Introduction
Congestive heart failure (CHF) is one of the major health concerns in the United States. Once a patient is offered proper treatment, he or she is expected to embrace a new lifestyle with a proper diet and physical exercise among others. According to Leppin et al. (2014), the lack of proper care for such patients and inadequate post-discharge follow-ups are to blame for the increasing cases of readmission of such patients. Cases of readmission not only overburden the medical staff but also put financial pressure on the patient. As such, it has been of interest to medical practitioners to find ways of addressing the problem. The telehealth monitoring system offers a perfect platform through which this problem can be addressed.
Change Model Overview
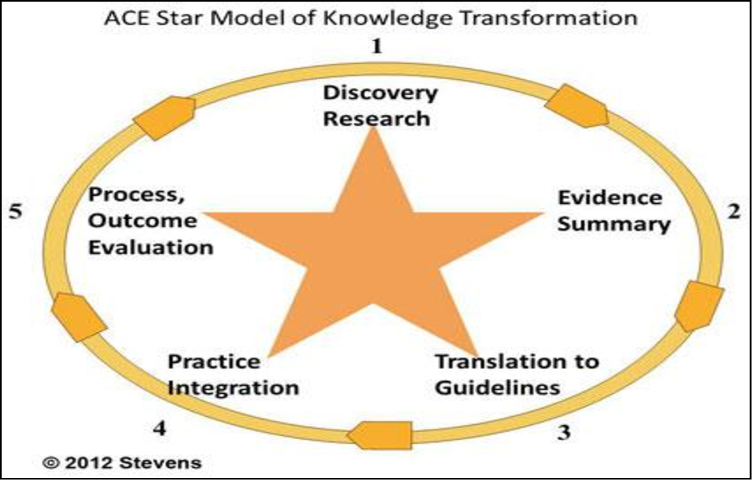
ACE Star Model, also known as the Star Model of Knowledge Transformation, is a concept used widely to support evidence-based practice (EBP) (Fry et al., 2015). Bhatt (2016) defines the model as “a simple, parsimonious depiction of the relationships between various stages of transformation, as newly discovered knowledge is moved into practice,” (p. 56). Shown figure 1 below, outlines five stages that must be observed in evidence-based practice. It starts with discovery through research, evidence summary, translation into guidelines, practice integration, and finally, evaluation of the outcome (Fernández-Llatas, Meneu, Traver, & Benedi, 2013). Nurses should use this process to facilitate change because it outlines simple but specific steps that should be taken to realize the desired outcome.
Define the Scope of the EBP
Readmission of congestive heart failure patients is a major problem in the United States because it exerts pressure on medical practitioners in the country. According to research conducted by Bhatt (2013), 20% of such patients are readmitted within 30 days of being discharged. The statistics also show that 50% of such patients end up being readmitted within six months of being discharged. This problem has a significant impact on healthcare because of the kind of burden it exerts on hospital facilities and medical staff.
Stakeholders
In this project, a team of medical practitioners will be needed to ensure that the goals set are realized. The stakeholders will include primary care physicians, heart failure nurses, cardiologists, pharmacists, dieticians, community nurses, and occupational therapists. Each of them will have specific roles to play.
Responsibilities of Team Members
The chosen members are important in this project because of their expertise when it comes to handling congestive heart failure patients. Primary care physician assesses the condition of the patient as soon as they are admitted to the hospital before referring him or her to a specific specialist. Heart failure nurse performs tests, counseling, and offers care to patients. Cardiologist ensures that relevant medical tests are conducted and proper treatment offered. The pharmacist offers the relevant medication for the patient, while the dietician defines food that the patient should take/avoid. Community nurse provides care at home or in the hospital when necessary, while the occupational therapist helps in-hospital recovery.
Evidence
The internal search revealed that cases of readmission are common despite the effort made by different stakeholders to reduce them. Quality improvement records and clinical practice guidelines at the institution emphasize the need to find a lasting solution to the problem, which proves that cases of hospital readmissions are still common.
Summarize the Evidence
The article by Leppin et al. (2014) shows that the use of a telehealth monitoring system can significantly reduce cases of readmission among patients with congestive heart disease. Their condition can be monitored remotely to determine whether they are making a proper recovery.
Develop Recommendations for Change Based on Evidence
Based on the analysis of the problem and findings made by scholars in this field, it is necessary to implement the telehealth monitoring program. Every stakeholder should understand his or her role in ensuring that CHF patients are properly managed after being discharged to eliminate or significantly reduce the need for readmission.
Translation
Action Plan
When implementing this plan, the identified stakeholders will be required to play their different roles dutifully. Once a patient is discharged, the community nurse will be responsible for monitoring his or her condition remotely. The nurse will be required to communicate with the patient regularly and if necessary, make physical visits. In such visits, she will record any changes in the condition of the patient and make a consultation with the relevant officers in the team. The nurse can change the medication if necessary. The pilot program will take six months. The method of evaluation of the outcome will be determining the rate of hospital readmissions within the period.
Process, Outcomes, Evaluation, and Reporting
The desired outcome is to reduce cases of readmissions of CHF patients by 85%. The outcome will be measured as discussed above and presented to the key stakeholders using graphs and charts to make it easy for them to understand the progress.
Identify Next Steps
The plan will be implemented on large scale by using steps embraced in the pilot program. The plan will be applicable to other units in the facility dealing with chronic health problems. To ensure that the implementation becomes permanent, it will be necessary to introduce relevant policies.
Disseminate Findings
The findings will be communicated internally using memos. The team will use official reports to communicate with external stakeholders and inform them about the findings.
Conclusion
It is critical for the local healthcare facilities to find ways of dealing with readmissions of CHF patients. The paper proposes the use of the ACE model of discovery, provide evidence, translation, integration, and evaluation when introducing and managing change.
References
Bhatt, D. L. (2016). Cardiovascular intervention: A companion to Braunwald’s heart disease. Philadelphia, PA: Elsevier.
Fernández-Llatas, C., Meneu, T., Traver, V., & Benedi, J.-M. (2013). Applying evidence-based medicine in telehealth: An interactive pattern recognition approximation. International Journal of Environmental Research and Public Health, 10(11), 5671–5682. Web.
Fry, D. E., Pine, M., Locke, D., Reband, A., Torres, Z., & Pine, G. (2015). Medicare inpatient and 90-day postdischarge adverse outcomes in carotid artery surgery. Surgery, 158(4), 1056-1064. Web.
Leppin, A. L., Gionfriddo, M. R., Kessler, M., Brito, J. P., Mair, F. S., Gallacher, K…. Montori, V. M. (2014). Preventing 30-day hospital readmissions. JAMA Internal Medicine, 174(7), 1095. Web.