Introduction
Colorectal cancer is among the most common cancers across the world. It starts either in the rectum or colon, and its naming depends on where it starts. Rectal and colon cancers are usually grouped because they have numerous common features. Due to this, they have the same screening tests that allow early pathology detection and ensure early intervention before it progresses further. Additionally, early detection provides a better prognosis leading to a quality of life for patients (Davidson et al., 2021). Colorectal cancer screening is recommended by the United States Preventive Services Task Force (USPSTF) as an effective way to reduce disease-related morbidity and mortality. In general, colorectal cancer screening ensures early detection of the disease and treatment before it becomes severe.
Numerous screening tests can be used to detect colorectal cancer. Stool tests, flexible sigmoidoscopy, colonoscopy, and CT colonography are among the screening strategies recommended by the USPSTF. Doctors usually provide which screening test is best for a patient, depending on their medical history (Qaseem et al., 2019). Colorectal cancer screening is an applicable initiative to the community because recommendation testing provided by USPSTF targets individuals at a higher risk of being infected by cancer.
Population Screening Purpose
The grade A given by the USPSFT is Colorectal cancer screening is recommended for all persons aged 50 to 75 years. In 2022 the U.S has so far recorded 151 030 new cases of colorectal cancer (Ho et al., 2022). Generally, the number of people diagnosed with colorectal has been dropping since the 1980s because more people are getting checked and making lifestyle changes to reduce their risk factors. Currently, the lifetime risk of developing cancer is 4% for women and 4.3% for men. This clearly shows that men are more likely than women to develop colorectal cancer during their lives. Lifestyle-related factors such as exercise, diet and weight have the capability of causing the development of colorectal cancer.
Most people diagnosed with colorectal cancer are above 50, and the risk increases with age. Due to this, the screening test will include both men and women with the range of 50 to 75 years. This screening is done due to strongly recommended by the USPSFT. The screening will be conducted in the lower Mississippi Delta because it is one of the hotspots where people above 50 years can develop cancer (Lauby-Secretan et al., 2018). The vulnerability in Mississippi Delta is caused by the highest poverty rate experienced in the region. Due to this, most people in the area cannot afford an appropriate diet, which is one of the factors that cause colorectal cancer. Therefore, screening about 50% of the region’s population, there is a possibility that 20% of the screened people will have colorectal cancer.
Setting
The screening event will be held at the Medical Center from 8:00 am to 1:00 pm on 1/06/2022. The reason for choosing this venue is that it receives numerous patients within the strongly recommended age of 50-75 years. Additionally, the place is easily accessible to all people within the region (Davidson et al., 2021). When the screening tests are located at the Medical Center, testing will be evenly distributed within the area. Generally, this venue is the perfect place to ensure that credible research will be done.
Screening Activity
Screening activity will involve educating patients about risk factors of colorectal cancers such as aging, family history, genetic syndrome and inflammatory bowel disease. Additionally, individuals within 50 to 75 years will be informed since they are at risk of developing colorectal cancer; routinely screening will reduce their threats. In most cases, precancerous polyps are the starting point of colorectal cancers (Ho et al., 2022). Since the abnormal growths do not show cancer symptoms, screening can detect them early to ensure they are removed before turning into cancer. Hence, sharing this information with people attending the screening will increase the numbers and times they get screened.
All the screening measures recommended by the USPSF will be used during the exercise. First, stool tests will involve guaiac-based chemicals and fecal immunochemical antibodies to detect blood in the stool. Second, doctors will use flexible sigmoidoscopy to check for cancer in the bottom portion of the colon and rectum by inserting a short, thin, flexible, lighted tube into the rectum. This is usually done within the range of 5 to 10 years (Lauby-Secretan et al., 2018). Third, colonoscopy is identical to flexible sigmoidoscopy, except that it is performed every 10 years and involves a longer, thin, flexible lighted tube. Finally, CT colonography will involve doctors creating images of the entire colon using computers and X-rays to see if there are any abnormal growths.
A colonoscopy test is required to complete the measurement procedure when stool tests, CT colonography, and flexible sigmoidoscopy show abnormal or positive results. However, colonoscopy is not required if either three tests show normal results. When a patient is diagnosed, doctors recommend radiation, surgical and medical treatments depending on the patients’ medical history and status (Qaseem et al., 2019). After treatment, patients expect outcomes such as surviving more than 10 years, being cured and changing lifestyles that can cause cancer again.
Cost Analysis
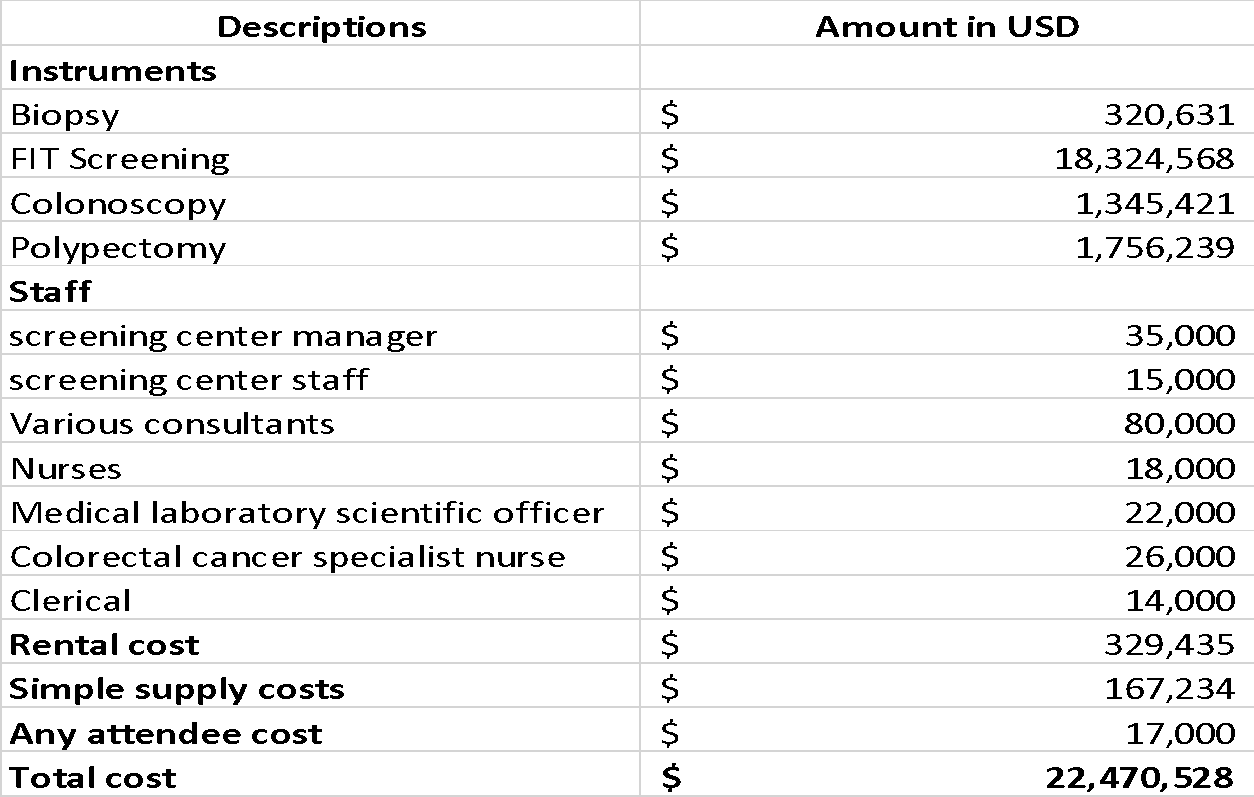
Table 1: Cost Analysis to Perform Colorectal Cancer Screening
Conclusion
Although colorectal cancer is among the leading cancers that cause numerous deaths annually, it can be cured. The cancer is common in older people who are above 50 years. Due to this, the USPSFT has strongly recommended that people within 50 to 75 years should have routinely screening for the disease. This helps them to detect cancer early before it is severe. The increased number of people screened has led to decreased number of people developing colorectal cancer.
References
Davidson, K., Barry, M., Mangoine, C., Cabana, M., Caughey, A., Davis, E., Donahue, K., Doubeni, C., Krist, A., Kubik, M., Li, L., Ogedegbe, G., Owens, D., Pbert, L., Siverstein, M., Stevermer, J., Tseng, C. and Wong, J. (2021). Screening for colorectal cancer. JAMA, 325(19), 1965. Web.
Ho, C., Zhao, Z., Chen, X., Sauer, J., Saraf, S., Jialdasani, R., Taghipour, K., Sathe, A., Khor, L., Lim, K. and Leow, W. (2022). A promising deep learning-assistive algorithm for histopathological screening of colorectal cancer. Scientific Reports, 12(1). Web.
Lauby-Secretan, B., Vilahur, N., Bianchini, F., Guha, N., & Straif, K. (2018). The IARC perspective on colorectal cancer screening. New England Journal Of Medicine, 378(18), 1734-1740. Web.
Qaseem, A., Crandall, C., Mustafa, R., Hicks, L., & Wilt, T. (2019). Screening for colorectal cancer in asymptomatic average-risk adults: A guidance statement from the American College of Physicians. Annals Of Internal Medicine, 171(9), 643. Web.