Introduction
The hospital discharge process is a critical administrative task that requires critical reform. Hospitals are faced with various logistical challenges that occur due to an inefficient discharge mechanism. This results in an increased length of stay, scheduling issues, and high rates of readmission, which accrue costs and limit patient satisfaction. The overcrowding of medical facilities has been primarily due to constricted patient flow as processes such as discharge become more complex and unorganized (El-Eid, Kaddoum, Tamim, & Hitti, 2015). There is an evident lack of standard or efficiency. The hospital discharge process can be improved by simplifying and delegating necessary duties to members of the medical team as well as focusing on the patient education factor to limit readmission.
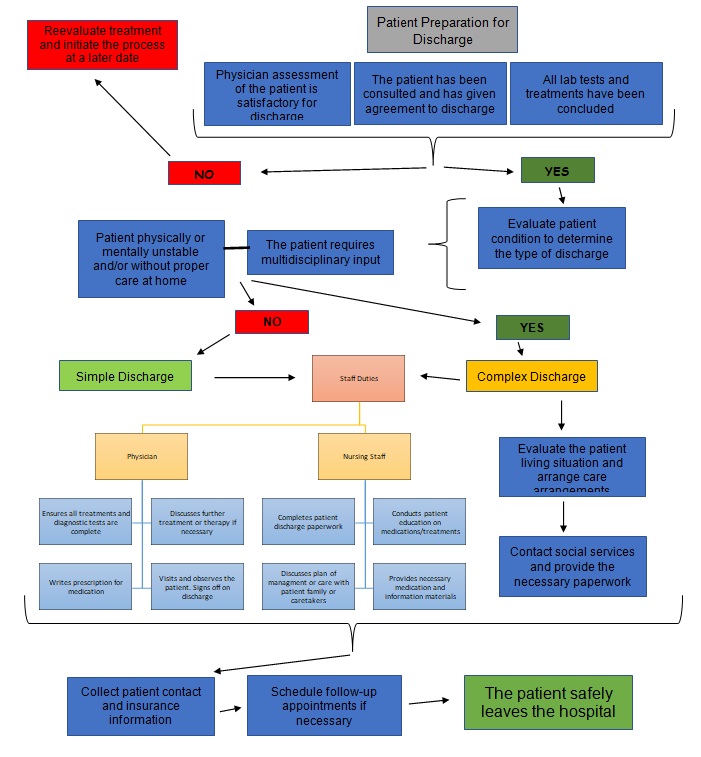
Workflow Chart
The first part of the flowchart focuses on preparation for discharge. It is a multistep process of examining the patient, communicating the intention to discharge, and ensuring the treatment is complete. The physician does it with the help of the nursing staff. Technology that is used in this step is primarily electronic health records for keeping track of the patient’s treatment. Usually, states have laws in place on patient discharge, indicating that a medical evaluation must occur to determine the conclusion of treatment and the patient consulted about the process. The information needed to complete this test is primarily the result of all completed treatments and analyses. This step was included due to the prevalence of patients discharged with pending diagnostic test results.
These are necessary for ensuring the individual’s appropriate treatment as well as a safe transition of care, which includes a comprehensive follow-up plan. At least 70% of patients are discharged with pending results, and only 18% of these were adequately noted in the discharge summary. It is estimated that a significant portion of physicians is unaware of the returning results, despite 9% requiring further intervention (Kanton, Evans, & Shieh, 2015). The health of the patients is endangered in such cases, and there is a high risk of readmission. Including these steps in the initial stages of hospital discharge protocol is necessary to ensure liability.
The next step is to evaluate the patient condition to determine physical and mental capability. At this point, the multidisciplinary approach is considered to determine the need for transfer to another facility for further treatment or residential care. Usually, the nursing staff aids with the paperwork, and a case manager investigates the patient’s plan of care after discharge. Electronic health records are once again instrumental in noting and tracking the necessary information. Legal frameworks on discharge exist in each state to guide this process ensuring it is safe to release the patient and there is an availability of proper aftercare. Information for completing this step is based on medical history and assessment. This information is used to determine whether there is a need for a simple or complex discharge. A simple discharge can be accomplished at the ward. Meanwhile, elaborate discharges that include transfers, social care, or additional accommodations are more intricate (Lees, 2013).
The last step consists of a comprehensive approach to finalizing the plan of care for the patient. That includes filling out prescriptions, patient education, and filling out paperwork. The physician, nursing staff, and administrative personnel are involved. In a simple discharge, the process is straightforward. However, in a complex discharge, a social worker may need to get involved to determine the next steps of care for the patient. It may be necessary to transfer the patient to another facility or contact social services to provide individual life-sustaining assistance at home. Electronic health records are used to record the information and send it to other facilities if necessary. Each hospital system maintains its policies on the procedures and rules to finalizing the discharge. Paperwork is completed with all contact or insurance information on the patient. Additional information may be required on a case-by-case basis. During this process, it is critical to emphasize the plan of care including education, follow-up appointments, and instructions for the patient that are easily understood (Horwitz et al., 2014). This improves the overall quality of the discharge practice that helps lower readmissions.
Evaluation and Improvements
Hospital discharge is evaluated by several parameters. There are statistical indicators that are based on the length of stay and the duration of the discharge process. Furthermore, there are qualitative evaluations that are conducted by patients expressing satisfaction. For example, patients can rate the effectiveness of patient education during discharge. These metrics are an effective tool for evaluation of the hospital discharge process as they highlight the areas of patient flow in a medical facility that are most critical. The flowchart was created to streamline the process, thus improving the speed and efficiency with which a patient is discharged. It emphasizes collaboration between staff and departments as well as patient education. Most often, the discharge process is complicated and delayed due to poor interdepartmental communication. Patients are forced to wait for hours until all the necessary procedures are completed (Ajami & Ketabi, 2007). The preparation process should begin up to 24 hours before planned discharge to competently follow the necessary procedures.
Patient education is a critical aspect that is often overlooked in the process of hospital discharge. It significantly impacts the outcomes of treatment, particularly in patients with chronic conditions. More than half of readmissions are preventable if the patient can adhere to medical recommendations and properly take prescription medicine. A competent approach to education at discharge helps reinforce the necessary recommendations and plan of care, which will help a patient to avoid readmission. Nurses who are in constant contact with patients have the most potential in implementing comprehensive education programs. Furthermore, both nurses and social workers can discuss plans of care with family members or other caretakers to ensure there is a proper support system in place for patients (Paul, 2008). Despite taking more time, patient education can be conducted efficiently with proper preparation before discharge.
Despite significant investment in health care technology, it is widely underutilized. Hospitals become dysfunctional with complicated processes such as discharge when there is a lack of communication and availability of information. The integration of specific software that functions in collaboration with electronic health records helps to manage patient flow. Instant availability of information in a unified software system improves communication amongst staff and departments. This becomes especially helpful in cases where a multidisciplinary approach was needed. Dedicated patient tracking technology is a tool that helps to approach health care strategically. It can be used in coordinating any activity related to the patient, including the readiness to discharge, tracking education sessions, and maintaining scheduled appointments (Maloney, Wolfe, Gesteland, Hales, & Nkoy, 2007). Overall, the use of technological decision support tools improves efficiency in patient flow while reducing the risk of human errors.
Summary
The discharge process should be efficient and standardized within a hospital environment to improve patient flow. It is critical to be aware of any process as it helps to improve the speed and effectiveness of the health services provided for the patient. A competent approach should be focused on providing the best care that influences patient health and satisfaction. A disorganized and dysfunctional discharge process leads to long wait times, a lack of bed space availability, and restricted patient flow. A simplified discharge flowchart creates a practical solution for the problem by emphasizing critical tasks and delegating them amongst the whole staff. Hospital administration should modernize and consolidate action plans for every complex process in the system.
References
Ajami, S., & Ketabi, S. (2007). An analysis of the average waiting time during the patient discharge process at Kashani Hospital in Esfahan, Iran: A case study. Health Information Management Journal, 36(2), 37-42.
El-Eid, G. R., Kaddoum, R., Tamim, H., & Hitti, E. A. (2015). Improving hospital discharge time: A successful implementation of Six Sigma methodology. Medicine, 94(12), e633. Web.
Horwitz, L., Moriarty, J., Chen, C., Fogerty, R., Brewster, U., Kanade, S., … Krumholz, H. (2014). Quality of discharge practices and patient understanding at an academic medical center. JAMA Internal Medicine, 173(18). Web.
Kantor, M. A., Evans, K. H., & Shieh, L. (2015). Pending studies at hospital discharge: A pre-post analysis of an electronic medical record tool to improve communication at hospital discharge. Journal of General Internal Medicine, 30(3), 312-318. Web.
Lees, L. (2013). The key principles of effective discharge planning. Nursing Times, 109(3), 18-19. Web.
Maloney, C. G., Wolfe, D., Gesteland, P. H., Hales, J. W., & Nkoy, F. L. (2007). A tool for improving patient discharge process and hospital communication practices: The patient tracker. AMIA Annual Symposium Proceedings, 493–497. Web.
Paul, S. (2008). Hospital discharge education for patients with heart failure: What really works and what is the evidence. Critical Care Nurse, 28(2), 66-82. Web.