blood supply disturbance in the ovaries and can have a detrimental effect on patients’ cognitive functions (Kurita et al., 2016). Some studies also found that women who had undergone premenopausal bilateral oophorectomy showed signs of reduced cognitive functions, but those taking HRT reported improved cognitive functions. The reported dementia because of hysterectomy is still unexplored, but a longitudinal study of homozygous twins who had undergone hysterectomies showed symptoms of Alzheimer’s disease (Kurita et al., 2016). Emre, Akbulut, Yilmaz, and Bozdag (2014) reported numerous deaths because of hysterectomies.
Some studies reported major complications in urinary incontinence (loss of control in urination) and bowel dysfunction, which occur in old age and affect women’s quality of life. However, the study of Emre et al. (2014) on a few randomized clinical trials focusing on the relation of hysterectomy and urinary incontinence provided inconclusive evidence. Randomized clinical trials indicated that the studies had little evidence to offer because only a few cohort studies were conducted. Despite little evidence of cohort studies, Saito et al. (2014) still concluded that urinary incontinence and bowel dysfunction were complications for hysterectomies when women reached old age. Emre et al. (2014) supported this finding when they researched urinary incontinence through Medline articles, using search words, and found that women who had a hysterectomy were 40% higher in acquiring urinary incontinence at later life than women who had not undergone hysterectomy (Emre et al., 2014). Other complications included occasional fever, hemorrhage, and other life-threatening events (Emre et al., 2014).
Pelvic floor dysfunction is a common problem of women who are at the menopausal stage (Wright et al., 2014). Uterine problems can greatly affect women’s social lives, especially in this age of globalization where women have vast roles in society. Hysterectomy can relieve symptoms that have interfered with their daily activities. Studies indicate that over 40% of women who have their ovaries removed have a decreased degree of depression. Moreover, women having a positive perception of their social support network in both pre and post-hysterectomy indicate increased chances of having a better quality of life. Physical complications in hysterectomy include edema and swelling in both legs. Long-term physical effects include numbness, tingling, and limited movement of the legs.
Another factor that affects women undergoing hysterectomies is inequities. Studies have found evidence of inequities for women, which need to be addressed by healthcare professionals for a corresponding intervention. The team should determine the psychosocial drawbacks of hysterectomies and meet the psychological needs of women.
There are cases where hysterectomy is necessary, such as the occurrence of postpartum hemorrhage (PPH), which is related to birth events threatening a mother’s life that affects her adjustment to motherhood (Vijaya, Patel, Purushothama, Mallesh, & Nagara, 2015). Severe PPH is described as blood loss equivalent to about 1,000 milliliters right after giving birth until weeks postpartum (Power, Jackson, Carter, & Weaver, 2015). There are cases where PPH needs an emergency hysterectomy to control the bleeding (Power et al., 2015). PPH and subsequent hysterectomy are two difficult situations that a mother should be able to adjust to after giving birth.
Power et al. (2015) conducted a study on perspectives of early mothering by describing their adjustment and recovery from an emergency hysterectomy after a severe PPH. During the recovery period, the mother may be separated from her baby, as she has to be admitted to the Intensive Care Unit (ICU) for observation and careful recovery (Power et al., 2015). During this time, the mother may experience guilt feelings, shame, and failure. In Australia, the incidence of women admitted to ICU after birth is 1.84 to 2.6% of all pregnant women (Power et al., 2015). UK has a significant number of pregnant or postnatal women admitted to ICU (Power et al., 2015).
On the relation of hysterectomy and breast cancer rate, the study by Gaudet et al. (2014) found no relation between breast cancer rate and simple hysterectomy. However, the researchers found that risk factors for hysterectomy were also common risk factors for breast cancer. This meant the conditions were similar for both illnesses, but there was no relation between hysterectomy and breast cancer.
An analysis of hysterectomy performed for the benign disease was conducted at the Department of Obstetrics and Gynecology, University Hospital Schleswig-Holstein, Campus Kiel, Germany, in which the data were taken from hospital records. The causes for surgery included fibroids and precancerous abrasions of the uterus (Schollmeyer, et al., 2014, p. 45). The techniques used in the various operations included vaginal hysterectomy, abdominal hysterectomy, TLH, LSH, and laparoscopically assisted vaginal hysterectomy (LAVH). Only 766 patients qualified for the criteria of the study. The common cause for hysterectomy was uterine myoma, which accounted for 58.6% of the study. Vaginal hysterectomy was the common technique used for uterine prolapse. In the study period, the researchers found no mortalities for hysterectomy for benign reasons but there were 52 (5.5%) cases, which had complications out of the total 953 operations. For the period 2007 to 2010, the numbers of abdominal hysterectomy and vaginal hysterectomy decreased due to the increase of laparoscopic hysterectomy (LH) and total laparoscopic hysterectomy (TLH).
Some studies found symptoms of psychological co-morbidity due to hysterectomy, which can result in negative feelings about body image, sexual orientation, youth, energy and physical activities, and reduced child-bearing ability (Darwish et al., 2014). However, in conducting a meta-analysis of the different studies and articles on hysterectomy, Darwish et al. (2014) found that hysterectomy performed for benign gynecological conditions was positively associated with depression or anxiety outcomes. Moreover, long-term studies suggested that women returned to their physical and psychological functioning after hysterectomy. Darwish et al. (2014) study further found that hysterectomy, no matter what type and technique used, had improved the quality of life and psychological outcome of women. There was a reduction in the symptoms of depression and depression scores compared to the preoperative indications. This suggests that women usually felt comfort after the non-malignant indications were removed due to hysterectomy. Sexual pleasure, arousal, and desire improved after hysterectomy, regardless of the surgical technique used (Darwish et al., 2014).
Impact of Hysterectomy on Women’s Lives
In other cases, hysterectomy creates psychological problems such as depression and low self-esteem, and negative outcomes on patients’ social lives. Power et al. (2015) indicated that women feel intense pain right after hysterectomy. In their research, Power et al. (2015) studied 27 women experiencing abdominal or vaginal hysterectomies, with their mothering capacity being the key inclusion criterion. The researchers found that hysterectomies limited their physical activities while others felt the experience was worse than a caesarian section. A cesarean section accompanied with hysterectomy requires time to recover, as this may result in emotional, physical, and psychological stresses (Power et al., 2015).
Hysterectomy without ovary removal is a different case. It has been argued that hysterectomy does not greatly affect women when the ovaries are not removed. However, quality of life should be considered when determining the effects of illness. Quality of life is linked with the individual’s sense of comfort and happiness in life. Studies in Taiwan and Turkey have found that women regard their uterus as the embodiment of femininity and maternity. As a result, the loss of a uterus is viewed as the failure to fulfill their purpose as women (Pendleton et al., 2016). In the study on women who have undergone hysterectomy, Pendleton et al. (2016) found that hysterectomy adversely affects patients’ body images, self-respect, and matrimonial status.
In order to answer the various concerns about the overuse of hysterectomy, scholars from the University of California at San Francisco conducted a study on hysterectomy and other treatment options and their impact on women’s quality of life. The study employed 63 participants, aged 30 to 50, who were suffering from excessive bleeding for four years. The women took synthetic progesterone treatment, but this was unsuccessful. The researchers recommended a hysterectomy to a group of participants and some to hormonal medication or birth control pills. The researchers asked the participants of their opinion about the quality of life, their physical and mental conditions, and their feeling after hysterectomy. After a period of six months, the participants who underwent hysterectomies reported reduced abnormal bleeding and had improved sleep and quality of life, including overall health and wellbeing. Seventeen of the 32 members of the medication group opted to have a hysterectomy and reported improved well-being. However, the participants who did not undergo hysterectomy also reported improvement in their quality of life (Brohl et al., 2015).
Additionally, in a 2000 survey of women who have undergone surgery, the researchers found that respondent women reported improved sexual functioning (Ogburn, 2014). A randomized survey in 2007 by “BJOG: An International Journal of Obstetrics and Gynecology” supported this finding, wherein respondents who had hysterectomy reported enhanced sexual functioning than they had before they underwent hysterectomy (Ogburn, 2014). In a report by the Maine Women’s Health Study, many women indicated that they were satisfied with the result of a hysterectomy. In a study on women aged 25 to 50 who had either hysterectomy or noninvasive treatments for benign tumors, fibroids, abnormal bleeding, and pain in the pelvic region, Dr. Karen Carlson of the Women’s Health Unit at Massachusetts General Hospital in Boston found positive perceptions of hysterectomy. The respondents reported that hysterectomy relieved their gynecologic problems and that their physical and mental health improved. A small percentage of the population indicated that they lost libido and had little sexual enjoyment (Ogburn, 2014).
Women and Informed Consent Law
It is noteworthy to provide some actual cases of hysterectomy in this section to define the impact of this medical practice on women’s lives. Ogburn (2014) underwent surgery to get rid of a benign cyst but later found out that the doctor who operated on her also removed the uterus and ovaries. It was a traumatic experience for this woman that led her to some unexplored activities as a woman and as a health activist later on. Ogburn (2014) then founded a not-for-profit foundation known as the “Hysterectomy Educational Resources and Services Foundation” (HERS) to provide valuable information for women who might experience non-life-threatening medical situations and the benefits of an informed consent law before they undergo hysterectomy (Ogburn, 2014).
Roth and Ainsworth (2015) provide another case involving an imprisoned woman who was rushed to a hospital for an emergency appendectomy. During the operation, the surgeon found severe endometriosis. A gynecologist was asked to give an opinion and she concluded that the best option was to remove the fallopian tubes and the ovaries. Discovery revealed the patient had a bilateral ovarian cystectomy for endometriosis but was not informed that it would create a serious problem in the future. The patient was completely depressed to learn that she had lost her reproductive organs. The endometriosis was so severe that the patient would not have a chance of natural conception and the cysts should be removed. The review also concluded that new consent forms should have a space in which patients can designate procedures that they do not wish to be done. According to Roth and Ainsworth (2015), some women who awoke finding that they had lost their womb and reproductive organs considered their situation as a violation of their physical integrity. These women believed that the time for consulting and thinking over the choice of a procedure is important because even a short postponement of the surgery can allow women to estimate all the risks they may face. Thus, the patient should have time to think about her situation and all information should be provided to her.
The Sarah Lee Brown Case
In 1987, a case involving Sarah Lee Brown and Dr. John Mladineo became the subject of a legal battle over medical malpractice (Brown v. Mladineo, 1987). Instead of only the tumor that was to be removed, Dr. Mladineo performed a complete hysterectomy on Ms. Brown (Brown v. Mladineo, 1987). After a week of discharge from the hospital, Brown complained of excreting bodily waste by way of her vagina (Brown v. Mladineo, 1987). When the doctor was informed of Brown’s complaint, he advised the patient to take a peculiar treatment – drink some vinegar (Brown v. Mladineo, 1987). Brown was admitted to the same hospital where Dr. Helen Barnes treated her for a rectovaginal fistula, which was caused when Dr. Mladineo performed the surgery and accidentally created a canal in the rectum to the vagina (Brown v. Mladineo, 1987). This case would not have happened if there had been an adequate informed consent law regulating surgeons before performing a hysterectomy.
Comprehensive Informed Consent Law
During the days of slavery in America, black women were subjected to sterilization because they were deemed unworthy to provide offspring. This was known as the “Mississippi Appendectomy”. In the 1950s, black women were provided with contraceptives so that the black population would not grow.
It is a different environment today. A woman’s reproductive decisions are protected under the Fourteenth Amendment of the U.S. Constitution. Court decisions support the principle that reproduction is part of the very essence of human identity and reproductive choices are regarded as irrefutable rights as they are defined in the 14th Amendment, which should not be bypassed by any government agency or regulation (Ross, 2018). Although Supreme Court jurisprudence states that the right to reproduce includes using contraceptive medications, as well as having an abortion, and the right to refuse to be sterilized (Skinner v. Oklahoma, 1942), law scholars and practitioners contend that these rights should extend to the areas of reproduction and child bearing decision-making. Birth decision making and procreation are personal choices that are supported by public policy, husbands’ and wives’ testimonies on the meaning of such choices, and the social consequences of those choices.
However, Purcell, Cameron, Lawton, Glasier, and Harden (2016) argued that reproductive choices are usually made with the influence of a doctor in the hospital, supported by government funding and legislative mistake. The state regulates and controls reproductive choices based on its policy of promoting public health despite the constitutional provision that protects such choices (Purcell et al., 2016). In a country that has a comprehensive informed consent law, a woman with problems in the reproductive organs is given the option to choose. The doctor must explain the various reasons, but the woman must have the final choice. Other states have passed their versions of the law. North Carolina enacted the Woman’s Right to Know Act (WRKA), which provides that women should be provided necessary information before they decide to have an abortion (Arrigo & Waldman, 2014).
The traditional practice of hospitals is that when a patient is scheduled for surgery, she is required to sign a consent form. The form contains provisions where the surgeon is authorized to perform further surgery where the surgeon thinks necessary. In this case, there should be an open discussion with the patient regarding the available treatment options. The form should not be overall consent. The patient can seek redress by asking for police assistance or directly going to court (Low et al., 2017).
Alternatives to Hysterectomy
Complications in hysterectomy force some in the medical profession to perform alternative treatment, and one of these is uterine artery embolization (UAE). According to a study, UAE provides symptomatic relief compared to hysterectomy (Brohl et al., 2015). There have been positive findings of patient satisfaction for UAE, like shorter time of hospitalization, but the patient has to go through a surgical intervention after a few years (Bruijn et al., 2017). UAE is also an effective treatment for myoma (Dueholm, Langfeldt, Mafi, Eriksen, & Marinovskij, 2014).
There are other alternatives to hysterectomy provided by the medical profession. For menorrhagia, women are now aware of the other treatment options. Endometrial ablation, which targets the lining of the uterus, is simpler to perform with fewer complications than hysterectomy. The National Heavy Menstrual Bleeding Audit of the Royal College of Obstetricians and Gynecologists and the National Institute for Health and Clinical Excellence (NICE) have advised that women experiencing extreme menstrual bleeding should undergo subsequent intervention of ablative trials. NICE reported that ablation as an alternative to hysterectomy can improve women’s quality of life. If it still fails, then the patient should be advised to undergo a hysterectomy (Gupt & Manyonda, 2014; Tiwari, 2014).
A technical innovation that is gaining popularity is the use of uterine manipulator (UM) which is under the classification of minimally invasive hysterectomy (MIH). The doctor removes the uterus by way of the vagina, improving exposure in the pelvis and increasing the length between the urethra and the operative field (Zhang et al., 2014). One problem with MIH is when the UM disseminates cancer cells, although this is still a debatable one because of the lack of empirical studies regarding this issue (Ringash et al., 2017; Yildirim et al., 2014). The surgeon inserts the manipulator which increases intrauterine pressure when the balloon is inflated. This can enhance lymph vascular space invasion (LVSI) or enhance the passage of malignant cells through the fallopian tubes into the peritoneal cavity. Another problem with the UM is that it can disaggregate tumor cells (Yilmaz et al., 2014; Zhang et al., 2014).
An alternative to hysterectomy for women with excessive menstrual bleeding (that is not due to cancer, fibroids, or endometriosis) is “balloon ablation” which destroys the endometrium, or uterine lining but does not involve uterus removal (Zhang et al., 2014). The principle reflects that of the balloon angioplasty procedure, which also uses a “balloon” to open blocked coronary arteries (Yildirim et al., 2014). In balloon ablation, a sterile solution is attached to the balloon so that it coincides with the shape of the uterus. Something is placed in the balloon to heat the fluid to 190 degrees Fahrenheit temperature. The heating process lasts for eight minutes. The purpose of the heating process is to destroy the endometrial tissue that touches the balloon (Zhang et al., 2014). The final stage consists of deflating the balloon, draining the fluid through the catheter, and removal of the catheter (Yildirim et al., 2014).
Reducing Variations in Surgery
Doctors can reduce variations in surgeries for ethical and economic reasons. Reducing variation can help myriad patients and reduce mortality and unwarranted use of resources. Patients can have other choices if the surgery can offer no benefits. Sanchez, Barach, and Johnson (2017) suggested that patient autonomy can reduce variation. However, reducing variations should be assessed by health experts who have a broad and clear interpretation of the facts in a particular case. The doctors involved should conduct further investigation if a proposed hysterectomy case is cleared with the patient or not. There should be sound evidence to provide a surgical intervention that is effective for such a disease (Sanchez et al., 2017).
Apart from the value, causes of variation include the factors associated with the delivery system, and are linked closely to cultural beliefs, and are affected significantly by the presence of casemix-adjusted data. With the application of the decision pathway, one can alter surgery processes to a considerable extent (Sanchez et al., 2017). Medical reports have noted lower deaths and complications than a few decades ago because of surgery (Sanchez et al., 2017).
Studies suggest that signs for an operation are difficult to discern in surgical guidelines and many published material only point to patient care after the decision for an operation has been made (Sanchez et al., 2017). Indications for hysterectomy have been much abused because these were not clear, which means hysterectomies were conducted without substantial reasons or causes for why they should be performed (Sanchez et al., 2017).
Evidence about the benefits and risks of surgery is significant in the decision to reduce variations, but it is not a decisive one. Variation for surgery can be provided if there is no treatment benefit or if there is no identification of the best treatment. Some new techniques of surgical practice have been introduced, but these are incomplete and slowly implemented, which means there is still a lack of evidence for its success (Sanchez et al., 2017).
A Cochrane study on the effects of clinical decision making of passive distribution of review evidence showed that appropriate reduction in surgery rates can be accomplished with the distribution of a bulletin. Educational measures distributed to surgeons doing operations resulted in a 9% fall in the operation rate. Additionally, shared decision making, which aims to give patients balanced information and a friendly atmosphere to give them the chance to choose the right treatment that fits their values and beliefs, is an ethical priority for the doctor and can reduce unwanted variation in surgery rates (Sanchez et al., 2017).
The Principle of Informed Consent
The principle of informed consent states that doctors and other health professionals should provide information on health risks and treatment options and get their consent to proposed medical procedures from their patients (Pallett et al., 2016). Women should be legally and humanely advised before undergoing hysterectomy. Without a consent law, it is possible that some physicians will not brief their patients about the complications or treatment alternatives. Passage of law means reducing threats or health risks, and patients are protected from medical malpractice. A comprehensive informed consent law provides that doctors inform women of the parameters and consequences before they give their consent to undergo a hysterectomy. Informed consent is provided to enhance patient autonomy (Pallett et al., 2016).
Mississippi women give their consent for a surgical procedure without an informed consent law, which challenges their health and rights as women. With an informed consent law, the doctor is mandated to provide information about all treatment options and effects of hysterectomy to a woman who is about to undergo hysterectomy (Corona et al., 2015). The doctor should provide all the information, and the patient should be the last to decide with the assistance of the doctor. Pallett et al. (2016) suggest that there should be a consensus between the doctor and the patient undergoing hysterectomy. With an informed consent law, the doctor is obliged to discuss with the patient whether a hysterectomy should be performed.
Informed consent is a legal term that lays down the manner in which physicians or surgeons conduct treatment or surgeries on their patients. In the medical profession, physicians are obliged to provide an explanation on the attributes of planned therapeutic action, its diagnosis for treating the infection, its hazards, and options to the anticipated diagnosis (Ahmed, 2015). The law provides for fines and other punishments if physicians diverge from what they are supposed to observe under the law and ethical principles, based on people’s treasured worth of “autonomy” (Spatz, Krumholz, & Moulton, 2016, p. 2063). When a patient and surgeons enter into an agreement, they are governed by certain rules and ethical practices (Shen, 2015). This is one ground on which such a law should be passed in Mississippi.
The principles of medical law provide that autonomy and consent are related. The focus of informed consent is that the doctor should provide all information as this is important to the patient’s decision whether to have a hysterectomy or not (Shen, 2015). Autonomy focuses on guiding where one is going, deciding where to go and in what activities to engage. Other studies also supported the autonomy principle in the context of informed consent. Informed consent enhances the patient’s independence. Autonomy also connotes treating an individual with informed consent as opposed to James Taylor’s contention that when a patient is being treated, the well-being of that person is the primary concern (Shen, 2015).
Autonomy means the patient dictates her life’s direction. For a patient to be autonomous, specifically in her decision to undergo a medical treatment, the doctor should not stop her decision, or control her decision by selecting information about medical options. Otherwise, the doctor would compromise the woman’s decision regarding her medical treatment. All information about other treatment options should be given to her. Healthcare professionals can refrain from taking over the patient’s autonomy by providing them with all information about the alternative courses of treatment that are at their disposal, including the advantages and disadvantages of those options. Some medical scholars and researchers have recommended reducing variation in surgical procedures, which has ethical and economic effects on surgery rates. Patient autonomy can be elevated, and a woman can choose to avoid it if there are no benefits to be derived from surgery (Sanchez et al., 2017).
Although attacked on both sides, the principle of informed consent has impacted the medical profession (Pallett et al., 2016). The concept of providing necessary information and acquiring consent from the woman to be placed under the knife has become a benchmark for change from the traditional protectionist and patriarchal method of treatment and a benchmark for yearning of enhancing women’s rights. There may be shortcomings to this present trend but patients’ rights, hospital ethics, the need to provide appropriate medical information to patients, and the need to acquire patient’s consent are now ordinary procedures in medical institutions, hospitals, clinics, and doctors’ dealings with their patients (Pallett et al., 2016).
In North America, doctors performed some hysterectomies even if they were not necessary. Investigations were conducted in the United States and Canada, which found that there were unwarranted hysterectomies performed. The medical profession is not united on this medical procedure regarding the reasons for hysterectomies in women (Pallett et al., 2016).
As mentioned, there are minor and serious complications in hysterectomy. The Hippocratic code on medical ethics states that the doctor will treat the patient according to his/her capability and knowledge but not to hurt or injure the patient. Furthermore, if the patient can have a choice of another method of therapy, it is possible that the mode of therapy is less expensive than surgery (Pallett et al., 2016). The doctor has a big role to play in the woman’s decision, but the doctor can also influence the decision. This, however, depends on the provisions of the informed consent law.
Proponents of women’s autonomy argue that the woman has individual rights, more valuable than the right of the fetus. They criticize and want to be free from government regulations and doctor’s intervention on reproductive issues because this comprised women’s autonomy (Pallett et al., 2016). Others argue that women’s autonomy is weakened because they are discriminated against by men. With the principle of informed consent, any doctor who operates on a woman and removes something from the reproductive organ without the patient’s consent commits an offense like physical injury or coercion (Pallett et al., 2016). Patients’ consent is not the only thing necessary, rather, adequate information that can help in the patient’s promulgation of a logical decision should be provided by the doctor. Patients can also refuse any treatment indorsed by the doctor and the doctor can be unethical and may violate the law if he/she refused to provide information regarding the patient’s condition, including other options, risks, and complications because of the treatment (Pallett et al., 2016).
Concerned organizations have provided guidelines, which include a case-by-case risk assessment based largely on the woman’s family history. Halder et al. (2015) conducted a study on women who underwent hysterectomy for the period from 2000 to 2010 and patients who underwent bilateral oophorectomy. The study identified 752,045 women who underwent hysterectomy wherein 403,073 patients had ovarian conservation while 348,972 underwent bilateral oophorectomy. The number of ovary removal has been controlled, particularly on women ages 45 to 49.
The study of Halder et al. (2015) suggests that ovarian conservation has been increasing. Procedural factors influenced this trend, such as the type of hysterectomy, which influenced the most for retaining the ovaries. Hospital characteristics influenced about 10% in the decision to conserve the ovaries, while 5% and 3% were attributed to patient decisions and physician characteristics, respectively (Halder et al., 2015). The researchers noted the variation and grouped the participants according to age and for those who underwent vaginal hysterectomy or not. Many hospitals admitted and subjected women of this latter grouping. The percentage of ovarian conservation registered as rather high. Hospitals across the United States have chosen to tread along the path of ethical practice by performing hysterectomy and bilateral oophorectomy only in extreme cases. The trend for ovarian conservation is influenced by data collected by hospitals regarding the relationship between oophorectomy and coronary heart disease and possibly mortality (Halder et al., 2015).
Gender Identity
A woman’s reproductive system is associated with gender identity. When this is removed by surgical means, the woman loses herself (Meij & Emanuel, 2016). Medical sociologists argue that medical treatments like hysterectomies can affect women’s lives. When a woman undergoes a hysterectomy, she loses one part of her identity as a woman and that is menstruation. Medical sociologists contend that monthly period and female femininity are correlated positively (Meij & Emanuel, 2016). Randomized studies that have been conducted indicated that menstruation is highly recognized by women (Meij & Emanuel, 2016). Menstruation makes women different from men, and they would not like to give it up so easily through hysterectomy. Menstrual periods provide an emblematic and substance connection between women. Hysterectomy marks the end of a woman’s menstruation, which disturbs gender identity, as this is closely related to womanhood (Meij & Emanuel, 2016).
Quality of Life (QoL)
The process of healing must be in several stages. Although painful as it may be, a woman who undergoes hysterectomy becomes a new individual (Danesh, Hamzehgardeshi, Moosazadeh, & Shabani-Asrami, 2015). Healing stages must be experienced with the care and a positive attitude. The loss of one part must lead to the recovery of a new life’s horizons. Various studies indicated that women who have undergone hysterectomy should develop a new way of looking at life and womanhood.
Nursing care should be planned adequately to correspond to the various stages of the healing process. Specific nursing care should make the patient move from the stage where she was dependent through a stage where she becomes conscious, self-actualizing, and independent (Danesh et al., 2015). The first stage should involve the patient coming out of isolation. Breaking free from hiding and numbness and accepting the innermost pains are significant movements that should be followed. Second, the numbness must be resolved and transformed into feeling (Danesh et al., 2015). In fact, suffering is a part of life that sometimes cannot be avoided and acceptance of suffering is the best way to reduce the pain. Visits from a mental health nurse or a professional person who can provide meaningful counseling are essential. The next stage is releasing or emptying, which involves dealing with fear and accepting the reality of womanhood (Danesh et al., 2015). The processes of emptying are in four vital steps:
- The patient must take hold of the pain like a pack of sticks to build a fire.
- The sticks have to be held in an embrace so that the person can move across the room to the fireplace.
- When reaching the fireplace, the individual can release the sticks and let them go.
- After all the steps, the individual feels warmed and happy from the sticks she has thrown out to the fire.
The individual who has undergone a hysterectomy must embrace womanhood once again after she has suffered from the medical event (Danesh et al., 2015). Studies indicate that one can accept the fact that suffering enables one to admire life, feel compassion for others of the same fate (Danesh et al., 2015). A woman who chooses to undergo a hysterectomy must learn to endure the pain because this can lead to an improved quality of life (QoL). QoL is multidisciplinary, but its definition is not universal, as it can be seen from different perspectives (Huber& Tu-Keefner, 2014). Hysterectomy can lead to improved QoL if the woman knows how to deal with it, patiently and perseveringly. There are also several notions and concepts which are influenced by culture. The World Health Organization classifies QoL into several broad areas, including physiological, emotional, and social ones (Huber & Tu-Keefner, 2014). Each of these areas affects all the others while QoL covers the entirety and wholeness. The WHO definition highlights life’s goals, expectations, aims, and anxieties of individuals as they go on and meet life’s sufferings. Health-related quality of life (HRQL) encompasses the person’s entire well-being. According to international experts, HRQL includes the physical, social, and emotional areas of a person’s functions, including awareness of a person’s quality of life and general life satisfaction (Huber & Tu-Keefner, 2014).
Positive and negative effects can be seen on women who undergo a hysterectomy. With the loss of fertility, the woman may become anxious and afraid of the many personal issues surrounding her life and her relationships with the people around her, particularly her husband (Huber & Tu-Keefner, 2014). Women complained of difficulties in uterine problems, including physical and menstrual pain, emotional and sexual dysfunctions, and a decline in general health.
Summary and Conclusion
This literature survey has explored the advantages and disadvantages of hysterectomy. The empirical studies provided the pros and cons and hysterectomies and the reasons why doctors recommend surgeries. The surgeon should provide the necessary information for the woman to choose what best suits her health. Like any other medical activity or event, doctors have varying views. There were patients who reported improved life while others had negative feelings about hysterectomy. In other words, the subject needs more empirical studies to substantiate what is in the literature. The presence of the informed consent law can also affect the outcomes.
This study uses a theoretical framework known as the health belief model (HBM) to determine problems of behavior. Researchers use HBM to understand and predict how patients apply health prevention and services. HBM begins with a hypothesis that actions pertaining to health are influenced by factors like the presence of adequate motivation to make problems of health significant; the idea that a person is at risk to a health issue or as a consequence of that health problem, or there is the perception of a health threat; and the belief that observing a doctor’s or a health worker’s recommendation would reduce the health issue at lesser costs (Huber & Tu-Keefner, 2014).
Authors argue that HBM is linked with social cognitive theory (SCT) (Collins, 2016). Young, Plotnikoff, Collins, Callister, and Morgan (2014) further expound on the concept of HBM elements, such as apparent benefits, difficulties, and indications to action. Individuals exhibit certain behaviors when they feel that: (a) benefits are derived in exhibiting the behavior, (b) the benefits are greater than the barriers in displaying such behavior, and (c) there are clues reminding them to display such behavior (Young et al., 2014). This concept was later modified and combined with Howard’s model: individuals need a stimulant to enhance their decision-making process, or they need to be motivated with what is known as an environmental cue (Young et al., 2014). The combination of Howard’s model and HBM provides the explanation of patient behavior relative to the subject of health services. The model further explores that when individuals look for information about their health, the motivation relies on how confident they are in understanding and providing excellent choices with regard to their health. Self-belief and experience of an exact choice are relevant when the individual seeks information about the availability of health services (Young et al., 2014).
Young et al. (2014) explained that for individuals to take action to avoid sickness, they have to believe that: (a) they are vulnerable to the disease; (b) the disease can inflict a severe impact on some part of their lives; (c) certain behaviors can reduce the severity of the disease whenever the disease inflicts upon them; and (d) these behaviors cannot be hindered by aspects like expenses, pain, humiliation, or the perceived barriers. HBM has a predictive ability and we can expand this to include the concept of self-efficacy, which is the perception or belief in how competent an individual is in possessing certain behavior (Young et al., 2014).
HBM constructs assert that individuals make decisions based on their beliefs and perceptions. The individuals’ actions relate to surgeries, preventive care, and other forms of treatment. HBM can provide the explanation of theories regarding the experiences and treatment responses/reactions of Mississippi women who have undergone or will undergo hysterectomies. I took this out so it cannot get confused with the research questions.
Methodology
In this chapter of the dissertation, I explain the methods for conducting the research. This section provides a description of various study techniques ranging from data collection method to research strategy. Lastly, this section of the paper also explores the ethical considerations of the research.
Research Design and Rationale
The research questions are:
- What are the perceptions of women who have undergone hysterectomy without prior awareness of comprehensive informed consent?
- What are the new themes that emerge from the lived experiences of women who have undergone a hysterectomy in the absence of comprehensive informed consent law?
The central concept of this paper is to understand the influence of informed consent in shaping the lived experiences of women who have undergone hysterectomies. The research tradition for investigating this central concept is to use a qualitative approach for sampling the views of the respondents. The rationale for doing so is that the qualitative approach best samples people’s attitudes and perceptions (Grove & Gray, 2015).
Role of the Researcher
One of the characteristics of qualitative studies is that other researchers under similar conditions and comparable results attained should repeat it. The attribute makes the qualitative studies different and the role of the researcher in the process significant (Grove & Gray, 2015). In fact, in qualitative studies, the researchers are considered as part of the data collection instrument. The researcher plays a critical role in reconciling the data collection process. Despite the availability of the data collection instruments such as the questionnaire, the data collection process is facilitated by the human mechanism or the researcher (Grove & Gray, 2015).
During the facilitation process, the researcher explains different aspects of the study including the expected biases as well as the assumptions made in the study. Moreover, the researcher describes the study expectations as well as the experiences that qualify the ability to conduct the study (Khatib et al., 2014). In addition, it is critical for the researcher in qualitative studies to keep records that expound the individual reactions, reflections as well as insights concerning the undertaken study.
Besides, the researcher should also be in a position to differentiate whether their role is emic or etic (DeJean, Giacomini, Simeonov, & Smith, 2016). In other words, the researcher acts as an insider who fully participates in the study. On the other hand, an etic role is where the researcher acts as an outsider or a mere objective observer. Nevertheless, in most instances, researchers find themselves acting in both responsibilities (DeJean et al., 2016). Researchers normally begin the interview as an outsider and gradually become a member of the interviewee through the appropriate explanation of the study instrument. The reverse case can also occur in which the researcher starts as an emic observer and progressively becomes an etic participant. Such variations exist in qualitative studies (Sirimusika et al., 2014).
Studies indicate that a good qualitative researcher has the capability of probing the research questions. The researcher listens, thinks through the answers from the interview, and then delves deeper through probing questions in order to understand more concerning the conversation (Grove & Gray, 2015). The researcher should build a bigger picture using ideas and theories borrowed from diverse sources (Grove & Gray, 2015).
Using the above information, my role as a researcher is to interview the respondents and investigate emerging themes and patterns from their responses. In order to identify the emerging themes and patterns, I employ various interview tactics to ask probing questions. Moreover, through the application of ideas and theoretical frameworks from a wide variety of sources, I build a bigger picture in order for the interviewee to understand me and attain the desired answers.
Participant Selection Logic
Even though all women who have undergone the hysterectomy in Hinds County, Mississippi qualify to partake in this study, only ten respondents have been selected to participate in this study. The identified number of participants is recruited from a support group and selected based on the level of their experiences with hysterectomy, as well as their willingness to participate in the study. Since the study aims to provide a qualitative, subjective perspective on the problem of interest, greater attention is paid to the quality of the collected information and not the quantity.
Comprehensive and well-structured face-to-face interviews are administered in order to collect detailed and in-depth data from the experienced participants. Considering the level of respondents’ expertise, it is enough to carry out only ten interviews to achieve the research saturation needed for high-quality interpretation of results and finding links between the studied variables. It is worth noticing that saturation is core to qualitative sampling and can be achieved merely when sampling is supported and combined with appropriate data collection and analysis tools (Baker & Edwards, 2012). Considering that possible biases associated with a small sample size are minimized through the utilization of appropriate and credible research instruments and elements of design, which will be discussed later in the paper, the use of information retrieved from ten participants in the present research project seems legitimate.
As for the face-to-face interview, it can address the main points while paying close attention to related issues that are not covered in the questions. In other words, the interview questions are semistructured, thereby allowing the interviewees to give whatever type of response they wish. Specifically, during the interview, the researcher has encouraged the respondents to give their lived experiences about hysterectomies. Moreover, during the interview, the researcher has also sought clarification in instances when there are unclear responses.
Instrumentation
Brixey, Brixey, McCormick, and Saba (2015) stated that all researchers should adopt prudent ways of collecting data. Particularly, he draws our attention to data collection methods that give respondents the freedom to express themselves (Taylor, Bogdan, & DeVault, 2015). The main data collection instrument in this study is the interview questions (Appendix A). The questions are open-ended and well designed in order to capture the main issues in the study while offering flexibility for the researcher to probe deeper into the responses provided by the respondents (Taylor et al., 2015). As indicated, face-to-face interviews are associated with the risks of the respondents giving false information since the individuals who are interviewed might be lured to do so (Taylor et al., 2015). In order to avoid the problems, the interview questions will be designed to allow flexibilities for the researcher to provide individual participants with more guidance on what to talk about depending on the observations.
For Researcher-Developed Instruments
DeJean et al. (2016) say that the qualitative research strategy has several types of designs. They include the use of inquiry, the research approach defined as a narrative, a phenomenological design, the application of participatory action, the development of a grounded theory, carrying out ethnography, and conducting a case study (DeJean et al., 2016). The proposed study uses the phenomenological research design. This design is right for this paper because it focuses on people’s experiences and life conditions (Creswell& Poth, 2016). Furthermore, it provides researchers with an opportunity to measure the perceptions of those experiences. This way, the phenomenological design will help to distinguish different phenomena from the respondents’ views, which is how we construct reality. This research design also merges with the main data collection method (interview) because it interprets facts, depending on people’s assertions. This way, the participants’ subjective opinions provide the framework for forming the research findings. Through this understanding, DeJean et al. (2016) stated that the focus of phenomenology is on the detailed analysis of reality. The main drawback of using the phenomenological research design is the difficulty of preventing researcher bias. Furthermore, since this research design mainly depends on subjective data, it is difficult to guarantee the validity and reliability of the findings obtained (Creswell & Poth, 2016).
Procedures for Recruitment, Participation, and Data Collection
Besides factoring in the interview responses given by the research participants, this study merges theory and data. The recruitment process includes sending an electronic letter with basic information about the research to the group’s leader who forwards it to other members. The participants’ names or e-mails will never be obtained from the leader/president of the support group. Those who decide to participate respond to the letter using the researcher’s e-mail address or phone number. The researcher and potential interviewees have met for consent procedures and interviews in a private room in a public library.
The eligibility criteria include a hysterectomy experience and age (20-40). The theory part would mainly come from the findings obtained from other researchers. Since the quality of theoretical data cannot reliably be assessed from the published reports, amalgamating these findings with raw interview responses would highlight the need to include deductive and inductive approaches in the data analysis (Andersen et al., 2015; Gattinoni & Giomarelli, 2015; Greenberg, Daniels, & Flanders, 2015). Moreover, since interviews outline the main data collection technique, an inductive approach would suffice. This paper is based on the inductive research approach because it can condense raw data into easily comprehensible summaries. Furthermore, this research approach easily establishes the link between the raw data obtained from the interviews and the research objectives. From this process, it is easy to develop a framework for understanding all the different sets of raw data obtained from the interviews. Studies indicate that the general inductive approach provides an easy-to-use and systematic set of procedures for analyzing qualitative data that can produce reliable and valid findings (Arnetz et al., 2015). Some researchers have criticized the inductive research approach for failing to provide a strong analytical focus that can be used to construct a model (Shen, 2015). However, this study uses an inductive research approach in developing the interview questions because it provides a simple evaluation of direct interview questions. Indeed, many researchers find the inductive approach easier to use than other data analysis methods.
Data Analysis Plan
Creswell and Poth (2016) argued that the best data analysis method should resonate with the nature of the data collected. This chapter has already shown that the interview method is the main data collection technique. This paper uses the thematic data analysis method as the main data analysis tool. It works by picking out unique themes from the responses given by the research participants. To do so, the themes represent the essential experiences of the respondents. Collectively, these themes would represent abstract concepts of the research questions. Simpson and Augat (2015) asserted there are two types of themes that would emerge in such kinds of analyses. The first type is the collective theme, which represents unique concepts that represent the views of two or more people. The second one is the individual theme, which only applies to the views of one respondent. Both categories would outline the data analysis method. Nvivo is the primary device for data collection and analysis; a Nvivo expert is hired and asked to sign a confidentiality agreement if identifiers are used. The identified software allows for gathering and classifying qualitative data to locate common themes afterward.
Issues of Trustworthiness
Since this study uses human subjects, trust issues are bound to emerge. To gain the respondents’ confidence, their names and contacts remain anonymous. In other words, all the participants who take part in the research remain unidentified. This requirement is important because the research involves investigating the lives of women who have undergone hysterectomies. Some of them would like to keep this information private. Lastly, the researcher makes sure that the respondents understand that the proposed study will not expose their personal information because it aims to meet academic goals only.
Ethical Considerations
Ethics is one of the issues that researchers need to give increased consideration to during the study process (Creswell & Poth, 2016). Ethics are values or moral obligations the researcher has to observe during the research process. Moral obligations are normally associated with the consent of the participants and confidentiality (Grove & Gray, 2015). Informed consent is the permission of the respondent to take part in the study process (Grove & Gray, 2015). The researcher has to explain to the respondent the importance of the study and why it is important for the respondents to take part in the study. On the other hand, like in most professional practices, confidentiality is the moral obligation to ensure that the information provided by the respondents is kept private. The information can only be shared in the circumstance that the respondents have provided their permission or when it is so important that it could be used to save the life of the third party (Creswell & Poth, 2016). The two important issues guide the conduct of this study. However, the ethical consideration primarily focuses on the informed consent process.
Informed consent is guided by three main principles. First, the consent has been provided voluntarily. Second, the participants can withdraw their consent at any given time. Third, in case the participant has withdrawn their consent, they are also free to withdraw the information or data that had already been collected. The researcher provides full information concerning the study and explains to the respondent the importance of the study and why it is imperative for the respondents to take part in the study (Creswell & Poth, 2016). The full information is provided in order for the participants to make informed decisions about their participation in the study.
The voluntary consent means that the participants accept to participate in the study in accordance with their values, preferences, and wishes (Grove & Gray, 2015). Providing the respondents with an opportunity to participate in the study voluntarily is one of the ways through which the researcher indicates respect for human dignity during the study. In this study, the due process of ensuring that the participants have consented to participate in the study without coercion, undue influence, or incentives is followed to the letter. The informed consent is detailed and contains all the requirements as indicated in the appendix.
However, before conducting the study, all the procedures are followed as a minimum requirement of the institution. In other words, ethical requirements including the permission to conduct the study by the institution, provision of consent forms to the participants, as well as assurance firms for the protection of the respondents and the information provided, have been conducted before the start of the study. Essentially, all the ethics approval processes are undertaken before the commencement of the study in order to protect the researcher and the respondents.
One of the aspects of ethical research is the protection of participants from harm (Polit & Beck, 2017). The only anticipated harm that might be experienced is psychological discomfort associated with the questions of the interview. The main mechanisms of protection include the fact that the participants can refuse to answer specific questions or withdraw from the study at any time. Additionally, a free or low-fee counseling hotline number is provided.
Summary
This chapter describes the methodology for the dissertation. The qualitative research approach mainly guides the process of data collection and analysis. It describes the research design, instrumentation, and data analysis procedures. Since human subjects provide information for the study, there is a keen emphasis on observing all ethical considerations related to their involvement in research.
Results
Introduction
The present study is devoted to the experience of hysterectomies in Mississippi women in the absence of informed consent law. The purpose consists of exploring the topic by focusing on the attitudes, beliefs, perceptions, and other ideas that would emerge from the interviews with the participants. The research questions are concerned with the perceptions of the women and the themes which emerge from their experiences. This chapter will describe the pilot interviews, settings, and data collection and analysis procedures, as well as the demographics and other results together with their trustworthiness, to respond to the research questions.
Pilot Study
The pilot study involved two African-American women aged between 30 and 40 years. They were recruited via emails sent by the leader of the support group on behalf of the researcher. The researcher and participants met in a private room of a public library for the consent procedures (Appendix B) and interviews. The pilots demonstrated that the anticipated timeframe for the interviews was correct; also, it proved the ability of the interview questions (Appendix A) and demographics survey (Appendix C) to provide the necessary information for the study. The pilot interviews yielded no need for changes in the interview questions, and they established the feasibility of the study.
Setting
The setting of the interviews was not changed; the private room in the public library was employed to ensure confidentiality. However, only eight of the participants were recruited from the support group; the rest were contacted by other participants who directed the recruitment email to their acquaintances. The recruitment strategy was changed to achieve the desired sample size. No women commented on the effect of the setting on them; when asked if they were comfortable with the settings, all of them agreed. No women demonstrated visible signs of distress, and none of them requested a referral to support services. Also, no women asked to stop the interviews, and none of them withdrew from the study citing discomfort. Overall, based on the researcher’s observations and reports of the women, it can be suggested that the experience was not traumatic for the women, and the settings were not likely to affect their responses in any negative way.
Demographics
The demographic data were gathered with the help of the demographics survey (Appendix C). The study managed to recruit only African Americans and Caucasians; seven of the ten participants were African American (Figure 1). Figure 2 demonstrates that at the time of the interview, most of the women were 30-40 years old. Many of them had a bachelor’s or master’s degree (Figure 3); most were married (Figure 4).
As for hysterectomy data, Figure 5 shows that most of the participants (six women) underwent their hysterectomy at the age of 20-30 years. None of them had a master’s degree at the time of their hysterectomy; mostly, they had a college-level education (Figure 6). Regarding the marital status, not much has changed for the participants since their hysterectomy; most of them were married at the time.
Data Collection
For the analysis, the pilot interviews were excluded, and the information was gathered from the sample of ten people, which is the number of participants that the study initially planned to recruit. Figure 7 depicts the marital status of participants at the time of hysterectomy. All the participants participated in interviews that used the interview question tool (Appendix A). The interviewees were also asked to complete the demographics survey, which employed a specifically-developed tool (Appendix C). For each participant, the procedures were carried out only once; no follow-ups were intended for the study. All the data collection procedures took place in the private room of the public library as was planned.
The longest interview took a little less than an hour and a half; most often, the women finished sooner. The demographics survey took around five minutes in most cases. For the interviews, audio-recording was used, after which the files were transcribed by the researcher. For the demographics survey, printed-out questionnaires were employed, which were then manually converted to electronic formats (MS Word and MS Excel files). No actual variations in the data collection procedures took place, and no unusual events were registered during them except for some interviews being shorter than was anticipated which did not cause any problems.
Data Analysis
Data analysis was carried out by a Nvivo specialist who signed a confidentiality agreement to ensure the protection of the data (Appendix D). The analysis followed the steps that are common for thematic analysis and have been described by Clarke and Braun (2014). The process was inductive: it started with finding individual codes and reviewing the codes for patterns. The patterns were then refined by the specialist and the researcher to develop the categories and themes. The Nvivo software was used to keep track of all the data (Appendix E) and provided a comfortable means of storing and reviewing the patterns. Also, it enabled the development of hierarchy charts, which were employed to visualize the patterns and the frequency of their appearance.
The Nvivo results are presented in Appendix F as a table; the first column names the themes, categories, and codes, the second one states the number of participants who mentioned the unit, and the final one indicates the number of references to it. For example, if the number of participants is three and the number of references is four, it means that the theme was mentioned by three participants four times, which implies that one participant mentioned it twice.
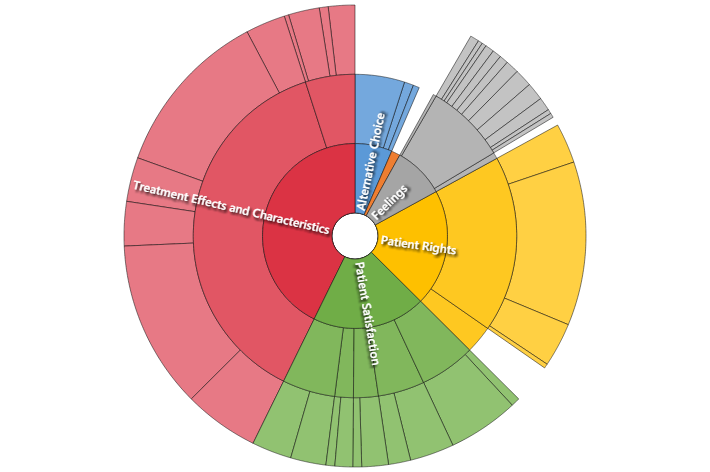
As can be seen from Appendix F, the data referred to a total of six general themes. In the table, they are presented in alphabetical order; Figure 8 indicates the frequency of their use by the participants. Most often, the participants focused on the outcomes of their treatment, as well as their satisfaction with it. Additionally, a major theme was related to the discussion of patient rights. The participants also reflected on their feelings and considered the possibility of the use of alternative treatment. Finally, a separate theme was concerned with the benefits that doctors might derive from disinformation; as believed by some of the participants, they were “taken advantage of or kept in the dark in order to put money in my doctor’s hands.”
Each of the themes included several categories and was associated with multiple codes as can be seen from the references. When considering alternative choices, one woman expressed no wish for alternative treatment, but the rest stated a desire to choose something different, and three of them also regretted not researching their options. In connection with this tendency, the women reported a wide variety of negative feelings, and only one of them described positive ones. Similarly, the treatment effects were divided into positive and negative ones with the latter category being noticeably more diverse and greater in volume. As pointed out by one of the participants: “I think I would have made a different choice due to the severity of the procedure and the negative outcomes such as hair loss, infertility, and vaginal dryness.”
The discussion of patient rights mostly revolved around the topic of informed consent, in which the participants considered the importance of this right: “we deserve to know the whole truth, not just the part that benefits the physician.” Additionally, they presented their experience of informed consent: “It would have been nice to know about other alternatives, but I wasn’t given that benefit.” Furthermore, many women referred to the right to choose: “My doctor took away my right to choose in order to pad his wallet.” In the discussion of their satisfaction with the operation, the women considered the problem of infertility, the complications, the processes and services, and outcomes. Overall, the data provided by the participants is sufficient for responding to the research questions as will be shown below.
Regarding discrepancies, it is difficult to claim that the data had any patterns which directly contradicted each other. For instance, different participants had dissimilar attitudes towards various complications and side effects of the treatment, but the fact that some women did not want to have more children while others did is not truly contradictory. Similarly, different levels of satisfaction and varied emotional responses are the reflection of diverse experiences and reactions to them; different people can be satisfied and dissatisfied with identical outcomes. No participants disputed the idea that the disinformation could have been caused by money-related concerns, and those that forwarded the claim made it clear that the idea was their personal opinion. Basically, the data consisted of individual views and feelings of the participants, which is why every case that somehow diverged from the general patterns was still included in the final table and incorporated into an appropriate category and theme.
Evidence of Trustworthiness
The trustworthiness of a qualitative study depends on several key dimensions (Polit & Beck, 2017), which were addressed during the stage of planning methodology for this study. The following strategies have been employed to ensure trustworthiness. The credibility of the results was achieved with the help of triangulation: in particular, the Nvivo specialist and researcher worked together to improve the quality of the identified themes. The same method also promoted confirmability: the two investigators checked each other’s results, making sure that the results represented the data provided by the participants. Furthermore, during the interviews, the researcher asked the participants if any questions needed clarifying, which also promoted confirmability and the ability of the data to reflect the voice of the interviewees.
Transferability was promoted by engaging people of different ages and races in the project; however, the limitations of the study’s sample have been considered, and the research makes an effort to avoid the conclusions that cannot be derived from the information gathered. The primary dependability strategy is related to the application of the data collection tool: it was devised to ensure the consistency of responses, and the data analysis showed that this outcome was achieved (no inconsistencies in the data were found). Therefore, it can be assumed that the results of the study could be replicated. Additionally, the study presents its methodology in detail, which is why it would be easy to carry out again. Thus, several trustworthiness strategies have been employed in the study to ensure the high quality of its results, and they did not change since the planning stage.
Results
The findings of the study can directly respond to its research questions. They detail the perceptions of the women who experienced a hysterectomy without a comprehensive informed consent law, as well as other themes that emerge from their narratives. Since the questions focus on the themes, it is logical to arrange this chapter around the established patterns (Appendix F).
The topic of patient rights reflected the way women perceived the lack of information in their hysterectomy consent procedures. Figure 9 demonstrates that most women experienced some form of lack of information; a few reported having no information at all, and some stated that they did not have enough information about hysterectomy or other options. Many women specifically noted that they were informed about the option of not performing the procedure, and a few also explicitly stated that they wanted more information. Basically, only one woman said that she had all the information she wanted (incomplete as it could be); the rest agreed that “it would have been very beneficial to know everything.” The women generally supported the idea of the importance of informed consent (“we deserve to know the whole truth”) and mentioned the right to choose, which the lack of information deprived them off (“we have a right to know everything there is to know about surgical procedures so that we can make an informed decision”). Thus, the first theme covered the problem of the lack of informed consent in the experiences of the majority of the interviewed women in this regard.
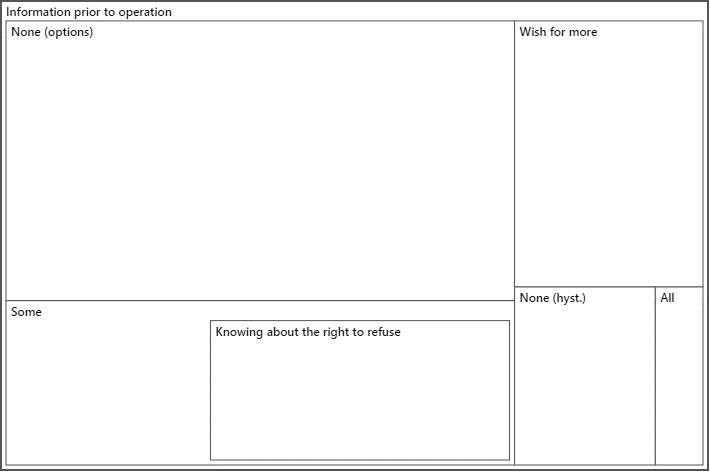
Consequently, one of the major themes discussed by the participants was the wish to change their decision. The primary element of this theme consists of the participants’ belief that if they had been provided with all the necessary information, they would have chosen something other than hysterectomy. Some of the women described hysterectomy as “the last choice” or “the last resort” (Figure 10). It should be pointed out that one of the women did not express regret; however, she also expressed the belief that she was provided with all the information that she needed. Thus, the women who were not satisfied with the provided information also expressed the wish to change their choice.
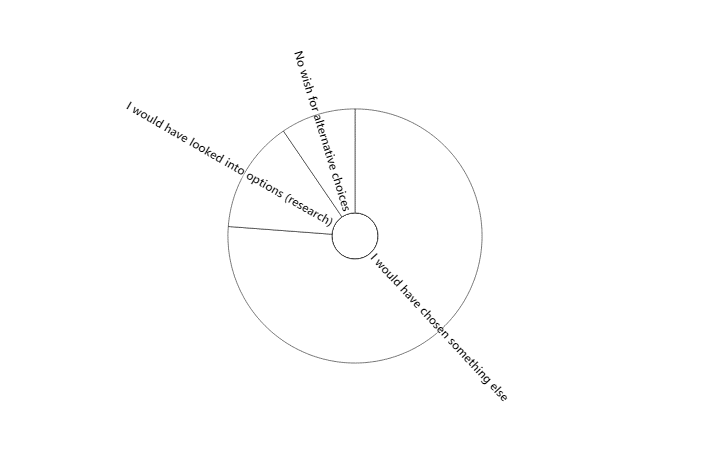
The women’s narratives also revolved around the topics of the effects of the treatment and the satisfaction with it. The latter topic is the one that has the most varied results: the women perceived their experiences rather differently, which is why there were reports of both satisfaction and dissatisfaction (Figure 11). Even when discussing the topic of infertility, two of the women stated that they were satisfied with the reality of not having more children, but for the majority, the change in their fertility was problematic. Furthermore, many women commended the quality of the service provided to them, but they also noted issues, which decreased it. Many women were dissatisfied with the processes and outcomes; some of them specifically attributed such attitudes to the lack of informed consent: “I wasn’t satisfied with neither the treatment process nor its outcomes because I didn’t know I had choices.”
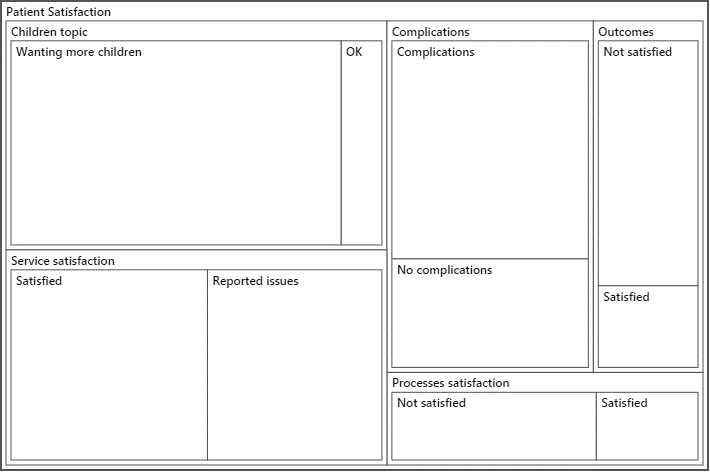
The effects of treatment were more uniform: despite the presence of positive outcomes (Figure 12), the majority of women reported negative ones and focused on them, referring to them more often (Figure 13).
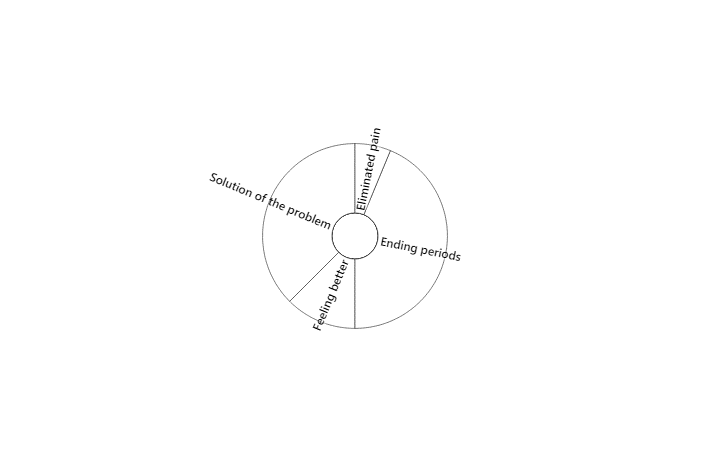
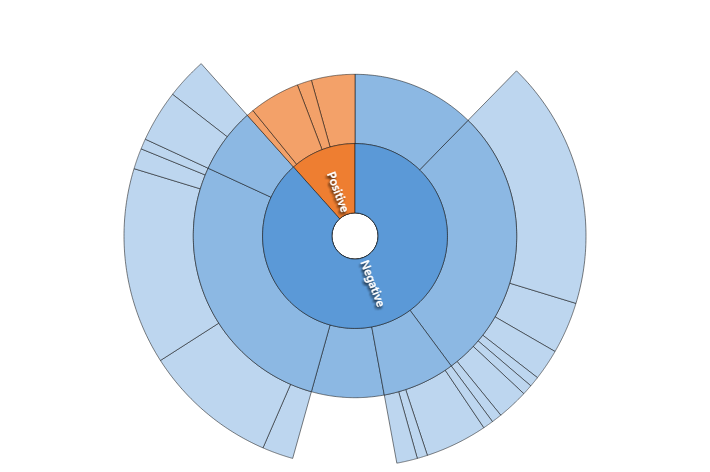
The negative outcomes were also more diverse and numerous (Figures 13 and 14). Again, the women who felt under-informed were more likely to report negative outcomes; the woman who was satisfied with the information provided to her briefly mentioned only three negative outcomes while the rest of the women discussed more issues and emphasized them several times. Furthermore, the well-informed woman reported no negative feelings. The under-informed women reported multiple and varied negative feelings, as well as bittersweet ones, including the feeling of being less attractive and being “less than a woman” (Figure 15). Thus, the perceptions of the under-informed women tended to be more negative than those of the well-informed ones.
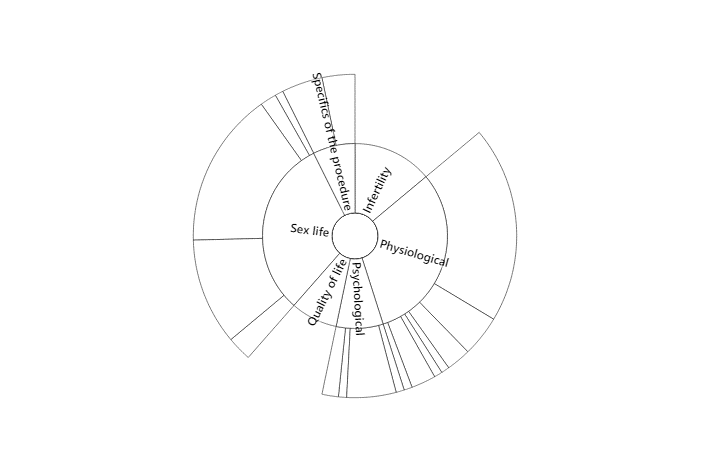
The final theme which emerged from the women’s interviews was that of the reasons for them being under-informed. According to them, doctors benefitted from misinforming them: “I believe my doctor intentionally withheld information from me just to get more money out of me”; “I feel like I got played just so the doctor or the hospital could reap the benefits of me paying lots of money for a surgery that I probably didn’t even need.” The women admit that this idea is subjective, but it is an important perception which indicates a pattern of distrust towards healthcare providers. One of the interviewees stated: “the surgery made me resent my doctor for not telling me everything there is to know about fibroids and hysterectomies.” This outcome is especially important for practice.
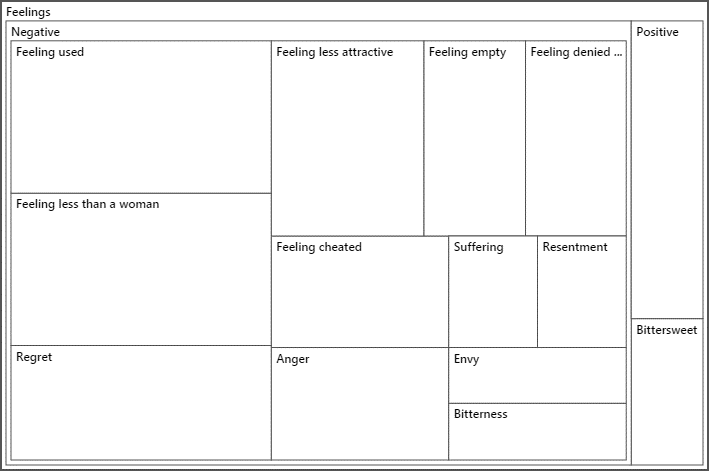
Regarding the discrepancies, only one of the respondents described their experience as predominantly positive, although she also noted some side effects of the procedure. It is noteworthy that she did not perceive the lack of information as problematic because she believed that she was provided with all the necessary information (she was informed about one alternative). She also did not think that she could be offered another solution. Regarding the rest of the women, even those of them who noted the positive outcomes of their surgery and believed that no other solution could fit their case still was dissatisfied with the lack of information and reported negative feelings as a result. Therefore, the discrepancy can be explained by the differences in perception: the woman who did not perceive the lack of information as problematic and believed that she was provided with sufficient information had no negative feelings. The only woman who was not dissatisfied with the amount of information provided to her still reported side effects but generally described the experience as a positive one.
Summary
The study’s findings respond to the research questions, indicating that multiple concerns emerge from the data provided by the interviewees. They include the wish to change the decision to undergo hysterectomy, the issues with informed consent, the negative outcomes of hysterectomies, and related feelings. The benefits of the procedure were also cited; one of the participants who did not view herself as misinformed had no negative impressions. Mostly, however, the participants perceived the hysterectomy experience negatively because they were under-informed. The implications of the research will be reviewed in the next chapter.
Discussion, Conclusions, and Recommendations
Introduction
The present qualitative study was conducted with the purpose of investigating the experiences of hysterectomies in Mississippi women in the absence of informed consent law. The goal was to explore and report the specifics of uninformed decision-making in the women who underwent hysterectomies. The findings of the study indicate that the hysterectomy perceptions of under-informed women tend to have negative patterns, including an emphasis on the negative outcomes of the procedure, negative emotions associated with it, and the wish to choose an alternative option. The women also reported the cases of being offered insufficient information or no information at all, and their trust in providers appears to have diminished. The present chapter will interpret the findings while considering their limitations and discuss the related implications and recommendations.
Interpretation of the Findings
The findings of the study are generally in line with the literature on the topic. In the absence of comprehensive informed consent law, the influence of healthcare providers on patient decisions was proven through the nine examples of them withholding information (Purcell et al., 2016). Hysterectomy was shown to be associated with important complications (including psychological and physiological ones), which caused the women to wish for a different choice after learning about the alternatives (Brohlet al., 2015; Darwish et al., 2014; Pendleton et al., 2016). The participants also acknowledged the positive outcomes of hysterectomy, especially its ability to resolve the causes of the surgery.
The reduced quality of life has been reported by most of the interviewees and supported by research (Ogburn, 2014; Power et al., 2015), but in the literature, there is also sufficient evidence to the opposite effect, that is, the improvement of the quality of life as a result of hysterectomy (Brohl et al., 2015). The fact that the persons with negative experiences are overrepresented in this study may be attributed to the specifics of the recruitment procedure, which searched for the women who were not provided with sufficient information before the surgery and, therefore, were more likely to regret it.
Thus, the findings support the idea that a comprehensive informed consent law would be beneficial because they indicate the issues associated with the lack of informed consent (Armijo-Olivo et al., 2014; Diamond, 2014; Miyata et al., 2014; Seagle et al., 2018). The study also provides the data relevant for Mississippi, extending the knowledge on the topic. Additionally, the demographics analysis shows that many of the under-informed women underwent the procedure at a relatively young age and with college-level education, and the African American women constituted the majority of the sample. However, the study does not offer enough data to support the related conclusions from the literature review, including the evidence of disparities or the effect of the level of education on hysterectomies.
The application of HMB to the results is insightful. HMB postulates that patient education is the key to fostering improved health behaviors and better health choices (Goodman, 2016; Lambert et al., 2017). In turn, the research’s findings demonstrate that the absence of information on healthy choices can make one’s experience and perceptions of hysterectomy negative. Furthermore, HMB considers the way individual perceptions affect one’s decision-making (Corace et al., 2016). Several of the women interviewed during the study noted that their perceptions of their options changed over time as they learned more about hysterectomy and its alternatives. Thus, the findings (as framed by HMB) once again highlight the importance of informed consent and patient education for satisfactory decision-making.
Limitations of the Study
Study limitations remain identical to the ones described in the prior chapters because the execution of the project did not differ much from its plans. The study’s sample remained rather small and specific; the responses of African American and White women from Mississippi were collected. However, the study did not intend to be generalizable; rather, it aimed to explore women’s experiences with hysterectomies in the absence of comprehensive informed consent, and this purpose was achieved. Similarly, the results could only provide women’s personal perspectives and ideas (subjective data), but the project aimed to gain this information. Therefore, the limitations of the study should be taken into account when interpreting the results, but they do not prevent the research from responding to its questions.
Recommendations
The study’s recommendations are concerned with the ways to explore the topic further. Given the sampling constraints, a detailed exploration of the women from other states and demographic groups can be developed. Furthermore, to make more generalizable conclusions about the experiences of Mississippi women, a study with a bigger sample could be helpful. Also, the present study did not intend to prove the relationships between the lack of informed consent and particular outcomes; for that, a quantitative (most likely, correlational) study would be necessary. Overall, the present study contains a general exploration of the topic; more specific, future investigations would provide more data for related policy changes.
Implications
The primary implications of the study are concerned with social change. It provides evidence that indicates that despite the acknowledgment of the importance of informed consent by the healthcare community, there are still instances in which the rights of patients are violated in Mississippi. Therefore, the significance of the introduction of various-level policies (from institutional to federal) which would cement the importance of comprehensive informed consent is highlighted. Additionally, the study supports the importance of providing sufficient information for decision-making in practice. No direct methodological or theoretical implications follow from the study, although it does lend some evidence to the ideas of HBM.
Conclusion
Dedicated to the exploration of the experiences of the women who underwent hysterectomies in the absence of comprehensive informed consent law, the present study can offer the following conclusions. Hysterectomy is a serious, invasive procedure, which can be justified in a few cases but can also have notable negative outcomes. Consequently, comprehensive informed consent is important with hysterectomy. However, the study demonstrates that the cases in which women are not provided with sufficient information to make their own decisions are still present. The women report negative outcomes and a wish to change their type of treatment; they also suspect that disinformation is beneficial for care providers, which affects patient-provider relationships. The results of the study highlight the significance of comprehensive informed consent, which is why it can be used to advocate for the introduction of comprehensive informed consent law.
References
Aarts, J. W., Nieboer, T. E., Johnson, N., Tavender, E., Garry, R., Mol, B. W. J., & Kluivers, K. B. (2015). Surgical approach to hysterectomy for benign gynecological disease. Web.
Abdulcadir, J., Tille, J. C., & Petignat, P. (2017). Management of painful clitoral neuroma after female genital mutilation/cutting. Reproductive Health, 14(1), 22-28. Web.
Ahmed, H. (2015). Risks of laparoscopic surgery. Obstetrics and Gynecology International, 3(4), 00089. Web.
Andersen, L. L., Ottesen, B., Møller, L. M. A., Gluud, C., Tabor, A., Zobbe, V.,… Toftager-Larsen, K. (2015). Subtotal versus total abdominal hysterectomy: Randomized clinical trial with 14-year questionnaire follow-up. American Journal of Obstetrics, & Gynecology, 212(6), 758-761. Web.
Antero, M. F., Shah, R., Burn, A., Hallisey, M., & Greene, J. (2016). A retrospective study on preoperative uterine artery embolization prior to hysterectomy [25E]. Obstetrics & Gynecology, 127, 49S. Web.
Armijo-Olivo, S., Ospina, M., da Costa, B. R., Egger, M., Saltaji, H., Fuentes, J.,… Cummings, G. G. (2014). Poor reliability between Cochrane reviewers and blinded external reviewers when applying the Cochrane risk of bias tool in physical therapy trials. PloS One, 9(5), e96920. Web.
Arnetz, J. E., Hamblin, L., Essenmacher, L., Upfal, M. J., Ager, J., & Luborsky, M. (2015). Understanding patient‐to‐worker violence in hospitals: A qualitative analysis of documented incident reports. Journal of Advanced Nursing, 71(2), 338-348. Web.
Arrigo, B. A., & Waldman, J. L. (2014). Psychological jurisprudence and the power of law: A critique of North Carolina’s Woman’s Right to Know Act. Duke Journal of Gender Law and Policy, 22, 55.
Baker, S. E., & Edwards, R. (2012). How many qualitative interviews is enough? Expert voices and early career reflections on sampling and cases in qualitative research. Web.
Bilandzic, A., Fitzpatrick, T., Rosella, L., & Henry, D. (2016). Risk of bias in systematic reviews of non-randomized studies of adverse cardiovascular effects of thiazolidinediones and cyclooxygenase-2 inhibitors: Application of a new Cochrane risk of bias tool. PLoS Medicine, 13(4), e1001987. Web.
Brixey, J. J., Brixey, J. E., Saba, V. K., & McCormick, K. A. (2015). Essentials of nursing informatics study guide. New York, NY: McGraw Hill Professional.
Brohl, A. S., Li, L., Andikyan, V., Običan, S. G., Cioffi, A., Hao, K.,… Maki, R. G. (2015). Age-stratified risk of unexpected uterine sarcoma following surgery for presumed benign leiomyoma. The Oncologist, 20(4), 433-439. doi:10.1634/theoncologist.2014-0361
Brown v. Mladineo, 504 So. 2d 1201 (1987).
Brown, J. (2017). Safe and sound: Vaginal hysterectomy with uncontained manual morcellation to effect uterine removal. Journal of Minimally Invasive Gynecology, 24(4), 511. Web.
Bruijn, A. M., Smink, M., Hehenkamp, W. J., Nijenhuis, R. J., Smeets, A. J., Boekkooi, F.,… Lohle, P. N. (2017). Uterine artery embolization for symptomatic adenomyosis: 7-year clinical follow-up using UFS-Qol questionnaire. Cardiovascular and Interventional Radiology, 40(9), 1344-1350.
Burgart, A. M., Strickland, J., Davis, D., Baratz, A. B., Karkazis, K., & Lantos, J. D. (2017). Ethical controversy about hysterectomy for a minor. Pediatrics, 139(6), e20163992.
Clarke, V., & Braun, V. (2014). Thematic analysis. In T. Teo (Ed.), Encyclopedia of Critical Psychology (pp. 1947-1952). New York, NY: Springer.
Collins, L. A. (2016). Knowledge, attitudes, and beliefs about preconception care among American adolescent females. Web.
Collins, S. K., Smith, B., Cheng, T., Hamner, K., Bolland, K., & Mcdougall, G. (2014). Barriers and incentives to breast cancer screening among African American and Caucasian women in the Mississippi Delta. Tuscaloosa, AL: University of Alabama.
Corace, K. M., Srigley, J. A., Hargadon, D. P., Yu, D., MacDonald, T. K., Fabrigar, L. R., & Garber, G. E. (2016). Using behavior change frameworks to improve healthcare worker influenza vaccination rates: A systematic review. Vaccine, 34(28), 3235-3242. Web.
Corona, L. E., Swenson, C. W., Sheetz, K. H., Shelby, G., Berger, M. B., Pearlman, M. D.,… Morgan, D. M. (2015). Use of other treatments before hysterectomy for benign conditions in a statewide hospital collaborative. American Journal of Obstetrics & Gynecology, 212(3), 304-206. Web.
Creswell, J. W., & Creswell, J. D. (2017). Research design: Qualitative, quantitative, and mixed methods approaches (5th ed.). Thousand Oaks, CA: SAGE Publications.
Creswell, J. W., & Poth, C. N. (2016). Qualitative inquiry and research design: Choosing among five approaches (4th ed.). Thousand Oaks, CA: SAGE.
Croce, S., Young, R. H., & Oliva, E. (2014). Uterine leiomyomas with bizarre nuclei: A clinicopathologic study of 59 cases. The American Journal of Surgical Pathology, 59(3), 19-24.
Danesh, M., Hamzehgardeshi, Z., Moosazadeh, M., & Shabani-Asrami, F. (2015). The effect of hysterectomy on women’s sexual function: A narrative review. Medical Archives, 69(6), 387-392. Web.
Darwish, M., Atlantis, E., & Mohamed-Taysir, T. (2014). Psychological outcomes after hysterectomy for benign conditions: A systematic review and meta-analysis. European Journal of Obstetrics, & Gynecology and Reproductive Biology, 174(1), 5-19. Web.
Deffieux, X., Vinchant, M., Wigniolle, I., Goffinet, F., & Sentilhes, L. (2017). Maternal outcome after abdominal packing for uncontrolled postpartum hemorrhage despite peripartum hysterectomy. PloS One, 12(6), e0177092.
DeJean, D., Giacomini, M., Simeonov, D., & Smith, A. (2016). Finding qualitative research evidence for health technology assessment. Qualitative Health Research, 26(10), 1307-1317.
DeJohn, P. (2014). Oregon surgery center is pioneer in outpatient hysterectomy.OR Manager, 30(8), 29-31.
Diamond, F. (2014). Highmark leads on procedure but other plans slow to follow. Managed Care, 23(9), 5-10.
Dueholm, M., Langfeldt, S., Mafi, H., Eriksen, G., & Marinovskij, E. (2014). Re-intervention after uterine leiomyoma embolisation is related to incomplete infarction and presence of submucousleiomyomas. European Journal of Obstetrics, & Gynecology and Reproductive Biology, 178, 100-106. Web.
Emre, A., Akbulut, S., Yilmaz, M., & Bozdag, Z. (2014). An unusual cause of acute appendicitis: Appendiceal endometriosis. International Journal of Surgery Case Reports, 4(1), 54-57. Web.
Eysbouts, Y. K., Massuger, L. F. A. G., IntHout, J., Lok, C. A. R., Sweep, F. C. G. J., & Ottevanger, P. B. (2017). The added value of hysterectomy in the management of gestational trophoblastic neoplasia. Gynecologic Oncology, 145(3), 536-542.
Fylstra, D. L. (2015). Ectopic pregnancy after hysterectomy may not be so uncommon: A case report and review of the literature. Case Reports in Women’s Health, 7, 8-11. Web.
Gattinoni, L., & Giomarelli, P. (2015). Acquiring knowledge in intensive care: Merits and pitfalls of randomized controlled trials. Intensive Care Medicine, 41(8), 1460-1464. Web.
Gaudet, M. M., Gapstur, S. M., Sun, J., Teras, L. R., Campbell, P. T., & Patel, A. V. (2014). Oophorectomy and hysterectomy and cancer incidence in the Cancer Prevention Study-II Nutrition Cohort. Obstetrics, & Gynecology, 123(6), 1247-1255. Web.
Goodman, E. (2016). True to form: How to use foundation training for sustained pain relief and everyday fitness. New York, NY: HarperCollins.
Gouy, S., Saidani, M., Maulard, A., Faron, M., Bach-Hamba, S., Bentivegna, E.,… Morice, P. (2017). Is uterine preservation combined with bilateral salpingo-oophorectomy to promote subsequent fertility safe in infiltrative mucinous ovarian cancer? Gynecologic Oncology Reports, 22, 52-54. Web.
Greenberg, R. S., Daniels, S. T., & Flanders, D. W. (2015). Medical epidemiology: Population health and effective health care (5th ed.). New York, NY: McGraw Hill Professional.
Grigore, M., Ilea, C., Terinte, C., Sava, A., & Popovici, R. (2014). Heterologous type of malignant mixed Müllerian tumor of the uterus presenting as a vulvar mass. European Journal of Gynaecological Oncology, 35(4), 458-460.
Grove, S., & Gray, J. (2015). Study guide for understanding nursing research: Building an evidence-based practice (5th ed.). Philadelphia, PA: Elsevier Health Sciences.
Gupta, S., & Manyonda, I. (2014). Hysterectomy for benign gynaeological disease. Obstetrics, Gynaecology and Reproductive Medicine, 14(5), 135-140. Web.
Halder, S. K., Laknaur, A., Miller, J., Layman, L. C., Diamond, M., & Al-Hendy, A. (2015). Novel MED12 gene somatic mutations in women from the Southern United States with symptomatic uterine fibroids. Molecular Genetics and Genomics, 290(2), 505-511. Web.
Hampton, T. (2014). Use of morcellation to remove fibroids scrutinized at FDA hearings. The Journal of the American Medical Association, 312(6), 588.
Harris, J. A., Uppal, S., Kamdar, N., Swenson, C. W., Campbell, D., & Morgan, D. M. (2017). A retrospective cohort study of hemostatic agent use during hysterectomy and risk of post‐operative complications. International Journal of Gynecology, & Obstetrics, 136(2), 232-237. Web.
Heng, S., Stephens, A. N., Jobling, T. W., & Nie, G. (2016). Measuring PC activity in endocervical swab may provide a simple and non-invasive method to detect endometrial cancer in post-menopausal women. Oncotarget, 7(29), 46573. Web.
Huber, J. T., & Tu-Keefner, F. (2014). Health librarianship: An introduction. Santa Barbara, CA: ABC-CLIO.
John, M. M., Malekpour, F., Parithivel, V., & Goyal, V. (2014). Giant pedunculated hemangioma of the liver. The American Surgeon, 80(9), 259-260.
Khatib, R., Schwalm, J. D., Yusuf, S., Haynes, R. B., McKee, M., Khan, M., & Nieuwlaat, R. (2014). Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: A systematic review and meta-analysis of qualitative and quantitative studies. PloS One, 9(1), e84238. Web.
Koleli, I. K., Ozdogan, E., Sariibrahim,B., Ozturk, L. B., & Karateke, A. (2014). Prognostic factors affecting lymph node involvement in cervical cancer. European Journal of Gynaecological Oncology, 35(4), 425-428.
Kurita, K., Henderson, V. W., Gatz, M., John, J. S., Hodis, H. N., Karim, R., & Mack, W. J. (2016). Association of bilateral oophorectomy with cognitive function in healthy, postmenopausal women. Fertility and Sterility, 106(3), 749-756. Web.
Lambert, C. L. C., Azuero, A., Enah, C. C., & McMillan, S. C. (2017). A psychometric examination of an instrument to measure the dimensions of Champion’s Health Belief Model Scales for cervical cancer screening in women living with HIV. Applied Nursing Research, 33, 78-84. Web.
Laughlin-Tommaso, S. K., Khan, Z., Weaver, A. L., Schleck, C. D., Rocca, W. A., & Stewart, E. A. (2016). Cardiovascular risk factors and diseases in women undergoing hysterectomy with ovarian conservation. Menopause, 23(2), 121-128. Web.
Lee, E. J., Gurr, D., & Van Wye, G. (2017). An evaluation of New York City’s 2015 birth certificate gender marker regulation. LGBT Health, 4(5), 320-327. Web.
Loke, A. Y., Davies, L., & Li, S. F. (2015). Factors influencing the decision that women make on their mode of delivery: The Health Belief Model. BMC Health Services Research, 15(1), 274-285. Web.
Low, H. Y., Zhao, Y., Huang, K. S., Shen, H. P., Wu, P. J., & Tseng, C. J. (2017). Intravenous leiomyomatosis of the uterus: A clinicopathological analysis of nine cases and literature review. Taiwanese Journal of Obstetrics and Gynecology, 56(3), 362-365. Web.
Lubotzky, F. P. (2017). The development, pilot and randomised controlled trial of a psychosexual rehabilitation information booklet for women undergoing pelvic radiation therapy for gynaecological or anorectal cancer. New York, NY: GRIN Verlag.
Meij, E. V. D., & Emanuel, M. H. (2016). Hysterectomy for heavy menstrual bleeding. Women’s Health, 12(1), 63-69.
Miyata, H., Tsuji, N., Jimi, T., Butsuhara, Y., Terakawa, K., & Nagano, T. (2014). Adenosarcoma of the uterine body initially presenting as an interstitial small tumor of the uterus: A case report. European Journal of Gynaecological Oncology, 35(4), 473-476.
Morice, P. (2014). Impact of tumor morcellation during the surgical extraction of solid tumors. Bulletin du Cancer, 101(6), 526-527
Ogburn, T. (2014). Shared decision making and informed consent for hysterectomy. Clinical Obstetrics and Gynecology, 57(1), 3-13. Web.
Pallett, A., Phippen, N., Miller, C., & Barnett, J. (2016). Informed consent for hysterectomy: Does a video presentation improve patient comprehension? Obstetrics, & Gynecology, 127, 55S. Web.
Pendleton, A. A., Natarajan, A., Ahn, R., Nelson, B. D., Eckardt, M. J., & Burke, T. F. (2016). A qualitative assessment of the impact of a uterine balloon tamponade package on decisions regarding the role of emergency hysterectomy in women with uncontrolled postpartum haemorrhage in Kenya and Senegal. BMJ Open, 6(1), e010083.
Peng, Y., Chen, L., Wu, D. B., Hu, W. P., & Li, H. (2017). Analysis on 50 cases of emergency hysterectomy. Biomedical Research, 28(17), 7454-7457.
Polit, D.F., & Beck, C.T. (2017). Nursing research: Generating and assessing evidence for nursing practice (10th ed.). Philadelphia, PA: Lippincott, Williams & Wilkins.
Pop-Vicas, A., Johnson, S., & Safdar, N. (2017). Should cefazolin be the first-line antimicrobial prophylaxis choice in patients undergoing hysterectomy? A systematic review and meta-analysis. Open Forum Infectious Diseases, 4(1), 650. Web.
Power, T., Jackson, D., Carter, B., & Weaver, R. (2015). Misunderstood as mothers: Women’s stories of being hospitalized for illness in the postpartum period. Journal of Advanced Nursing, 71(2), 370-380. Web.
Purcell, C., Cameron, S., Lawton, J., Glasier, A., & Harden, J. (2016). Contraceptive care at the time of medical abortion: Experiences of women and health professionals in a hospital or community sexual and reproductive health context. Contraception, 93(2), 170-177. Web.
Reis, N., Engin, R., Ingec, M., & Bag, B. (n.d). A qualitative study: Beliefs and attitudes of women undergoing abdominal hysterectomy in Turkey. International Journal of Gynecological Cancer, 18(5), 921-928.
Rimbach, S., Holzknecht, A., Nemes, C., Offner, F., & Craina, M. (2015). A new in-bag system to reduce the risk of tissue morcellation: Development and experimental evaluation during laparoscopic hysterectomy. Archives of Gynecology and Obstetrics, 292(6), 1311-1320. Web.
Ringash, J., Waldron, J. N., Siu, L. L., Martino, R., Winquist, E., Wright, J. R.,… Hotte, S. (2017). Quality of life and swallowing with standard chemoradiotherapy versus accelerated radiotherapy and panitumumab in locoregionally advanced carcinoma of the head and neck: A phase III randomised trial from the Canadian Cancer Trials Group (HN. 6). European Journal of Cancer, 72, 192-199. Web.
Rizk, B., Fischer, A. S., Lotfy, H. A., Turki, R., Zahed, H. A., Malik, R.,… Herrera, D. (2014). Recurrence of endometriosis after hysterectomy. Facts, Views, & Vision in ObGyn, 6(4), 219.
Rosenstock, I. M. (1974). Historical origins of the health belief model. Health Education, & Behavior, 2(4), 328-335.
Ross, L. J. (2018). Teaching reproductive justice: An activist’s approach. In L. J. Rosset et al., Black women’s liberatory pedagogies (pp. 159-180). Cham, Switzerland: Palgrave Macmillan.
Roth, R., & Ainsworth, S. L. (2015). If they hand you a paper, you sign it: A call to end the sterilization of women in prison. Hastings Women’s LJ, 26, 7.
Saito, S., Kajiyama, H., Miwa, Y., Mizuno, M., Kikkawa, F., Tanaka, S., & Okamoto, T. (2014). Unexpected ovarian malignancy found after laparoscopic surgery in patients with adnexal masses–a single institutional experience. Journal of Medical Science, 76(1-2), 83-90.
Sanchez, J. A., Barach, P., & Johnson, J. K. (2017). Surgical patient care: Improving safety, quality and value. New York, NY: Springer.
Sandberg, E. M., Hehenkamp, W. J., Geomini, P. M., Janssen, P. F., Jansen, F. W., & Twijnstra, A. R. (2017). Laparoscopic hysterectomy for benign indications: Clinical practice guideline. Archives of Gynecology and Obstetrics, 296(3), 597-606.
Schollmeyer, T., Elessawy, M., Chastamouratidhs, B., Alkatout, I., Meinhold-Heerlein, I., Mettler, L.,…Weigel, M. (2014). Hysterectomy trends over a 9-year period in an endoscopic teaching center. International Journal of Gynecology and Obstetrics, 126(1), 45-49. Web.
Seagle, B. L. L., Alexander, A. L., Strohl, A. E., & Shahabi, S. (2018). Discussing sarcoma risks during informed consent for nonhysterectomy management of fibroids: An unmet need. American Journal of Obstetrics, & Gynecology, 218(1), 103-e1-105-e1.
Seki, T., Yanaihara, N., Hirata, Y., Fukunaga, M., Tanaka, T., & Okamoto, A. (2014). Uterine endometrial carcinoma with trophoblastic differentiation: A case report with literature review. European Journal of Gynaecological Oncology, 35(4), 461-464.
Seror, J., Bats, A. S., Douay-Hauser, N., Nos, C., Bensaid, C., & Lecuru, F. (2014). Contributions of laparoscopic and robotic surgery in the treatment of uterine cancer. La Revue du Praticien, 64(6), 813-815.
Shen, Z. (2015). Cultural competence models and cultural competence assessment instruments in nursing: A literature review. Journal of Transcultural Nursing, 26(3), 308-321.
Simpson, H., & Augat, P. (2015). Experimental research methods in orthopedics and trauma. Stuttgart, Germany: Thieme.
Singh, S., Ryerson, A. B., Wu, M., & Kaur, J. (2014). Ovarian and uterine cancer incidence and mortality in American Indian and Alaska native women, United States, 1999-2009. American Journal of Public Health, 104(S3), S423-S432. Web.
Sirimusika, N., Peeyananjarassri, K., Suphasynth, Y., Wootipoom, V., Kanjanapradit, K., & Geater, A. (2014). Management and clinical outcomes of endometrial hyperplasia during a 13-year period in Songklanagarind Hospital. Journal of the Medical Association of Thailand, 97(3), 260-266.
Skinner v. Oklahoma, 316 U.S. 535.(1942).
Spatz, E. S., Krumholz, H. M., & Moulton, B. W. (2016). The new era of informed consent: Getting to a reasonable-patient standard through shared decision making. JAMA, 315(19), 2063-2064. Web.
Suwannarurk, K., Thaweekul, Y., Mairaing, K., Poomtavorn, Y., & Bhamarapravatana, K. (2014). Silent abnormal placentation linkage to peripartum hysterectomy: Thammasat University Hospital 6-year study. Journal of the Medical Association 97(5), 473-477
Tapper, A., Hannola, M., Zeitlin, R., Isojärvi, J., Sintonen, H., & Ikonen, T. (2014). A systematic review and cost analysis of robot-assisted hysterectomy in malignant and benign conditions. Journal of Obstetrics, & Gynecology and Reproductive Biology, 177(1), 1-10. Web.
Taylor, S. J., Bogdan, R., & DeVault, M. (2015). Introduction to qualitative research methods: A guidebook and resource. New York, NY: John Wiley, & Sons.
Theunissen, M., Peters, M. L., Schepers, J., Maas, J. W., Tournois, F., Suijlekom, H. A. V.,… Marcus, M. A. (2016). Recovery 3 and 12 months after hysterectomy: Epidemiology and predictors of chronic pain, physical functioning, and global surgical recovery. Medicine, 95(26), e3980. Web.
Tiwari, V. (2014). Calculating the true cost of robotic hysterectomy. Journal of the Healthcare Financial Management Association, 68(8), 80-85.
Vijaya, U. A., Patel, A., Purushothama, R. K., Mallesh, M., & Nagaraj, A. (2015). Peripartum hysterectomy: A limiting factor for procreative potential, & safe-motherhood: A 5 years retrospective study. Journal of Evolution of Medical and Dental Sciences, 4(71), 12277-12287. Web.
Wright, J. D., Tergas, A. I., Burke, W. M., Cui, R. R., Ananth, C. V., Chen, L., & Hershman, D. L. (2014). Uterine pathology in women undergoing minimally invasive hysterectomy using morcellation. JAMA, 312(12), 1253-1255.
Yildirim, Y., Ertas, I. E., Nayki, U., Ulug, P., Nayki, C., Yilmaz, I., … Solmaz, U. (2014). En-bloc pelvic resection with concomitant rectosigmoid colectomy and immediate anastomosis as part of primary cytoreductive surgery for patients with advanced ovarian cancer. European Journal of Gynaecological Oncology, 35(4), 400-407.
Yilmaz, O., Korkmaz, M., Jaroszewski, J. J., Yazici, E., Ulutas, E., & Saritas, Z. K. (2014). Comparison of flunixin meglumine and meloxicam influence on postoperative and oxidative stress in ovariohysterectomized bitches. Polish Journal of Veterinary Sciences, 17(3), 493-499.
Young, M. D., Plotnikoff, R. C., Collins, C. E., Callister, R., & Morgan, P. J. (2014). Social cognitive theory and physical activity: A systematic review and meta‐analysis. Obesity Reviews, 15(12), 983-995.
Yusuf, F., Leeder, S., & Wilson, A. (2016). Recent estimates of the incidence of hysterectomy in New South Wales and trends over the past 30 years. Australian and New Zealand Journal of Obstetrics and Gynaecology, 56(4), 420-425. Web.
Zafar, S. M. A., Iqbal, J., Javed, N., Noor, S., & Niaz, A. (2017). Total laparoscopic hysterectomy at tertiary care hospital: Minimal risk of complications: Cross sectional study. Journal of the Society of Obstetrics and Gynaecologists of Pakistan, 7(2), 61-64.
Zhang, C., Havrilesky, L., Broadwater, G., Di Santo, N., Ehrisman, J., Lee, P., …Valea, F. (2014). Relationship between minimally invasive hysterectomy, pelvic cytology, and lymph vascular space invasion: A single institution study of 458 patients. Gynecologic Oncology, 133(1), 211-215.Web.