African Americans are among the largest ethnic groups in the United States, with a greater percentage being of African ancestry, while some are of non-Black descent. This population descended from enslaved people from Africa coerced to work in the New World. Working as slaves, they had limited rights and were not entitled to an equal share in the economic, political, and social spheres of the country’s progress. Unfortunately, they continue to be subjected to systemic inequalities till the present day. The current paper seeks to focus on the health status of this group and decipher whether disparity prevails.
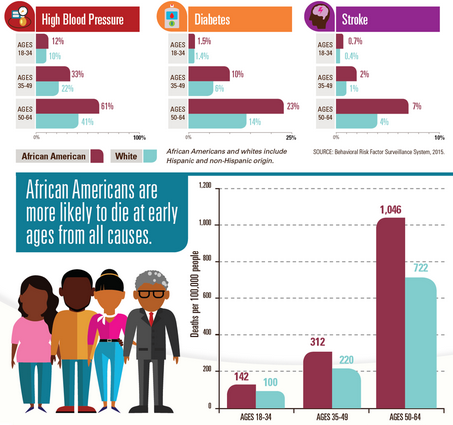
Even though the health status of African Americans has improved over the years, disparities with the health status of the White Americans continue to exist. The death rate has declined for older adults, but there are high morbidity and mortality rates among young adults for conditions which are typical among White Americans. The figure below illustrates this further, as obtained from the Centers for Disease Control and Prevention [CDC] (2017). Despite earlier mentioned improvements, Noonan et al. (2016) note that African Americans have the worst health status in the USA. Health People 2010 sought to address disparities in healthcare affecting this population, and deterioration was salient in mortality rates for neonates and post-neonates, HIV, coronary heart disease, cardiovascular disease among individuals with chronic kidney disease, and stroke (Noonan et al., 2016). On the contrary, improvements were observed in morbidity rates for sexually transmitted diseases and HIV.
The disease burden on African Americans as mentioned above depict the nutritional challenges experienced by racial group. Kolahdooz et al. (2016) highlight that African Americans have higher rates of overweight and obese individuals across the lifespan due to low socioeconomic status that limits access to healthy foods. Due to their low-income neighborhoods, they lack access to a variety of food stores and nutritious foods. As a result, this minority group ends up consuming high-energy foods of low nutritive value, and this tends to expose them to dietary disorders and associated diseases.
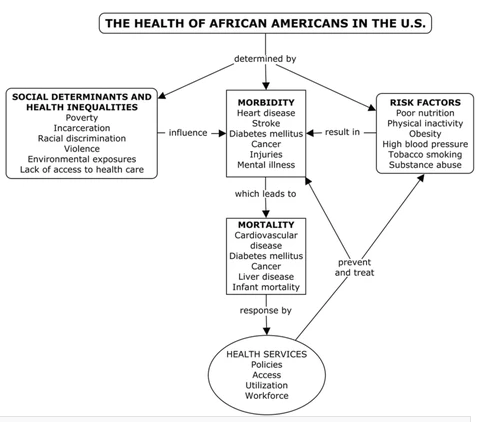
The discriminatory policies stemming from the slavery period and which bore racial discrimination continue to restrict accessibility to beneficial amenities among African Americans. Socioeconomic factors have a greater influence on the health of African Americans compared to other factors where income and educational level are significant factors, as indicated by the University of Iowa (2018). Noonan et al. (2016) show that fewer Blacks attain high school and university education compared to Whites. As a result, unemployment is equally low in this ethnic population as opposed to its Whites counterparts. Eventually, due to the lack of knowledge and resources, the health of African Americans is placed at a greater disadvantage. The figure below gives a clear picture of the health status of African Americans and factors resulting in the extant level of health.
The salient health disparities affecting this ethnic population have prompted faith-based organizations to get involved in attempts to improve the health status of African Americans. Sequentially, this is meant to bridge the gap in health for this population. These institutions organize health fairs, educational sessions, and screenings but encounter the challenge of resources in terms of educational materials and technology (Holt et al., 2017). These faith-based organizations (FBOs) are not aware of evidence-based interventions; hence, partnerships with healthcare organizations are imperative to enhance the efficacy of preventive initiatives by these FBOs.
Cultural factors have a bearing on the health of African Americans based on beliefs and values affecting what they do. 30% of African Americans believe that fate and destiny influence their health, and only a half of the population considers health to be essential (Noonan et al., 2016). As a result, spirituality plays an essential role in helping individuals to change their perceptions, which is linked to the regard of supernatural forces.
The fact that the younger population is suffering from diseases which are more common during older adulthood suggests that preventive services are more important compared to curative ones. The fact that African Americans have cultural beliefs and values that affect their health practices further justifies the essence of prevention compared to treatment. After all, curative services are more costly, and because African Americans have limited resources, the cheaper alternative of prevention is a better option.
Since African Americans believe in supernatural forces which influence their health, spiritual-based interventions are deemed to be more effective. Spruill et al. (2015) highlight the essence of spirituality in enabling this ethnic population to deal with their emotions, behaviors, perceptions, and coping strategies in attaining good health. Leininger’s theory on cultural care diversity and universality focuses on emic and etic factors, inferring to participants’ and professionals’ knowledge, respectively (Wagner, 2019). Thereby, in reference to the participants, spirituality is effective because it tends to be reinforced by the activities of FBOs. The etic knowledge is addressed through training to enhance their cultural competency while dealing with the ethnic group in question.
In conclusion, inequality in the accessibility and utilization of various societal structures is evident. African Americans have the worst health status due to both structural and cultural factors. In addition to the lack of resources, this ethnic population has distinct beliefs and values affecting their adoption of health practices. Thereby, preventive services are essential to this population as they need the right information to help change their perspectives and aid to minimize the effects of the lack of resources.
References
Centers for Disease Control and Prevention [CDC]. (2017). African American health. Web.
Holt, C. L., Graham-Phillips, A. L., Daniel Mullins, C., Slade, J. L., Savoy, A., & Carter, R. (2017). Health ministry and activities in African American faith-based organizations: A qualitative examination of facilitators, barriers, and use of technology. Journal of health care for the poor and underserved, 28(1), 378–388. Web.
Kolahdooz, F., Butler, J. L., Christiansen, K., Diette, G. B., Breysse, P. N., Hansel, N. N., McCormack, M. C., Sheehy, T., Gittelsohn, J., & Sharma, S. (2016). Food and nutrient intake in African American children and adolescents aged 5 to 16 years in Baltimore City. Journal of the American College of Nutrition, 35(3), 205–216.
Noonan, A.S., Velasco-Mondragon, H.E., & Wagner, F.A. (2016). Improving the health of African Americans in the USA: An overdue opportunity for social justice. Public Health Reviews, 37, 12.
Spruill, I. J., Magwood, G. S., Nemeth, L. S., & Williams, T. H. (2015). African Americans’ culturally specific approaches to the management of diabetes. Global Qualitative Nursing Research, 2, 1-9.
University of Iowa. (2018). Black Americans face education, income barriers to healthy behaviors, study finds.
Wagner, J. (2019). Leadership and influencing change in nursing [eBook edition]. University of Regina Press.