After discovering that Lewis Blackman had pectus excavatum, his parents decided to have him undergo surgery at a university medical center. Lewis was prescribed painkillers and ketorolac to help ease the excruciating pain he was in the following surgery. On day three, Lewis started having severe stomach discomfort, which the nurses eventually identified as ileus (Quality and Safety Education for Nurses, 2019).
The patient deteriorated, his blood pressure fell, and he became cyanotic. However, no experienced physician was ever consulted by the nurses and residents about the patient’s condition. The patient died, and according to the postmortem results, he developed a perforated duodenal ulcer. A sentinel events diagram will be used to analyze the four-day events which Lewis Blackman underwent before his death due to septic shock.
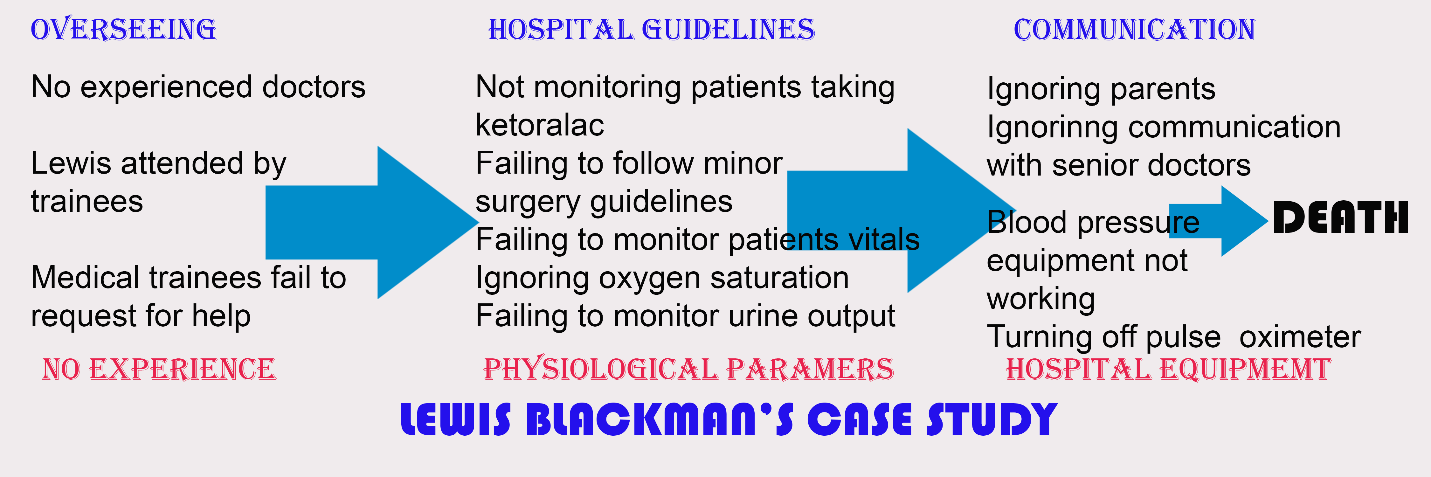
The problem is that Lewis died from septic shock on the fourth day following his operation. The events include a lack of oversight, inexperienced doctors responsible for Lewis’s care, hospital procedures, inaccurate vital readings, poor communication, and inadequate hospital machines (Quality and Safety Education for Nurses, 2019). As a result, trainees at this facility likely failed to correctly diagnose conditions or check patients’ vital signs since they were given unsupervised access to the patient’s details.
Lewis was admitted to a teaching medical center, implying that many doctors working there were in their initial years of medical school or residency. The patient’s reduced oxygen concentration was first ascribed to asthma. Therefore, no one took his condition seriously, and the pulse oximeter was reduced to 85% and ultimately switched off by the nurse (Quality and Safety Education for Nurses, 2019).
Due to the high risk of perforation, duodenal ulcers are one of ketorolac’s most severe side effects. The patient was given an IV dose of pain medicine without being adequately hydrated or understanding the possible risks of the drug (Solid Line Media, 2014). The doctors and nurses should have seen whether the drug impacted this patient, but they did not. The doctors failed to consult with more experienced colleagues and paid little attention to parents’ complaints about a decline in their patient’s urination. The patient had a septic shock and died on the fourth day after surgery.
Even after they could not take Lewis’s blood pressure, the personnel still did not contact senior physicians to evaluate the patient’s physiological parameters. Miscommunication was a significant issue since Lewis’s parents were worried about his decreasing urination on the last day, yet the staff ignored them (Quality and Safety Education for Nurses, 2019). Furthermore, there was a lack of clear communication between the medical team and the parents throughout this case. The lack of adequate monitoring at the training facility and the difficulty of the young doctors admitting their inexperience are the root causes of neglect. On the final day, the nurse failed to recognize that Lewis’s complaints were not typical surgical adverse effects. The nurse and the concerned medical personnel were supposed to seek advice from senior doctors regarding this atypical pain.
Given the patient’s symptoms, a competent physician would have ordered a basic blood test, which would have revealed the presence of gastrointestinal bleeding. This is a problem in the health sector since medical experts are scarce, so young and inexperienced physicians are not supervised. It is suggested that the possible adverse effects of ketorolac be emphasized in hospital policy. Young residents should be more responsible for notifying attending doctors of significant changes in a patient’s physiological parameters. Patients and their relatives must be informed of their condition, procedures performed, treatment, and other options available.
References
Quality and Safety Education for Nurses. (2019). The Lewis Blackman story. Web.
Solid Line Media. (2014). Transparent health – Lewis Blackman story. YouTube. Web.