Executive Summary
Many factors have influenced the disbandment of hospital-based infusion therapies over the past sixty-five years. The laws of the state initially required hospital caregivers to provide all four infusion therapies. However, the rules changed at the beginning of the 1960s (Bolton, 2009). Due to these legal changes, there was a need for highly skilled and specialized nurses to take up infusion responsibilities. It led to the development of infusion teams in various hospitals in the USA. At the turn of the 21st century, however, expenses and cost regulations regarding infusion services triggered multiple drawbacks. Business counseling organizations suggested disbanding infusion groups in numerous health facilities as an expense-cutting measure (Carr, Glynn, Dineen & Kropmans, 2010). This measure staked on shifting all the imbuement obligations from the overburdened medical attendants (Hadaway, 2012).
The United States is in the early phases of rebuilding its financial structure (Carr et al., 2010). The structure, in combination with the quality-based installments and pay-for-execution programs, intends to fund the social insurance framework within the USA. As such, the reestablished accentuation on enhancing patient results and security, for example, diminishes the vascular access gadgets as well as the imbuement-related intricacies. It also slackens the usage of perceived gauges and rules as the clinical results, after an imbuement group, are obscure (Wagner, 2009). Furthermore, there is next to no information discussing healing centers, nursing units, and mixture groups. Numerous infusion caregivers see an increment in combination-related inconveniences, bargains in patient security, and a comparing diminishing inpatient fulfillment, yet do not have the workforce and assets to approve these recognitions. Episodic confirmation or view of these issues misses the mark regarding the information expected to invite chiefs to bolster the monetary developments of another infusion team.
This dire information will help in the decision-making exercise between proceeding with the backing arrangements for the current group or growing the administrations of a conventional group. Currently, the choices in clinic management encompass a discriminating concentrate on business perspectives, namely, how the proposed activity will influence expenses and income. The business proposal is a typical instrument used to answer the troublesome inquiries regarding the designation of constrained assets and the infusion nurses (Bolton, 2009).
Introduction/ Concept Description
The term ‘business proposal’ functions to highlight two unique approaches: one, a proposition spotlight, and two made and two, as a money-related result (Wagner, 2009). A business proposal comprises an organized plan utilized by hierarchical chiefs to legitimize the interest in an undertaking, another service, or improvement (Carr et al., 2010). This schedule contains complete data accompanied with substantial clinical information for the examination and cautious budgetary investigation, aiming to secure the forecasted targets.
The plan also embodies the ambition and desire to bolster the organization’s administration. As Kelly (2009) explains, the clinic’s executives have ratified the proposal, as it has revealed the acquisition of a budgetary profit and accumulative interests, all in a sensible period. The formulated proposition is, therefore, crucially indispensable, as it facilitates the accomplishment of the money-related profits at the end of the day. The scheme incorporates an examination, which involves the healing facility acting in an unraveling way to diminish its difficulties (Carr et al., 2010).
According to Bolton, it is imperative to gather and dissect clinical results information from relevant directories and persons (2009). While information from distributed studies is useful, information from the particular healing facility gives a more definite picture of what is happening. Individual patterns for resolving issues may incorporate unsuitable rates of the focal line related Circulatory System Disease (CLABSI), paying little heed to numerous intercessions officially executed.
Other equally important issues concerning the implantations include penetration, extravasations, phlebitis, vein thrombosis, iatrogenic pneumothorax amid focal venous catheter insertion, and venous air emboli connected with any vascular access gadget. Information from mixture-related episode reports and Sentinel occasion reports ought to submit to an evaluation. Cases of carelessness or misbehavior combined with Imbuement treatment must subside (Gopal, Fitzsimmons & Lawrence, 2006). The proposition ought to break down the neighborhood and national needs relating to the undertaking. Cases of national needs identified with Imbuement-related results incorporate the doctor’s facility gained conditions from the Centers for Medicare & Medicaid Services (Hawes, 2007).
The healing facility cannot bill Medicare when these conditions occur, and this rundown now incorporates four mixture-related conditions. They encompass air emboli, blood contradictory, vascular catheter-related diseases, and pneumothorax from focal venous catheter insertions. Numerous other national activities, for example, pharmaceutical blunders, caution weaknesses, transfusion practices, and needle stick and different sharps wounds, ought to go through the analysis.
The proposition must give an unmistakable comprehension of what is being set forward, for example, an implantation group that meets the INS definition. The extent of administration for this group, the staffing blend, buying of new capital gear (ultrasound machines), hours of operation, and patient needs are necessary. The board should examine the distinct options for the proposed infusion team such as beginning a small catheter insertion group, or a group with restricted hours of operation. Nevertheless, the issues and adverse clinical results adequately included in the proposition give data regarding why these choices are poor decisions.
Monetary information for every option ought to undergo comprehensive investigations so a reasonable correlation can surface, remarks Hadaway (2012). As Finkler, Jones and Kovner summarize, these progressing expenses may surpass the expenditures of an imbuement group (2012). Finally, the proposed activity must fit the healing facility’s expressed mission, vision, and key arrangements. The most vital provisions for doctor’s services incorporate settings include the nature of patient care and astute budgetary administration. Other equally important goals encompass those that are entirely reliable with the safe conveyance of implantation treatment (Silva, Priebe & Dias, 2010). The business proposal will hail from the association’s point of view that will be paying for the proposed development of a healing center and a mixed group.
Problem Statement
According to Carr et al., the activities in the hospital have increased, thanks to the growth in the number of patients admitted to the hospital during weekends (2010). It, therefore, follows that the available staff is not adequate for this growth in volume, quotes Hawes (2007). Secondly, the patients diagnosed with critical conditions do not even surface in the weekend census of the hospital (Finkler, Jones & Kovner, 2012). It is for these reasons that the facility has deemed it fit to increase the number of staff by employing weekend infusion nurses to take care of the vast number of patients over the weekend.
Proposed Solution
In light of the problem statement above, the executives have contemplated hiring an additional infusion nurse for weekend coverage. The supplemental infusion nurse will enable the facility to provide quality and time-conscious care to patients who come to the hospital during weekends (Brunelle, 2003). Over and above this, there are plans to assimilate a comprehensive employee health-promotion program that will focus on the most crucial needs of the organization. This employee program will help abate the rise in costs in conjunction with restoring the productivity and health of the staff (Kelly, 2009). Further, the management proposes to enforce an annual health assessment and survey of employees that will serve to certify that the services provided, target the most crucial health needs of the population. As prescribed by law, the board will draw the annual goals and direction of the program (Gopal, Fitzsimmons & Lawrence, 2006).
Goals and Objectives
This segment records how the proposed infusion group will improve the clinic’s capacity to meet built-up objectives as well as goals. Outlined beneath are a couple of conceivable goals, pinpointing how the implantation group recruitment will bolster these envisions (Wagner, 2009).
- The clinic looks forward to dispensing timely and cost-effective care for patients over the weekend.
- To establish a separate cost center that will track the revenue and expenses associated with patients during weeks.
- To reduce the overall cost of supply and infusion therapy procedures by ameliorating the venipuncture proficiency rates (Bolton, 2009). Augmenting the usage of sets of administration and other additional services will also help condense the production costs as well as enhance the standardization and development of staff.
Justification
Option 1
Take no action and continue staffing as we do. Since the problem will not diffuse soon, overtime expenses will continue to rise (Finkler, Jones & Kovner, 2012). This crisis will eventually impede staff satisfaction; thus, placing the hospital at very significant risk of losing its key personnel members (Gopal, Fitzsimmons & Lawrence, 2006). Therefore, until the board develops a mechanism to account for the increased activity, the facility will continue to incur overtime overheads and continue using traveling nurses.
Option 2
Hire an additional infusion nurse for the weekend coverage, cautions Hawes (2007). The nurse’s responsibilities will include overseeing all processes in the hospital during the weekend. Integrate a new cost complex to tackle the revenues associated with short-stay patients as well as the bills related to the nurses’ food, linen, salaries, supplies, equipment, and other items. The present nurse manager of the entity will chaperone this imminent cost facility.
Option 3
Set apart an exclusionary space in the hospice for the personnel and short-stay care provisions. This alternative looks to deflect from the possibility of having to absorb these short-stay residents onto the inpatient unit. This decision, however, calls for an entirely different business plan entailing a cost/benefits evaluation (Finkler, Jones & Kovner, 2012). The evaluation will necessitate completion by other commercial counterparts other than the nurse manager, as it would engage other stakeholders such as engineering, finance, and other departments.
Impact on the Organization
This segment depicts how the proposed imbuement group will change or influence the association (Wagner, 2009). It further clarifies various legislative parts, outlining how these sections may change as an aftereffect of this new imbuement group. The board must choose the part of the mixture group chief and staff alongside an intensive exchange of how the new imbuement group will communicate with other office operations. As outlined by Carr et al., these activities include the radiology, outpatient administrations, and crises divisions (2010).
There are clear articulations about the extent of implantation treatment officials relegated to the mixture group versus those exercises that will be the obligation of the medical staff attendants. Numerous parts of hierarchical changes could happen from the advancement and recruitment of an implantation group, asserts Kelly (2009). The need for staff advancement and tutoring of all patient considerations is instrumental to enhancing those perspectives of mixture consideration relegated to the nursing staff. Master implantation attendants will regulate item assessment and quality change undertakings. They will also distinguish other danger administration procedures, and serve on related authoritative advisory groups (Gopal, Fitzsimmons & Lawrence, 2006). The area gives an abnormal state clarification of how the association will reform as an aftereffect of the imbuement group
Cost-Benefit Analysis: Benchmarking & Productivity
Most people consider this as the standout element amongst the distinctive parts of a business proposal, as it stipulates the expenses or investment funds projection that influences the last support to get up and go. It is critical to measure the money-related advantages of the improvement of an infusion group just one desire in circumstances like that one in the business case. Finkler, Jones and Kovner proffer various methodologies that pertain to the cost-benefit analysis (2012). Of vital importance are the concepts of benchmarking and productivity. A cost-benefit analysis can operate under the benchmarking parameters to entrench preeminent practices and skills for the clinic as contrasted with other organizations. The CBA procedure entails money-saving investigations (Wagner, 2009). The reason for this is to outline the expenses connected with the proposed change and contrast them and the benefits and investment funds to show the quality of the Association.
Another equally important concept is the productivity notion that strives to ensure that all the organizational units and departments are all right, thus safeguarding the performance of the firm. This section ought to incorporate the pay, advantages, and finance costs for the imbuement colleagues. Imbuement attendant specialists drive foreseen reserve funds from the more productive time administration, diminishment in hold up time (in this way enhancing patient throughput), and lessening so as to perform an assortment of strategies. Catheter utilization can also exhibit a decrease in expenses as an aftereffect of expanded competency (Gopal, Fitzsimmons &Lawrence, 2006).
This new position will not need a replacement component because it is a weekend job. An infusion nurse (IN) x 2,080(number of paid hours per year) x $30 (average hourly pay rate for the infusion nurse= $ 62,400 per year. Benefits are currently running at 30% (according to human resources), for a total salary of $89,856. Overtime expenses were $5,400 last month. After implementing the new Infusion Nurse (IN) position, we expect this amount to decrease by 75%, creating savings of $48,600 anticipated by the third month of the project. As noted earlier, short-stay patient revenues will not finance the unit cost center. Instead, it is advisable to implement a separate cost center that will function as a tool for auditing the clinic’s income and expenses. The overall effect of this change would be an increase in FTEs by 1.0.
Market Analysis
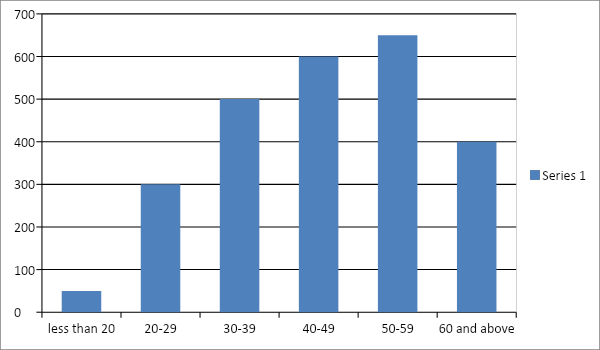
For slightly more than six months, a twenty-five percent increase has surfaced due to the high number of patrons visiting the health facility for outpatient as well as inpatient services. The hospital receives an average of five short-stay patient transfers or admissions per day- a financial aspect not included in the budget process (Finkler, Jones & Kovner, 2012). The hospice dismisses the short-stay residents before midnight and, therefore, does not count them in the midnight census. We have unraveled an exceptional practice, nonetheless, after appraising other similar medical corporations and perusing journal articles. Our findings divulge that many hospitals and care complexes segregate specified enclosures in the hospital, expressly designed for caring and tending to these patients. This trend is a daily routine especially for those high volume hospitals caring for numerous residents (Kelly, 2009). Other establishments, on the other hand, apportion cost centers to audit the facility’s revenue and expenses, overseen by the conventional nurse administrator. As Hadaway (2012) explains, third fractions of our patients are veterans and, therefore, get extra healthcare services through our hospital (see Table 1).
The 4 P of Marketing
Product
Before implementing the plan, we will determine the products that we wish to incorporate as well as ask ourselves important questions that will enable us to understand our products. We will need to know how useful this program will be as regards the need to solve our problems as a medical corporation (Silva, Priebe & Dias, 2010). We shall also take into account the pros and cons of these products in combination with their distinctive features and traits, says Bolton (2009).
Price
Price is the second agent in the list of the four Ps. For the health facility to work efficiently and gain profits at the end of the day, the management crew has to mull over the price/ cost of every service provided. We will consider all variables that make up the cost of a service or product. These variables include the location of the facility, distribution, and the cost of the same service in other installations, as well as the methods and plans of payment (Hawes, 2007).
Promotion
The promotion is the third entity on the list. Whether done through event marketing, website, social media or any other form of advertisement, we will have to ensure that the marketing strategy that we employ is appropriate. This certification is about the product on offer, the customer, and the price. A promotion that lacks authority can be a real waste of time and money (Carr et al., 2010).
Placement
The final P on the list is placement. It clearly states where a product or service will fetch the highest prices and values. We will also create an exit strategy in case things do not go as planned. In such cases, we will try to find other sales channels (Finkler, Jones & Kovner, 2012).
Explanation of the Program and Its Implementation
We will particularize the details in the job description analysis for the Infusion Nurse role and draw the salary structure, siphoning help and advice from the human resource personnel. As the norm, the human resource will publicize the new contract internally through memos before proceeding to advertise it in the local dailies and magazines. As regards the internal advertisement, we will only welcome applications and resumes for a maximum of three days, starting on the publication day (Finkler, Jones & Kovner, 2012). In case we do not obtain any resumes or qualified applications from our internal workforce, we will go on and display the position in the local editorials and gazettes.
Once we detect a couple of qualified applicants, the nurse manager, and the nurse in charge of each scheduled period will interrogate the prospects (Kelly, 2009). The first two aspirants will carry on sitting for subsequent interviews with the clinical nurse specialist, two chief physicians, as well as the nurse manager of the unit. After these exercises, we will then single out and make a pitch to the most competent personage, and upon accession, we will affix the start date in compliance with the group schedule. If the character recruited is an internal staff member, we will ensure that we substitute his or her slot immediately. We shall enlist the help of the nurse manager and human resources in the substitution of this position (Hadaway, 2012).
We will conduct an imperious staff meeting to elucidate on the new position and its accredited roles and responsibilities advise Brunelle (2003). Furthermore, we will also bring up-to-date staffing itineraries to signify the new occupation. In collaboration with the finance division, we will institute a cost center integer and a signature title for the area (for example, Short-Stay Division or 5 West Short-Stay). By teaming up with the admissions bureau, we will install a comprehensive communication technique that will work to certify that an adequate coding system is in place. We will also devise a brief commentary to all staff members and stakeholders, explaining how to encrypt the time on their time billets, if they are watching over the short-stay patients.
Evaluation of Program
The program will undergo an intensive assessment procedure for a maximum of 60 days and again at six months, following the start of the program. We shall enlist the knowledge of various reports to help in executing an accurate analysis of this new venture (Finkler, Jones & Kovner, 2012). The overtime records, productivity, monthly financial statements, and surveys pertaining to patients, charge nurses, staff satisfaction, and physicians are among the accounts we shall utilize. They will also obtain varied materials through employee orientation to be sure that each employee is aware of the services available to them. Every employee will acquire the services of health and program offers, through an online email receipt or fliers. They shall also obtain a site events calendar, containing all the respective particulars and event details (Gopal, Fitzsimmons & Lawrence, 2006).
Management Plan
In this section, we discuss the roles practiced by every team member involved in the development of the infusion group (Finkler, Jones & Kovner, 2012). One person should be enough to oversee the creation of the proposal. This individual should be the proponent of the venture, who is capable of preparing an analysis of what is necessary and how to achieve it (Bolton, 2009).
Table 2: Management Plan
Table 3: Marketing/ Communication Plan
Table 4: Key Resources for Performance
Assumptions
The management crew postulates that the budget of the health facility is sufficient to support an infusion team. Another notable assumption encompasses the stipulation that sufficient nursing expertise is available in infusion therapy to staff the infusion group (Brunelle, 2003). The last assumption is that there is the availability of baseline data for evaluating an infusion group.
Limitations
- Lack of funds for supporting the infusion team in terms of benefits, salaries, overhead cost and supplies
- Lack of the necessary qualification and expertise for nurses to be in the infusion team
- There is an inadequate baseline data of major performance indicators, working as the foundation for the effect of the infusion group.
- Nurses and other medical staff resist the formation of an infusion team.
Alternative analysis
Alternatives
Analyze current labor and inventory cost. It should be the highest cost option.
Reasons for selecting it
Keep the status quo alive with all members of the health facility. Insert all VADS and perform all infusion therapy.
Fiscal Blueprint/ Plan
The clinic will appoint one infusion nurse, whose salary settlement per year will equal to 2,080 x $30 = $62,400, analyzes Hadaway (2012). This new task does not necessitate any substitutions whatsoever as it is on a contractual basis, executed during the weekends only. Regardless, the position entails various costs peculiar to benefits; the gains will amount to 30%. The aggregate salary bill equals $81,120. Presently, the overtime charges for the previous month were $5,400. According to Silva, Priebe and Dias (2010), these expenditures emanate from the increased number of hospice workers needed to deliver nurse the short-stay clients. By putting into action the new RN occupation, we postulate that this amount ($5,400) will devaluate by 75%, thus, salvaging a minimum of $48,600. Nonetheless, some cumulative over time will surface as time advances, assures Wagner (2009).
The revenue collected from the short-stay residents is funding the outpatient services at the institution and, therefore, is quite strenuous to quantify (Finkler, Jones & Kovner, 2012). We have found out that we are raking in roughly $500 per patient in indemnification. We unraveled this piece of information after teaming up with the accounts receivable constituent and scrutinizing the patients’ records and medical history over the recent 90 days. The hospital receives a minimum of 200 patients during weekends. So 200×2 days per week x 90 weeks (number of weekends per year) = 36000 patients per year. Anticipated revenue of $500 per patient x 36000 patients = $18,000,000. This venture entails a high-end budget. If the proposal is feasible, we will create a complete budget that will incorporate indirect costs (Gopal, Fitzsimmons & Lawrence, 2006).
Table 5: Rough Financial Plan
Conclusion
In this era, patients engage more in out-of-the-pocket expenses for health care. As a result, patients demand quality as well as increased services. As the consumers of health care become more knowledgeable, they continue to appreciate patient-centered health care. However, the hospital administrative bodies can work to incorporate lower costs from the well-coordinated care treatments. As much as these regimens are of low costs, they should be safe and proficient. Infusion teams, therefore, can be the source of these lower costs of health care.
References
Bolton, D. (2009). Writing a business case for the expansion of service: Expanding the IV therapy team, from start to finish. Journal of Infections Preview, 10(1), 27-32.
Brunelle, D. (2003). The impact of a dedicated infusion therapy team on the reduction of catheter-related nosocomial infections. Journal of Infusion Nursing, 26(6), 362-366.
Carr, P., Glynn, R., Dineen, B., & Kropmans, T. (2010). A pilot intravenous cannulation team: An Irish perspective. British Journal of Nursing, 19(10), 19-20.
Finkler, S., Jones, C., & Kovner, C. (2012). Financial management for nurse managers and executives (4th ed.). Amsterdam, Netherlands: Elsevier Health Sciences.
Gopal, K., Fitzsimmons, L., & Lawrence, J. (2006). Nurse-led central venous catheter Service: Christie experience. British Journal of Radiology, 79(4), 762-765.
Hadaway, L. (2010). Development of an infusion alliance. Journal of Infusion Nursing, 33(5), 278-290.
Hawes, M. (2007). A proactive approach to combating venous depletion in the hospital setting. Journal of Infusion Nursing, 30(1), 33-44.
Kelly, L. (2009). Crossing professional boundaries: nurse-led catheter insertion. Nurse Manager, 16(6), 32-37.
Silva, G., Priebe, S., & Dias, F. (2010). Benefits of establishing an intravenous team and the standardization of peripheral intravenous catheters. Journal of Infusion Nursing, 33(3), 156-160.
Wagner, J. (2009). The impact of a dedicated IV team. Critical Care Nurse, 29(2), 12-19.