Abstract
The prevalence of pressure ulcers in immobile patients still presents an important issue in the field of health care. The given study uses a mixed methods design to contribute to the field and conclude on the effectiveness of improved PU prevention protocols. According to the research results, the use of an improved PU prevention strategy in immobile patients helps reduce the prevalence of PUs threefold if compared to the traditional care strategy. The potential barriers to PU prevention in hospital settings were analyzed with the help of face-to-face interviews. The results indicate that, despite the benefits of PU prevention, nurses are concerned about increasing workload and the need to improve risk-assessment skills. In addition, patients’ unwillingness to collaborate and follow self-care recommendations is another theme related to PU prevention barriers. These results can provide the basis for recommendations helping to improve currently used strategies.
Introduction
Pressure ulcers (PUs) are a significant burden to healthcare as they are associated with high morbidity expenditures. According to Cano et al. (2015), “the cost of care for one PU is between $500 and $70,000, depending on the stage” (p. 574). At the same time, PUs are considered to be a preventable health problem. Therefore, by changing the procedures of patient risk assessment and undertaking measures to mitigate those risks promptly, hospitals can minimize unnecessary costs associated with the occurrence of PU and improve patient safety indices.
Purpose
The given topic is interesting because the development of PUs in hospitalized patients can be mainly regarded as a nurse-sensitive outcome. It means that a nurse should have the knowledge and the skills needed to recognize at-risk individuals and commence timely interventions in order to improve patient results. It is possible to say that, by impacting the area of nursing directly, the exploration of the effects of PU prevention protocols in emergency departments can help practitioners in acquiring these necessary competencies. Additionally and more specifically, the proposed research project will aim to explore the links between patient outcomes and nurse behaviors, as well as to inform the design of new potential solutions to the PU problem. These goals are measurable and realistic, yet their accomplishment will largely depend on the quality of research design in general.
The topic is relevant today because the prevalence and incidence of PU remain high although their rates may significantly vary across different types of settings. Additionally, Truong, Grigson, Patel, and Liu (2016) note that hospitals may implement different standards of PU prevention and treatment. It means that the efficacy of patient care may vary depending on the undertaken measures, as well as setting contexts. Thus, in-depth research of new care algorithms and materials may substantially benefit both patients and hospitals by providing opportunities for practice improvement.
Target Audience
Considering that the research project is meant to modify nurses’ behaviors, it will primarily target the given group of healthcare practitioners. Firstly, it will aim to provide the educational tool for all nurses regardless of their cultural, social, and demographic backgrounds in a specific, selected setting. However, it is expected that the findings will benefit every nursing practitioner and hospital working with at-risk individuals.
Research Questions
- Does the implementation of the prevention protocol reduce the incidence of PU in hospitalized patients?
- What are the patient and the hospital costs of utilizing the new protocol compared to usual care procedures?
- How effective is the new protocol in treating PUs registered on patient admission in terms of wound recovery?
- What are the major difficulties and barriers to the implementation of the PU prevention protocol in the hospital environment?
Problem Statement
Considering that emergency departments are associated with a high risk of PU development in hospitalized patients, the lack of standard and effective preventive care protocols may compromise patient safety and lead to excess treatment costs.
Hypothesis
Compared to usual care initiated within the emergency department, the implementation of the PU protocol, covering a broad range of nursing behaviors in relation to the identified adverse health condition, can potentially help reduce the occurrence of hospital-acquired PUs during a prolonged hospitalization. The hypothesis suggests that the frequency and correlation of the implementation of preventive care measures (independent variables) are directly related to patient outcomes (dependent variable). The relationship between them will be tested through the comparison of pre- and post-utilization data, whereas the factor of nurse adherence and PU incidence rate will be measured at both stages of research.
Review of Literature
Silicone foam dressing is one of the primary methods of preventing pressure ulcers in patients. However, it is not widely implemented as a standard protocol, which relies primarily on repositioning and use of soft padding under the points of contact. Truong et al. (2016) analyzed the available literature on the effectiveness of silicone foam dressings versus standard protocols. According to their findings, silicone foam shows greater effectiveness in preventing ulcers – it is 42.9% vs. 3.6% for standard protocol (Truong et al., 2016, p. e730). In addition, the average net cost of the intervention was $52.87 dollars, whereas about $107.9 was needed for the implementation of usual care protocols (Truong et al., 2016, p. e730). This source directly answers some of the research questions pertaining to the thesis of this paper. However, its major limitation lies in the duration of the experiment and its small sample size, which makes it difficult to extrapolate the results.
Cano et al. (2015) experimented with changes to the standard protocol and the materials used for preventing the development of pressure ulcers in patients. Namely, all standard supportive surfaces were replaced with Hill-Rom Advanced Microclimate Technology Mattresses. Advanced protocols of supervision and care were strictly followed. As a result, the incidence of PU dropped from 11.7% to 2-4% (Cano et al., 2015, p. 574). This source directly answers the first, second and third research questions, providing data for financial feasibility and the overall effectiveness of the intervention. One of the potential gaps in this research, however, lies in the lack of comparison between newly introduced and standard protocols. It is possible that high results were achieved because of higher percentages of compliance associated with motivation from participation in an experiment.
The article by Worsley, Clarkson, Bader, and Schoonhoven (2016) investigated some of the barriers and facilitators to participation in pressure ulcer prevention. According to their findings, the greatest barriers to practicing PU prevention were limitations in resource (not enough staff/lack of equipment), lack of professional education, and professional boundaries. This source answers the fourth research question by addressing factors directly and indirectly associated with the implementation of PU prevention protocols. One of the greatest limitations of this study is that it does not provide any guidelines for overcoming the problem.
There are various obstacles to the implementation of special protocols reducing the incidence of HAPUs in emergency departments and other types of hospital settings. Discussing the barriers to PU prevention, Balzer and Kottner (2015) focus on the necessity to institutionalize changes, agree on the most effective patient care practices to be used, and successfully incorporate the revised care protocols into practice. Apart from that, many authors highlight the negative impact of challenges related to outcome evaluation. Thus, many researchers agree that the question of determining relevant patient-important outcomes is still open even though there is a range of valid tools helping to study health changes (PU staging procedures, visual assessments, etc.) (Balzer & Kottner, 2015; Padula et al., 2015).
The use of prophylactic dressings helping to reduce pressure on certain parts of the body is widely discussed by modern researchers and is often listed among the most promising components of HAPU prevention strategies. As the authors of certain systematic reviews conclude, special medical dressings (especially multi-layer) have a significant impact on HAPU incidence rates and can reduce chronic wound prevention costs that exceed $15 billion in the United States (Black et al., 2015, p. 484). As for the results of long-term experiments, the implementation of comprehensive HAPU prevention programs including adhesive dressings leads to a 69% reduction in incidence rates in ICUs (Swafford, Culpepper, & Dunn, 2016).
According to the study with the sample size exceeding 400 adult ICU patients, prophylactic wound dressings help reduce the incidence of HAPUs by more than 10% (Black et al., 2015, p. 485). The ability of wound dressings made of different materials to reduce the incidence of HAPUs in high-risk patients is also discussed in the review by Clark et al. (2014). As is clear from their findings, the use of wound dressings in EDs positively impacts patient outcomes, whereas hydrocellular foam dressings cause the 11 times reduction of HAPU incidence rates if compared to gauze dressings (Clark et al., 2014, p. 467).
Apart from the use of special medical equipment and repositioning techniques, current PU prevention strategies can be improved with the help of patient education and the promotion of self-help. In their systematic review, Baron et al. (2016) suppose that behavioral and educational interventions help patients better recognize worrying symptoms. Despite that, the extent to which education on self-help and PU prevention in patients with movement issues impacts the actual incidence rates presents a significant research gap that needs to be addressed in the nearest future.
Other components of effective PU prevention strategies discussed in the reviewed articles include the use of CBPM devices and electric stimulation. In their study, Behrendt, Ghaznavi, Mahan, Craft, and Siddiqui (2014) prove that modern CBPM systems can decrease the incidence of HAPUs by generating pressure images and providing recommendations that allow “off-loading high-pressure areas” (p. 127). Having studied the sample of more than 400 patients, the authors found out that the use of CBPM was associated with a five times decrease in HAPU incidence rates (Behrendt et al., 2014, p. 131). Specific preventive interventions included in HAPU prevention strategies may vary depending on patients’ medical conditions. For instance, electric stimulation is among promising methods to be used in people with spinal injuries despite numerous issues related to the choice of stimulation frequency, currents, and length (Liu, Moody, Traynor, Dyson, & Gall, 2014).
Research Methods Used and Data Collected
Research Design and Search Strategy
Within the frame of the research, a thorough literature review was conducted in order to analyze the hypothesis and make conclusions concerning the effects of special PU prevention protocols on the costs of treatment and health outcomes of high-risk patients. A mixed-methods research design was chosen to conduct the study and take into account both quantitative and qualitative findings reported by the previous researchers in the field. An opportunity to analyze the combination of numerical and categorical data can be listed among the key advantages of literature reviews. Given that it is helpful in identifying trends in various research fields, the use of the specified research design was regarded as the best option.
The following steps were taken to construct and implement a proper search strategy:
- Choose at least 2 professional medical databases;
- Determine the right keywords related to the hypothesis;
- Conduct keyword search;
- Sort search results to exclude repetitions;
- Eliminate irrelevant and low-quality articles.
Professional databases utilized for the research included CINAHL and MedLine (accessed via PubMed). Given that the hypothesis referred to the financial and health effects of specialized PU prevention protocols, both topics needed to be reflected in search queries. Therefore, the following keywords were used: barriers to PU prevention, HAPU, PU, pressure ulcer prevention program, hospital-acquired pressure ulcers, standard pressure ulcer protocol, PU prevention costs. During the first stage of data collection, 112 articles from professional nursing and medical journals were retrieved in total (with repetitions excluded). Then, the search results were sorted based on the up-to-dateness (articles no older than five years were preferred) and quality of studies. In reference to the latter, it was determined with special attention to the hierarchy of evidence (systematic reviews and RCTs were included first), researchers’ objectivity (the discussion of study limitations, etc.), and the impact factors of journals. Finally, 11 journal articles relevant to the topic and meeting the requirements above were included in the literature review, and their findings were summarized to answer the research questions. The chosen studies are dated 2014 (3 articles), 2015 (4 articles), and 2016 (4 articles).
Results and Analysis of Research Findings
The Effects of Comprehensive PU Prevention Protocols
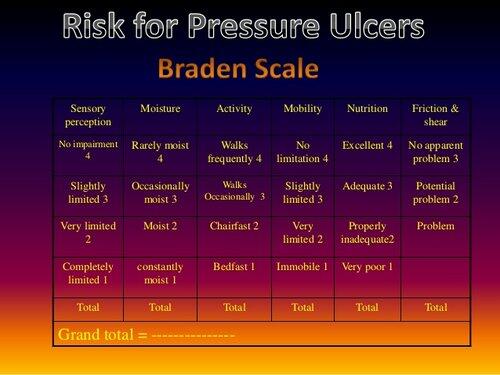
The first part of the study presented an experiment, in which nurses were provided with improved PU prevention guidelines. Prior to the intervention, the researchers used the Braden Scale to determine the risks of PU in participants. According to the results, all participants had high or very high risks (the score range from 6 to 12). Given the health characteristics of the population, the highest risks were associated with the mobility subscale (see figure below).
The intervention and control groups that took part in the experiment were heterogeneous in terms of ethnicity, age, and medical condition. The mean age in the intervention group was 59 years and 5 months. On average, the members of the control group were older (the mean age was 62 years and 3 months). In reference to the racial composition of the groups, the data was the following for the intervention group: White – 45%, Asian – 10%, African American – 25%, Hispanic – 20%. In the control group, the larger part of the participants was White (35%), whereas the percent of people identifying themselves as African Americans, Hispanics, and Asians was 30, 15, and 20 respectively. When it comes to gender composition, women presented 55% of the intervention group and 40% of the control group. The causes of the participants’ immobility were extremely different and included severe arthritis, hip traumas, stroke, fractures, and neurodegenerative disorders.
To measure the effectiveness of the above approach to decreasing the incidence of hospital-acquired pressure sores, a standardized PU classification scale was used. Before and after the intervention, the pressure ulcer status of the participants was measured using the NPUAP guidelines concerning PU classification. The following results were retrieved with the help of the Braden Scale: 70% of participants in the intervention group and 65% in the control group had high risks of PUs, whereas the risks for the remaining participants were very high.
The measurements taken prior to the start of the program indicated that, despite high risks, there were no cases of bed sores in both groups since the patients had been hospitalized recently and received appropriate care from their relatives. Two weeks after the implementation of improved PU prevention guidelines, the presence of stage 1 pressure ulcers was discovered in 10% of the intervention group, whereas the cases of stage 2, 3, 4, and unstageable PUs were absent. The control group received usual care; in particular, there were no strict requirements concerning the frequency of skin assessments and patient repositioning. As it has been mentioned, the risks of PUs were extremely high for 35% of participants receiving usual care. The following data on the PU status of patients from the control group were collected after the experiment: stage 1 PUs developed in 20% of the participants, whereas 10% had stage 2 pressure sores. The analysis of the practical results of the tested intervention indicates that the cases of stage 1 and 2 PUs were three times more often in the group receiving usual care if compared to the intervention group. The results demonstrate that the combination of measures with proven effectiveness positively impacts patient outcomes regarding pressure ulcers, which is consistent with previously reported findings (Behrendt et al., 2014; Baron et al., 2016). However, defining the specific role of each measure included in the protocol may require the use of a larger sample.
Perceived Barriers to PU Prevention
Ten nurses agreed to participate in qualitative interviews and share their opinion on the problems related to the prevention of pressure sores in immobile people. The participants were nursing professionals aged 27-39 with a minimum of 3 years of professional practice. The following questions were included in the interview:
- Demographic data, professional experience;
- Do you find the prevention of pressure sores time-consuming and why?
- What do your colleagues think about standard PU prevention practices, do they find them overrated?
- Can the majority of bedsores be prevented and why?
- What aspects of PU prevention should be emphasized in staff education to improve patient outcomes?
A thematic analysis was conducted to analyze the interviews and single out the most common ideas related to factors that make PU prevention strategies less successful. From reliability considerations, all interviews were coded by the two researchers, and three themes were found to be the most frequent in the nurses’ answers. Among them, there were a heavy workload that increases with the implementation of new PU prevention practices (in 60% of the interviews), the need to improve nurses’ risk assessment skills (in 50% of the interviews), and patients’ unwillingness to cooperate (30%). In general, the findings support the opinion that the professional skills of nursing staff and their attitudes toward nurse-patient communication can have an impact on the prevalence of PUs (Balzer & Kottner, 2015). Importantly, there were no interviewees who regarded the currently used PU prevention practices as extremely effective.
Discussion of Hypothesis/Conclusion
The study hypothesizes that the use of improved risk assessment and PU prevention practices positively impacts patient outcomes and reduces the costs of PU treatment. Importantly, the issue impacts both health outcomes of vulnerable patients and the costs of treatment because managing the consequences of hospital-acquired pressure sores involves significant financial expenditures (Swafford et al., 2016). The given research focused on studying the effectiveness of a comprehensive pressure ulcer prevention protocol if compared to standard care that patients at one of the local hospitals received. Another area of focus that has been identified earlier is the range of barriers to pressure ulcer prevention in hospital settings.
The results of the study demonstrate that healthcare managers can positively impact patient outcomes in relation to HAPUs by increasing the frequency of skin assessment and repositioning procedures, using high-quality equipment, and providing necessary patient education. Also, from the qualitative analysis, it is clear that the barriers related to workload, staff education, and patients’ attitude to self-care can pose a threat to the success of PU prevention programs. However, given that sample size directly impacts validity, conducting similar studies with larger samples is recommended.
References
Balzer, K., & Kottner, J. (2015). Evidence-based practices in pressure ulcer prevention: Lost in implementation? International Journal of Nursing Studies, 52(11), 1655-1658.
Baron, J., Swaine, J., Presseau, J., Aspinall, A., Jaglal, S., White, B.,… Grimshaw, J. (2016). Self-management interventions to improve skin care for pressure ulcer prevention in people with spinal cord injuries: A systematic review protocol. Systematic Reviews, 5(1), 150-157.
Behrendt, R., Ghaznavi, A. M., Mahan, M., Craft, S., & Siddiqui, A. (2014). Continuous bedside pressure mapping and rates of hospital-associated pressure ulcers in a medical intensive care unit. American Journal of Critical Care, 23(2), 127-133.
Black, J., Clark, M., Dealey, C., Brindle, C. T., Alves, P., Santamaria, N., & Call, E. (2015). Dressings as an adjunct to pressure ulcer prevention: Consensus panel recommendations. International Wound Journal, 12(4), 484-488.
Cano, A., Anglade, D., Stamp, H., Joaquin, F., Lopez, J. A., Lupe, L., … Young, D. L. (2015). Improving outcomes by implementing a pressure ulcer prevention program (PUPP): Going beyond the basics. Healthcare, 3(3), 574–585.
Clark, M., Black, J., Alves, P., Brindle, C. T., Call, E., Dealey, C., & Santamaria, N. (2014). Systematic review of the use of prophylactic dressings in the prevention of pressure ulcers. International Wound Journal, 11(5), 460-471.
Liu, L. Q., Moody, J., Traynor, M., Dyson, S., & Gall, A. (2014). A systematic review of electrical stimulation for pressure ulcer prevention and treatment in people with spinal cord injuries. The Journal of Spinal Cord Medicine, 37(6), 703-718.
Padula, W. V., Makic, M. B. F., Mishra, M. K., Campbell, J. D., Nair, K. V., Wald, H. L., & Valuck, R. J. (2015). Comparative effectiveness of quality improvement interventions for pressure ulcer prevention in academic medical centers in the United States. The Joint Commission Journal on Quality and Patient Safety, 41(6), 246-256.
ProHealth Wound Care. (n.d.). Risk for pressure ulcers [Image]. Web.
Swafford, K., Culpepper, R., & Dunn, C. (2016). Use of a comprehensive program to reduce the incidence of hospital-acquired pressure ulcers in an intensive care unit. American Journal of Critical Care, 25(2), 152-155.
Truong, B., Grigson, E., Patel, M., & Liu, X. (2016). Pressure ulcer prevention in the hospital setting using silicone foam dressings. Cureus, 8(8), e730. Web.
Worsley, P. R., Clarkson, P., Bader, D. L., & Schoonhoven, L. (2016). Identifying barriers and facilitators to participation in pressure ulcer prevention in allied healthcare professionals: A mixed methods evaluation. Physiotherapy, 103(3), 304-310.