Surgical site infections (SSIs) are among the most common causes of postoperative illness. According to Heuer and Kossick (2017), SSIs account for nearly $3.5 to $8 billion per year due to prolonged recovery and up to 11 times longer hospital stay. However, about 60% of all SSI cases are preventable (Heuer & Kossick, 2017). Along with the provision of a clean and sterile surgical site and adequate tissue oxygenation, preoperative antibiotic prophylaxis is one of the most frequently used procedures aimed to reduce the incidence of SSIs. The majority of the US hospitals administer cefazolin. Therefore, the paper will be devoted to the design of a Clinical Decision Support System (CDSS) for the cefazolin use.
Cefazolin belongs to the first generation of cephalosporins. It is cheap compared to many other remedies. It is safe and has minimal side effects. Moreover, its pharmacological properties and dynamics have been sufficiently studied (Heuer & Kossick, 2017). The antibiotic agent has a direct impact on the targeted bacteria “by inhibiting the cell wall synthesis instead of interrupting its reproduction” (Heuer & Kossick, 2017, p. 294). The evidence shows that cefazolin is primarily effective against gram-positive aerobic microorganisms, such as staphylococci and streptococci (Heuer & Kossick, 2017). As stated by Okumura, Veroneze, Burgardt, and Fragoso (2016), for prophylaxis, healthcare providers mainly utilize 2 grams of cefazolin. However, since the efficiency of the agent depends on multiple physiological indicators of patients, as well as the nature of bacterial species, the dosage should be modified based on such criteria as patients’ age and weight.
Although cefazolin has good SSI preventive qualities, it has often been used inappropriately in many clinical settings. Okumura et al. (2016) note that “inadequate use of antimicrobial agents is associated with higher healthcare expenditures, microbial selection, resistant species prospection and other negative clinical outcomes” (p. 717). Therefore, the design of CDSS that will support effective and cost-efficient cefazolin administration is essential.
Since 2005, computerized provider order entry (CPOE) systems started to use algorithms to guide surgical prophylaxis prescriptions and cefazolin administration (Okumura et al., 2016). CPOE-based CDSS can be defined as software designed to assist clinical decision-making in which individual characteristics of patients are matched to a computerized clinical knowledge base. The CDSS provides all patient-specific assessments and recommendations to a healthcare provider to support his or her decision, i.e., selection of a particular drug dosage strategy. As stated by Spaulding and Raghu (2014), since CDSSs implies encoding of clinical workflows, they have the potential to significantly reduce prescribing errors and drug doubling incidents and result in better health processes and improved individual patient care.
When speaking of an algorithm for cefazolin administration, it should include various decision options for each particular prophylaxis scenario. For every patient, dosing strategies, treatment duration, and intervals of administration must be manually prescribed and entered into the system based on individual demographic and physiological features, i.e., age, renal injuries, and BMI (Okumura et al., 2016). Considering that cefazolin has the distinct minimum inhibitory concentration for every bacterial species, the dosage and re-dosing intervals should be different for S. aureus (0.25 to 1 pg/mL), Escherichia coli (1.0 to 4.0 pg/mL.20), and other microorganisms as well (Heuer & Kossick, 2017).
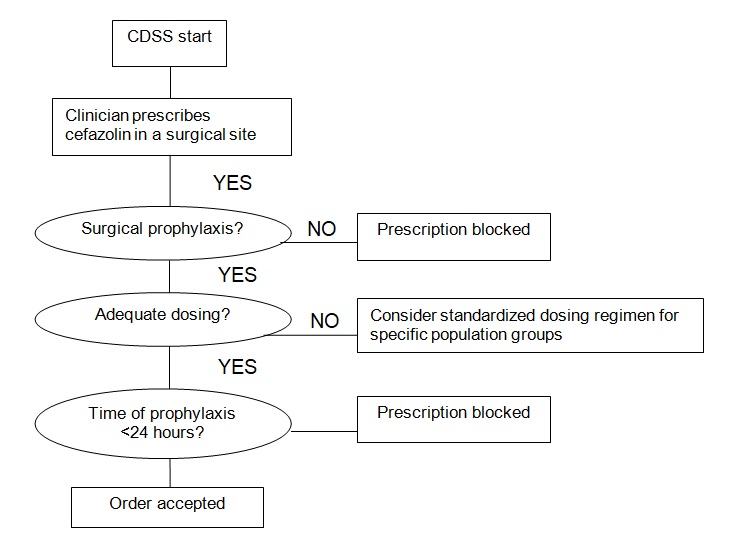
It is worth noticing that along with dosing and administration intervals, it is essential to consider the factor of drug-to-drug interactions (at the “Adequate dosing” stage). Warfarin and furosemide can have a moderately and highly clinically significant interactions with the antibiotic agent. As noted by Baillargeon et al. (2012), the combination of warfarin with cefazolin significantly increases the risks of bleeding. Therefore, it is important to consider these peculiarities when choosing the drug administration strategy for patients with such conditions as deep vein thrombosis and pulmonary embolism who intake warfarin.
During the implementation stage, when a healthcare practitioner will enter the cefazolin prescription, the system will provide real-time alerts based on the proposed algorithm. The types of alerts will include such categories as dosage, renal dose adjustment, drug-to-drug interactions, and duplicate therapy. According to these alerts, the clinician may either change the prescription or override the alert providing a rationale for doing so in a pull-down menu on the computer screen (Zenziper et al., 2014). During the initial phase in the algorithm adoption process, the alerts will be saved and assessed by the system administrator and knowledge engineers. Based on the assessment data, the CDSS will be adjusted and alerts will be customized according to specific hospital needs, i.e., cost efficiency, better patient safety, etc.
Although CPOE/CDSS can help hospitals gain multiple benefits including greater procedural standardization, better patient safety, and reduced process costs, there are still multiple barriers to its adoption (Spaulding & Raghu, 2014). In the case of the proposed CDSS for cefazolin use, the obstacles may include the lack of training, the lack of compliance with the CDSS, deficiencies in the current medical error reporting system, as well as a general resistance to change. Since the given barriers can potentially undermine clinical workflows and result in information loss and unclear and biased record of the CDSS implementation outcomes, the hospital administration should aim to develop an adequate organizational culture and infrastructure in order to provide support for the personnel and enforce the compliance with the CDSS. For this reason, before the CPOE implementation, all involved healthcare practitioners should be provided with comprehensive training and instructed on the CDSS-related practical benefits in order to decrease the resistance to change.
Additionally, Andersson Hagiwara et al. (2014) observe that a poorly developed CDSS can potentially produce harm. For instance, the researchers state that if an interface is unclear or irrational, it can results in multiple errors even when utilized by experienced users (Andersson Hagiwara et al., 2014). Thus, to facilitate system integration, all CDSS alerts must be simple, straightforward, and specialized in the selected area of performance (Moja et al., 2014). In this way, it will be possible to reduce ambiguity and consequent errors. Along with this, Brunette et al. (2013) state that one of the primary complaints of physicians using CDSS is the slow reaction of the software to their manipulations (e.g., mouse clicks, screen changes, etc.). Since it can significantly reduce the speed of prescription order and the quality of patient communication, the hospital should improve the technological infrastructure and its maintenance to increase the efficiency of the electronic health record system and minimize the risk for communication breakdown.
The findings of the literature review indicate that the CPOE/CDSS is a highly valuable technique that can substantially facilitate the selection of the best evidence-based decision regarding a particular patient’s need. The CDSS introduced in the given paper aims to support clinical decision making in cefazolin administration for surgical prophylaxis and prevention of SSIs. A six-step algorithm and the inclusion of four major types of alerts are suggested for this purpose. It can be argued that with effective integration of the CDSS, the hospital may significantly reduce the rate of medical errors related to drug administration and polypharmacy. However, to achieve a greater result, it is required to provide an appropriate organizational culture and support system encouraging clinicians’ compliance with a change initiative and fostering better technological operation.
References
Andersson Hagiwara, M., Suserud, B.-O., Andersson-Gäre, B., Sjöqvist, B.-A., Henricson, M., & Jonsson, A. (2014). The effect of a Computerised Decision Support System (CDSS) on compliance with the prehospital assessment process: Results of an interrupted time-series study. BMC Medical Informatics and Decision Making, 14, 70.
Baillargeon, J., Holmes, H. M., Lin, Y., Raji, M. A., Sharma, G., & Kuo, Y. F. (2012). Concurrent use of warfarin and antibiotics and the risk of bleeding in older adults. The American Journal of Medicine, 125(2), 183–189.
Brunette, D. D., Tersteeg, J., Brown, N., Johnson, V., Dunlop, S., Karambay, J., & Miner, J. (2013). Implementation of computerized physician order entry for critical patients in an academic emergency department is not associated with a change in mortality rate. Western Journal of Emergency Medicine, 14(2), 114–120.
Heuer, A., & Kossick, M. A. (2017). Update on guidelines for perioperative antibiotic selection and administration from the Surgical Care Improvement Project (SCIP) and American Society of Health-System Pharmacists. AANA Journal, 85(4), 293-299.
Moja, L., Liberati, E. G., Galuppo, L., Gorli, M., Maraldi, M., Nanni, O., … Kwag, K. H. (2014). Barriers and facilitators to the uptake of computerized clinical decision support systems in specialty hospitals: Protocol for a qualitative cross-sectional study. Implementation Science, 9, 105.
Okumura, L. M., Veroneze, I., Burgardt, C. I., & Fragoso, M. F. (2016). Effects of a computerized provider order entry and a clinical decision support system to improve cefazolin use in surgical prophylaxis: A cost saving analysis. Pharmacy Practice, 14(3), 717.
Spaulding, T. J., & Raghu, T. S. (2014). Impact of CPOE usage on medication management process costs and quality outcomes. Inquiry (United States), 50(3), 229-247.
Zenziper, Y., Kurnik, D., Markovits, N., Ziv, A., Shamiss, A., Halkin, H., & Loebstein, R. (2014). Implementation of a Clinical Decision Support System for computerized drug prescription entries in a large tertiary care hospital. Israel Medical Association Journal, 16(5), 289-294.