Introduction
Blindness is a disabling condition with different causes and etiologies. One of the commonest causes of blindness is cataracts, which is the leading cause of preventable blindness throughout the world (Rose 2009). This condition has multiple etiologies and can develop at any age. In addition, the cause and progress of cataracts influence the management of the condition. A specialist ophthalmic nurse (SON) has a role to play in the management of patients with this condition. The occurrence of cataracts in a diabetic patient increases the chances of blindness (Rose 2009; Ring 2012). This essay discusses the role of a specialist ophthalmic nurse in the care of a diabetic cataract patient.
Rationale
Cataract is the most important cause of preventable blindness mainly in the developing nations. On the other hand, diabetes is a condition that commonly results in blindness in patients living in developed nations (Pager & McCluskey 2004). The combination of these conditions in a patient significantly increases the risk of blindness. These conditions are a threat to vision in any age group. Consequently, the care of patients with these conditions requires specialized professionals that can actively manage them and prevent blindness.
Epidemiology
Diabetes is increasing in prevalence with the age of onset of this condition decreasing (Hopley, Carter & Mitchell 2003). The WHO estimates that over two million UK citizens (4% of the population) are affected by this condition (Hopley, Carter & Mitchell 2003). A larger number of citizens are also affected by the condition although they are not aware. The number of teenagers affected by the condition is also increasing, with most of these having type I diabetes (Hopley, Carter & Mitchell 2003).
Table showing the diabetes prevalence :
Reflective Account
The trigger for choosing this essay topic was from the reflective report of the pre-operative check in the eye ward of an 86-year-old Diabetic patient for cataract surgery. This woman (referred here as Mrs. B for privacy reasons) came to the hospital to attend her cataract surgery that was scheduled for that day. She was in the company of her daughter. The surgery was delayed and later scheduled for the afternoon. Consequently, the daughter requested to be excused from the hospital and be called half an hour before the end of the procedure. A pre-operative assessment, including the integrated care pathway, revealed that Mrs. B was diabetic with normal sugars but was taking Warfarin tablets. A test to assess the coagulation status of the patient revealed that the INR was not within the therapeutic range prompting the cancelation of the operation.
According to Pesudovs and Coster (2008), deranged INR could predict profuse bleeding in patients undergoing surgery. This patient and her daughter were disappointed. A specialized ophthalmic nurse has a special role to play in the pre-operative assessment of these patients (Rahman, Rotchford, & Ramaesh 2013; Nightingale 1992). In addition, Rose (2009) states that health practitioners have the responsibility of fulfilling promises made to patients. Gibbs’s reflective cycle was used to analyze and evaluate issues.
Pathophysiology
Anatomy and Physiology
The eye is an organ that allows people to visualize their external environment. A functioning eye is necessary for the optimum survival of the species. Each of the different parts making the eye has a special role that contributes to normal vision (Douthwaite 1993). In fact, any abnormality with any of the components of the eye results in impaired vision. The lens is the structure affected by cataracts with eventual blindness (Kaufman 2003). This structure is crystalline with a biconvex shape resembling a magnifying glass (Marsden 2006). In addition, the lens is strategically located behind the pupil and the iris and serves to refract light entering the eyeball to the retina (Kaufman 2003).
Different researchers, ophthalmologists, and surgeons have described the anatomical position of the lens and the different functions that this structure serves. According to Kaufman (2003), the lens is nourished by different methods such as diffusion of nutrients from the aqueous fluid. The absence of blood vessels in the body of this structure ensures that it is clear and transparent to allow light to pass through to the retina. In addition, the cells forming the epithelium of the lens are arranged in a circular manner from the center. In addition, the cortex of this structure has fibrous cells spanning between the two epitheliums (Marsden 2006).
The PH balance of the lens is important to maintain. Consequently, this function is served by the diffusion of proteins from the surrounding aqueous fluid. In a diabetic patient, the metabolism of the lens is affected resulting in blindness. In a normal individual, the lens is made up of water and proteins (Pesudovs & Douglas 2008). In addition, this structure relies on glycolysis for the production of energy. This process is effective in young individuals but declines with a progressive increase in age. In addition, the maintenance of normal blood sugar is important for a normal eye.
In a diabetic patient, the control of blood sugar is often a problem with the sugar levels fluctuating. Hyperglycemia that is common in these patients interferes with the process of energy production in the lens resulting in the cataracts (Marsden 2006). The physiological function of the lens is to refract light to the retina at the back of the eye. For this purpose, the lens has crystalline proteins in the cortex with sodium-potassium pumps that facilitate the passage of electrolytes and other substances. Consequently, the sodium-potassium ion pumps contribute to the stability and refractive power of the lens.
Aside from the ion pumps on the epithelium of the lens, the ATPase enzyme contributes to the lens clarity (Marsden 2006). If the pumps are not working, the clarity of the lens may reduce. The electrolyte balance in the lens determines the PH and the clarity of the lens (Marsden 2006). The ATPase enzyme serves as a transporter exchanging intracellular ions (main sodium) for the extracellular ions (main potassium) (Marsden 2006). The balance between these electrolytes is important for normal lens functioning.
Treatment Modality
Surgery is the commonest and most effective modality for treating cataracts. Different surgical procedures have been described with each having an advantage over the others. The most common of these is the micro-incision Phacoemulsification procedure (Herbert 2009). Phacoemulsification surgery is a day procedure and begins with the incising of the cornea to access the lens. This incision provides an opening where the instrument used to carry out Phacoemulsification is inserted (Fedorowicz, Lawrence, & Gutierrez 2005). The device uses ultrasonic waves to damage the cataract followed by suctioning of the resultant materials. Finally, an intraocular lens is inserted into the eye.
Nursing Model
The nursing model that is utilized in this essay is the Orem Self-care model (1985). Diabetic patients with cataracts can be managed using this model. In this model, patients take care of themselves as far as possible and have a responsibility for their health (Hargraves 2001). Orem (1985) states that when patients cannot take care of themselves, they can be described as “self-care deficient”, and a nurse should take over their care. A nurse should provide this care to patients until the patients could be able to provide their care (Stollery & Shaw 2005).
The ability of patients with ocular problems to take care of themselves depends on their condition. These include the severity of the illness and the management procedures such as anesthetic techniques (Orem 1985). In addition, the specialist ophthalmic nurse has a role to play in the determination of patient needs. When these patients are helpless, the nurse should promptly provide the appropriate care to prevent complications and further progression of the disease (De Coster, Natalia, & Lorne 2007; Yanoff 2009). In addition, a specialist ophthalmic nurse provides an opportunity for patients to develop trust in their care providers.
Orem (1985) described different levels of self-care for patients with different conditions. SONs can use these levels to determine the care that a diabetic patient with cataract needs. First, the patient may be wholly compensated meaning that they are reliant on other individuals for their care. An example of this condition is the patient being under general anesthesia and is unable to do anything including breathing (Heise, Gonzalez, & Oetting 2006). These patients should have all their needs met while undergoing the surgery to ensure that complications do not arise and that the patient recovers faster (Fedorowicz, Lawrence, & Gutierrez 2005). SONs have the role of providing basic care and monitoring for these patients (Ahmed 2002; Yanoff 2009).
In the second Orem system category, patients are described as partially compensatory. An example of this level in the care of an ophthalmic patient with diabetes and cataracts is the patient is undergoing the surgical procedure (Charlton 1995). While the patient is not under general anesthesia, they cannot move. However, they can perform basic functions such as maintaining the airway and other body functions. While at this level, patients need to be secure and supported in all the necessary ways. In addition, these patients often require orientation since the eye that was operated on is often padded. The other form of support that these patients require is nutritional as they are cannot see clearly.
The third level of self-care, as described by the theorist, is the supportive/educative level (Orem & Taylor 2001). At this level, the patient is alert and can maintain self-care leaving the SON to provide education and other supportive care. The time before the theater and after the operation can be categorized at this level. Patients can be educated on the expected outcomes. In addition, the SON assesses the need for intervention in these patients.
Psychosocial Theory
The utilization of a psychosocial theory enables the provision of the best care for patients. The psychosocial theory that is appropriate to the provision of care for diabetic cataract patients is the locus of control theory (Rotter 1966). According to Rotter (1966), the management of patients is determined by internal forces (internal health locus control) and external forces (external health locus control). Diabetic patients can control their sugars adequately with minimal input from health care providers if they are taught very well (Lamoureux 2007). On the other hand, patients with diabetes can be reliant on their health care providers to manage themselves. The role of a SON is to ensure that these patients can manage their condition optimally.
Ocular Health Promotion
Ocular health promotion is necessary to ensure that patients do not develop ocular problems (Stephenson 1894). In addition, ocular health promotion prevents the complications of cataracts and their rapid development (Pesudovs & Coster 2008). One important part of ocular health is to ensure that individuals practice good hand hygiene. These patients also need to be taught how to maintain good eye drop compliance (Alva, Gray, Mihaylova, Leal, & Holman 2015). The role of a SON is to ensure good recovery after surgery. In addition, these individuals teach their patients how to stay healthy and maintain their blood sugar levels within normal. Several campaigns have been described in the attempt to reduce infection after ocular surgery (Erie, McHugh, Warner, & Erie 2011).
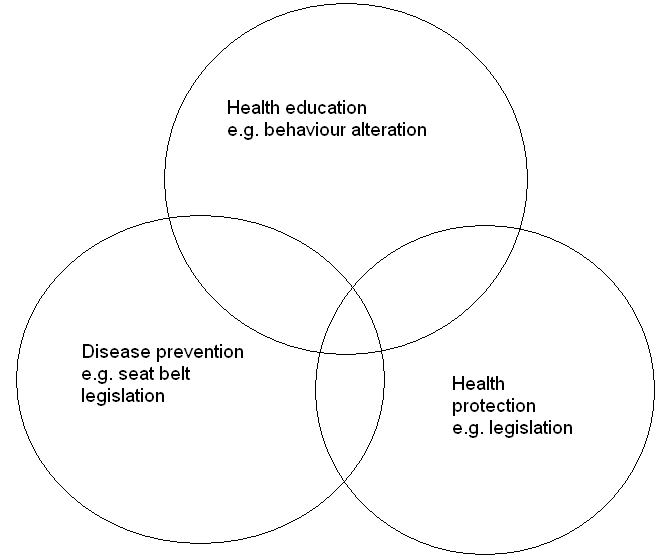
Postoperative complications of ocular surgery include endophthalmitis that is potentially blinding (Erie, McHugh, Warner, & Erie 2011). The framework utilized in health promotion is the Tannahill’s framework (Erie, McHugh, Warner, & Erie 2011). In this framework, the author describes different strategies such as health education, prevention, and protection (Kyari, Tafida, Sivasubramaniam, Murthy, Peto, & Gilbert 2014). For the model to be effective, therefore, the SON should be a good educator to provide basic care information for diabetic patients with cataracts. Other areas that the SON may educate their patients include control of their sugar levels, diet adjustments, and watching their weight.
Aside from education, the SON also needs to emphasize the need for screening programs (Murthy, John, Shamanna, & Pant 2012; Berman 2008). In addition, the SON needs to provide advice on the preoperative and postoperative care of the patients. Appropriate follow-up is necessary as these patients can develop complications. For this purpose, the patient needs to have a number that they can use to call the hospital in the event of a complication. If any of the complications develop, these patients can call and get information and instructions. In addition, SONs need to provide patients with instructions on how to manage their eyes while in their homes.
The complications of eye surgery can be prevented if the SON follows up on their patients. According to Watkinson and Seewoodhary (2015), appropriate follow-up includes the use of health records and home visits. Where a SON cannot carry out home visits, they need to utilize the social welfare department to ensure that there is an appropriate follow-up (Murthy, John, Shamanna, & Pant 2012). Institutions can also increase the number of SONs to ensure that there are enough of these individuals to provide primary care services. Additionally, these institutions need to provide additional resources for the SONs.
Professional Issue
The professional issue chosen is informed consent. According to Hardy (2009), informed consent is crucial in the management of any patient. Informed consent ensures that the rights of patients such as autonomy are respected (Hardy 2009). According to Hardy (2009), patients have the right to accept or decline medical intervention. The informed consent ensures that these patients make the right decisions and are aware of the procedures and their consequences. The SON should provide information to patients before their surgery and ensure that they understand the procedure.
Most health bodies such as the WHO and the Nursing and Midwifery Council hold nurses and other health care practitioners accountable for their actions and decisions (Orem & Taylor 2001). Informed consent is one of the tools used to provide information to patients. SONs provide patients with information on their condition, the risks involved, and the benefits of the surgical intervention. In addition, this form allows SONs to carry out an assessment of the patients. This form is a legal requirement for any surgery as it is a binding contract between the patient and the care providers (Hardy 2009).
SONs need to practice effective and efficient record keeping (Hardy 2009). Patient information is recorded for use in future encounters and to aid in the management of these patients (Hardy 2009). Registered nurses need to practice appropriate record-keeping so that they can effectively manage patients (Shietty 2003). In addition, the health institutions need to embrace the use of the health information system to store patient information. The role of a SON in the management of patient information includes recording and retrieval of this information. In addition, SONs attempt to utilize patient information to provide appropriate care. The provision of information to patients is necessary to prevent the development of complications after surgery.
Conclusion
In conclusion, specialized ophthalmic nurses have a special role to play in the management of patients with diabetes and cataracts. This essay discusses the etiology and management of cataracts in diabetic patients. It utilizes the Orem self-care model to explain the different roles of SONs in the management of these patients. The different levels described should be taken into consideration when managing and supporting these patients.
Recommendations
Several recommendations are possible from the reflection and the assessment of nurses’ roles in the management of diabetic cataract patients. First, SONs should be trained on how to educate their patients. Training should be on how to assess patients before they undergo any surgery. Secondly, nurses have the responsibility of informing patients of the procedure they will undergo and its consequences. The last recommendation is that SONs need to adopt the latest technologies in the management of patient information.
References
Ahmed, I 2002, ‘Revisiting early postoperative follow-up after phacoemulsification.’ Journal of Cataract & Refractive Surgery, vol. 28, no. 1, pp. 100-108.
Alva, M, Gray, A, Mihaylova, B, Leal, J, & Holman, R 2015, ‘The impact of diabetes-related complications on healthcare costs: new results from the UKPDS (UKPDS 84)’, Diabetic Medicine, vol. 32, no. 4, pp. 459-466,
Charlton, J 1995, Ophthalmic surgery complications: Prevention and management. Lippincott, Philadelphia.
De Coster, C, Natalia, D, & Lorne B 2007, ‘Health care utilization for injury in cataract surgery patients.’ Canadian Journal of Ophthalmology/Journal Canadien d’Ophtalmologie, vol. 42, no. 4, pp. 567-572.
Douthwaite, W 1993, Cataract: Detection, measurement, and management in optometric practice, Boston: Butterworth-Heinemann.
Erie, A, McHugh, R, Warner, M, & Erie, J 2011, ‘Article: Model of anesthesia care that combines anesthesiologists and registered nurses during cataract surgery’, Journal of Cataract & Refractive Surgery, vol. 37, no. 1. pp. 481-485,
Fedorowicz, Z, Lawrence, D, & Gutierrez, P 2005, ’Day care versus in‐patient surgery for age‐related cataract.’ The Cochrane Library, vol. 13, no. 1, pp. 71-75.
Hardy, J 2009, ‘Supporting patients undergoing cataract extraction surgery’, Nursing Standard (Royal College Of Nursing (Great Britain): 1987), vol. 24, no. 14, pp. 51-56,
Hargraves, L 2001, ‘Adjusting for patient characteristics when analyzing reports from patients about hospital care.’ Medical care, vol. 39, no. 6, pp. 635-641
Herbert, E 2009, ‘Complications of phacoemulsification on the first postoperative day: can follow-up be safely changed?’ Journal of Cataract & Refractive Surgery, vol. 25, no. 7, pp. 985-988.
Hopley, C, Carter, R, & Mitchell, P 2003, ‘Measurement of the economic impact of visual impairment from age‐related macular degeneration in Australia.’ Clinical & experimental ophthalmology, vol. 31, no. 6. pp. 522-529.
Kaufman, P 2003, Adler’s physiology of the eye: Clinical application (10th ed.), St. Louis: Mosby.
Kyari, F, Tafida, A, Sivasubramaniam, S, Murthy, G, Peto, T, & Gilbert, C 2014, ‘Prevalence and risk factors for diabetes and diabetic retinopathy: results from the Nigeria national blindness and visual impairment survey’, BMC Public Health, vol. 14, no. 1, pp. 1092-1114,
Lamoureux, E 2007, ‘The effectiveness of low-vision rehabilitation on participation in daily living and quality of life.’ Investigative Ophthalmology & Visual Science, vol. 48, no. 4, pp. 1476-1482.
Marsden, J 2006, Ophthalmic care, Chichester, West Sussex, England: Wiley.
Murthy, G, John, N, Shamanna, B, & Pant, H 2012, ‘Elimination of avoidable blindness due to cataract: Where do we prioritize and how should we monitor this decade?’ Indian Journal of Ophthalmology, vol. 60, no. 5, pp. 438-445,
Orem, D, & Taylor, S 2001, Nursing: Concepts of practice (6th ed.), St. Louis: Mosby.
Pager, C, & McCluskey, P 2004, ‘Public versus private patient priorities and satisfaction in cataract surgery.” Clinical & experimental ophthalmology vol. 32, no. 5, pp. 482-487.
Pesudovs, K, & Coster, D 2008, ‘An instrument for assessment of subjective visual disability in cataract patients.’ British journal of ophthalmology, vol. 82, no. 6, pp 617-624.
Pesudovs, K, & Douglas J 2008, ‘An instrument for assessment of subjective visual disability in cataract patients.’ British journal of ophthalmology, vol. 82, no. 6, pp. 617-624.
Rahman, M, Rotchford, A, & Ramaesh, K 2013, ‘Catatrac: a novel red light-emitting diode device for screening cataracts in the developing world’, Eye, vol. 27, no. 1, pp. 37-41,
Ring, L 2012, A Handbook of Ophthalmic Nursing Standards and Procedures, M & K Update Keswick.
Rose, K 2009, ‘Management of day-surgery patients with cataract attending a peripheral ophthalmic clinic’. Eye vol. 13, no. 1, pp. 71-75.
Stephenson, S 1894, Ophthalmic nursing, Scientific Press, London.
Stollery, R., & Shaw, M 2005, Ophthalmic nursing (3rd ed.), Blackwell Pub, Oxford.
Tantri, A, Clark, C, Huber, P, Stark, C, Gillenwater, J, Keele, J, Spilger, N, Fitzpatrick, B, Heise, M, Gonzalez, J, & Oetting, T 2006, ‘Article: Anesthesia monitoring by registered nurses during cataract surgery: Assessment of need for intra-operative anesthesia consultation’, Journal Of Cataract & Refractive Surgery, vol. 32, pp. 1115-1118,
Watkinson, S, & Seewoodhary, R 2015, ‘Cataract management: effect on patients’ quality of life’, Nursing Standard, vol. 29, no. 21, pp. 42-48,
Berman, A 2008, Kozier & Erb’s fundamentals of nursing: Concepts, process, and practice (8th ed.), Pearson Prentice Hall Upper Saddle River, N.J.
Shietty, S 2003, Eye disease blepharitis, diabetes and your eyes, cataracts, North Sydney, NSW Health.
Nightingale, F 1992, Notes on nursing: What it is, and what it is not (Commemorative ed.), Lippincott, Philadelphia.
Yanoff, M 2009, Ophthalmology (3rd ed.), Mosby Elsevier, Edinburgh.