The current situation I intend to impact is making hospice residency and interaction a pleasant experience for all patients and family. Since hospice care involves making a patient near the end of life comfortable, there are various issues that family and caregivers should address to make the process smooth (Center for Hospice Care, 2019). When I achieve the desired outcome, patients and relatives, involved in the interaction with hospice should receive a pleasant experience. Patients and families should get services, which consist of handling documents, care, communication from responsible people.
Several behaviors require changes; first is how medical executives recognize and respond to changes in a patient’s behavior pattern, which should be done in a timely and proactive manner. The second is working behavior with the family that requires an understanding of the family’s needs and reflection (Thompson & McClement, 2019). The third is having a positive attitude toward the care of the dying, which some employees lack. Before the behavior changes, responsible people should have a thorough knowledge of managing patients and addressing their physical and psychosocial needs, and how to communicate with families to inform them properly about all activities involved.
Person-centered palliative care training should be established to cause the necessary changes in employees’ behavior so that nurses will get a comprehensive understanding of patient’s and families’ needs, preferences, and individual differences. Furthermore, education workshops should be created to cover the main aspects, which can be among parties’ main struggles, including pain, depression, etc. (“Palliative care,” 2017). Finally, self and peer assessment should be made. The following resources would be needed: time of employees and internal trainers, paper and online materials for the workshops and assessment, additional external trainers’ fees, financial help in case of required maintenance for the process.
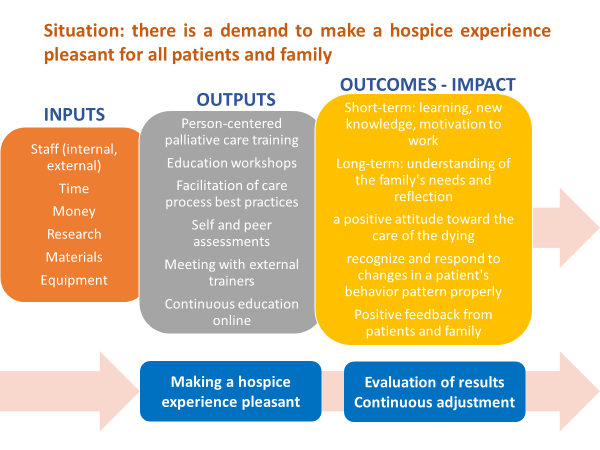
Situation: there is a demand to make a hospice experience pleasant for all patients and family
Inputs: staff (internal, external), time, money, research, materials, and equipment.
Outputs: person-centered palliative care training, education workshops, facilitation of care process best practices, self and peer assessments, meeting with external trainers, continuous education online
Target audience: hospice employees, patients, families
Outcomes: short-term: raising awareness and learning, knowledge building for medical executives, families, patients, motivation to work for nurses; long-term: understanding of the family’s needs and reflection, a positive attitude toward the care of the dying, recognize and respond to changes in a patient’s behavior pattern properly, positive feedback from patients and family
Main impact: making a hospice experience pleasant
Assumptions: patients near the end of life require the same level of care; families of patients are under stress; some medical employees may not have a comprehensive education to treat palliative patients or the right attitude towards the situation
External factors: external support, sharing best practices, changes in the socio-economic situation in the hospice.
References
Center for Hospice Care. (2019). Patient/family handbook for hospice care. Web.
Palliative care. (2017). The College of Family Physicians of Canada. Web.
Thompson, G.N. &McClement, S.E. (2019). Critical nursing and health care aide behaviors in care of the nursing home resident dying with dementia. BMC Nurs 18(59). Web.