The Veteran Affairs (VA) health care organization deals with veterans that have been brought to the community hospitals. The key problem experienced by the organization and parties concerned includes poor quality of health care services provided to patients and escalating costs that can be considered one of the reasons for implementation of the Managed Care program aimed at reducing costs and making the management of resources more effective. So, the organization selects the tools for collection, evaluation, and displaying of data on the factors that should be measured to trace the improvement after implementation of the program. Collection of data should include collection of information about the patients and quality of services provided to them before implementation of the quality improvement methodology and after it. Besides, it is necessary to plan the evaluation of gaps and techniques aimed at elimination of gaps.
The methodology used to make the quality improvement process was chosen to make the changes more effective due to the well-planned activities of collection of data, evaluation of gaps, assessment of further necessary changes to be introduced. So, Six Sigma approach can be considered the most effective as it includes six stages created with regard to the cyclic nature of changes and operation of the organization. Though this approach can be rather effective in manufacturing, it appeared to be beneficial for health care organizations because they have customer orientation and should achieve such results as reduced costs, reduced length of stay, as well as reduced readmission rates gained with the help of improvement of quality of health care services provided.
Introduction
The organization under consideration is the Veterans Affairs (VA) system of hospitals that should provide veterans with adequate treatment at a reasonable price with regard to the quality of services. The services provided to veterans include managed Care aimed at reducing costs of health care services and improving quality in terms of better and more appropriate management of resources including human resources and financial resources such as operations and health care strategies claimed to be inappropriate. In this respect, the mission of the organization focuses on the improvement of the quality of health care services provided including reducing the length of the patients’ stay at hospital, reducing costs spent by veterans, and reducing the readmission rates by implementing more adequate treatment strategies such as diagnosing and observation. The quality of services provided to patients can be improved with the help of reports aimed at assessment of the situation (Ransom, 2008, p. 4). As stakeholders are patients, health care providers, and investors, it is necessary to take into account their needs and expectations from implementation of the improvement plan (Dlugacz, 2006, p. 76).
Objectives
The objective are goals of the organizations set to achieve the results indicated in the mission statement. In other words, it is necessary to introduce short-term and long-term goals that can serve as indicators of each stage of the quality improvement process. Responsiveness can be measured to assess the opinion of patients and health care providers including nursing staff and doctors. Another goal of the organization includes measuring the readmission rates before and after implementation of the quality improvement program with regard to the length of stay in different cases in terms of the seriousness of the disease and the number of times a patient was readmitted. Improvement of patients’ attitude to nursing staff and vice versa can be considered another key goal while applying the QI plan.
Scope
The main departments and programs involved into the quality improvement plan include nursing staff because they are the main health care providers for patients that have no complications and should be cared for steadily without making any interventions. As bringing veterans back to the Veterans Affairs system is the major goal of the organization together with implementation of changes to improve the treatment and make it more adequate, effective, and resource-efficient, it is necessary to evaluate the improvement in insurance, quality, responsiveness, and patient-orientation of the program. For instance, it is possible to use such methodology for implementation of quality improvement plan as Six Sigma approach aimed at measuring and displaying the improvements achieved with the help of the program, especially to monitor the cost-efficiency of health care services provided by the staff of VA hospitals (Dlugacz, 2006, p. 74).
Data Collection Tools
The data about the performance of the organization should be collected and evaluated in order to compare and contrast the situation before and after implementation of the quality improvement plan. In this respect, the main focus of the organization includes the reducing of the patients’ length of stay and reducing the readmission rates. In other words, the data to be collected it is necessary to collect information on the length of stay in each particular case in order to be able to analyze the situation in terms of the length of stay, treatment measures, period between the discharge and the readmission, and the number of readmissions the patient had before the implementation of the quality improvement methodology. Besides, certain data collection tools can be used in one case whereas they appear to be ineffective in others.
National Healthcare Quality Report (NHQR) Fact Sheet can be used to monitor the measures of treatment and preventive techniques. Sampling (IHI Tool) is necessary to assess the situation in the organization before implementation of quality improvement measures. Simple Data Collection Planning (IHI Tool) is probably the first tool that should be used because it is necessary for planning the improvement process in terms of gaps that should be identified in the organization and needs of stakeholders and the system in general. For instance, each separate case requires specific measures such as mortality ratio calculated with the help of monitoring and data collection tools (Knaus, Wagner, Zimmerman, & Draper, 1993, p. 754). Another tool that can be effectively used by the VA organization is the Scatter Diagram (IHI Tool) that can be applied for comparison and contrast of data to identify gaps and improvements achieved. Moreover, early readmission rates are closely connected to the quality of care; so, it is necessary to evaluate this factor (Ashton, et al. 1995).
QI Processes and Methodology
QI processes
The first process in the implementation of the quality improvement plan should be planning of the changes, identification of gaps, and assessment of the situation with staff members, patients and their attitude, and cost-efficiency in order to compare these data with results received after implementation. The next set of strategies applied to the organization should include collection of data on readmission rates and length of stay. Moreover, it is necessary to trace the tendencies in other health care organizations that have recently implemented changes and the way staff members reacted to changes. It is also possible to assess such indicators as current situation and potential gaps that may occur in the process of implementation and cause other problems (Ravishankar, 2008, p. 550).
Methodology
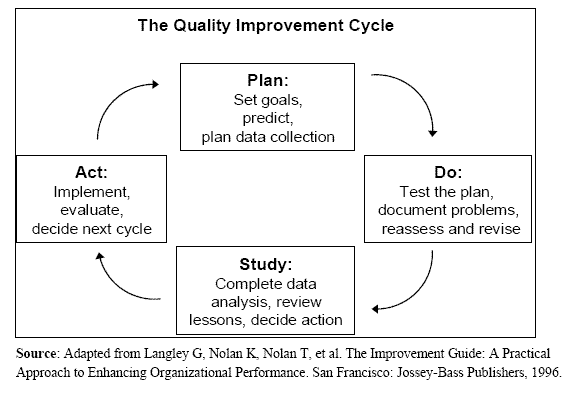
The organization can benefit from implementation of three methodologies such as Six Sigma, Plan Do Check Act (PDCA), or Customer Inspired Quality. All three methodologies mentioned above have their advantages and disadvantages that can be appropriate for one organization and ineffective in the other. In other words, other organizations involved into manufacturing can easily apply the Six Sigma or Plan Do Check Act (PDCA) methodologies while the Customer Inspired Quality is more appropriate for health care organizations as it combines techniques of different methodologies and uses a customer perspective to be more effective in terms of the health care operation (Moyers, Shaw, & New, 2006, n. p.).
Comparative Databases, Benchmarks, and Professional Practice Standards
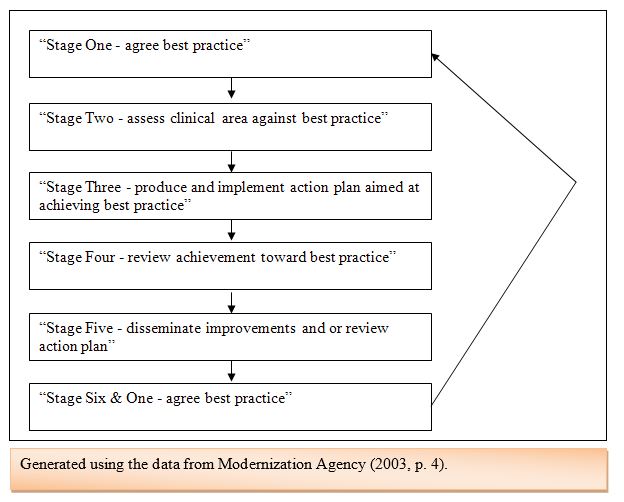
An annual report can be one of the most effective methodologies used by the Veterans Affairs health care organization in order to introduce quality improvement strategies and monitor the effectiveness of changes. This method can be appropriate for benchmarking in terms of comparing the national standards in health care with regard to quality improvement measures. In other words, Six Sigma approach can be used to make the quality improvement plan implementation more well-thought and organized in terms of potential gaps that may occur and expectations of patients and nursing staff that should be influenced by the implementation of a new program. Benchmarking is aimed at identifying the gaps in the QI plan because it mostly deals with quality ad costs and influences all stakeholders including patients, medical staff, and government. The milestones for indicators of quality improvement achieved after implementation of QI plan include such factors as application of the most appropriate technique, assessment of this technique for organization, creation of the plan aimed at achieving the goal, compare the most appropriate technique and the results of application, implement improvements to receive more effective results, and repeat the cycle (Modernization Agency, 2003, p. 4).
Authority/Structure/Organization
The implementation of the plan is the important stage of the improvement strategy and should be performed by the middle managers whereas all other staff members of the health care organization such as Quality Improvement Committee, medical staff, and department staff should contribute to the effectiveness of plan implementation through sharing information on the results of improvement plan, collecting data on the patients’ satisfaction, reporting about changes that can take place among staff members, and others.
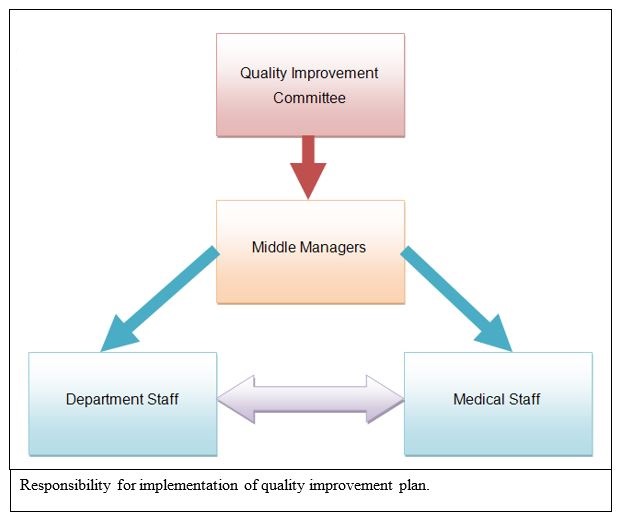
Moreover, leadership strategies should also be of great value in the process of quality improvement because staff members should strive for improvement of their skills in order to help adjust the system to the needs of patients. However, the responsibility for implementation should be on middle managers while the effectiveness of changes should be assessed by the Quality Improvement Committee members.
Communication
The results of the improvement are communicated by department staff members and medical staff members to middle managers who are responsible for implementation of the changes and evaluation of the effectiveness of measures taken. In this respect, middle managers report to the members of the Quality Improvement Committee who assess the results and make decisions concerning the further changes to be introduced or possible gaps to be evaluated and identified in the next stages of the plan implementation. In other words, the communication of results of the data evaluation and the situation with patients and staff members should be adequate and be performed in a timely manner to ensure that all members of the organization receive appropriate information on the progress of the changes taken.
Education
As the quality improvement plan may require certain skills of staff members improved, it is necessary to take into account the strategies used for implementation of changes and adjust the educational needs and capabilities of staff members to that data. In this respect, all members of department staff and medical staff should report to heads of their departments and to middle managers that organize reports for the Quality Improvement Committee members who make final decisions. So, reports and a clear approach while sharing information should be used to enable all staff members operate the data effectively without experiencing the lack of data for making adequate decisions. In other words, the education of staff members can include report techniques to make report analysis more effective in terms of the data collected and its influence on further decisions made.
Annual Evaluation
The annual evaluation of the effectiveness of the organization’s operation should be performed with regard to the indicators mentioned above. In other words, it is necessary to evaluate the organization in terms of the primary goals set and achieved including reducing of costs, reducing of length of stay, and reducing o readmission rates. So, such elements as readmission rates and length of stay compared to costs spent on every patient should be the basis for the annual reports and further improvements to be implemented.
Reference List
Ashton, C. M., Kuykendall, D. H., Johnson, M. L., Wray, N. P., and Wu, L. (1995). The association between the quality of inpatient care and early readmission. Annals of Internal Medicine, 122 (6), 415-421.
Knaus, W. A., Wagner, D. P., Zimmerman, J. E., and Draper, E. A. (1993). Variations in mortality and length of stay in intensive care units. Annals of Internal Medicine, 118 (10), 753-761.
Dlugacz, D. (2006). Measuring health care: Using quality data for operational, financial and clinical improvement. San Francisco, CA: Jossey Bass.
Modernization Agency. (2003). Essence of Care: Patient-focused benchmarks for clinical governance. Web.
Moyers, H., Shaw, J. G., and New, W. (2006). Methodology comparisons: Six Sigma, Lean, Theory of Constraints and Customer-Inspired® Quality. Web.
Ransom, E. R., Joshi, M. S., Nash, D. B., and Ransom, S. B. (2008). The healthcare quality book: Vision, strategy, and tools (2nd ed.). Chicago, IL: Health Administration Press.
Ravishankar, N. (2008). IT applications for healthcare: leverage processes for high quality. SetLabs Briefings (Sept.), 47-58.