Introduction
A patient’s fall is the inability to adequately “respond” to a loss of balance or a shift in the center of gravity. Falls in the elderly are among the most frequent causes of hospitalization and are associated with an increased risk of injury, including hip fractures, subdural hematomas, or death (Dykes et al., 2020). Numerous studies have shown that patient—and family-centered strategies significantly reduce falls and injuries in older adults. This statement must be confirmed theoretically and practically. This paper uses the PICOT question format and recent research to focus on evidence-based nursing practice for fall prevention in the hospital.
PICO(T) Question
Among hospitalized patients 65 and older (P), would a patient-centered approach (I) be more effective compared to the usual fall prevention approach (C) in reducing falls-related outcomes (O) for about one month (T)?
Methods/Current Practice
Key Words Searched
Falls, hospital, prevention, intervention, the patient-centered approach, the usual fall prevention approach, and patient safety.
Search Engines Used
Using keywords and index terms on Google Scholar, PubMed, ProQuest, and JAMA Network.
Tables/Figures
Results/Opportunities for Improvement
The practice project resulted in the following conclusions: A patient-centered approach to fall prevention is more efficient and effective than a standardized, usual process. Notably, this approach aligns with the International Classification of Functioning, Disability, and Health (ICF) established by the World Health Organization (Honaker, 2021). It considers a patient’s characteristics, adapting to their specific needs, desires, and preferences. Compared to a similar approach, a patient-centered method raises patient awareness of fall risks and related prevention strategies (Fowler & Reising, 2021).
Depending on the degree of criticality of the fall risk, specific nursing interventions are used: starting with familiarizing a patient with the environment and demonstrating to them a call light to the use of yellow wristbands for patients so that a nurse can be in a ward at all times, providing uninterrupted assistance and support (Fowler & Reising, 2021). Indeed, noticeable results can be seen after a month of using a patient-centered approach. However, it will take longer for older adults (65 and older) to feel more relaxed and unafraid to move around without assistance.
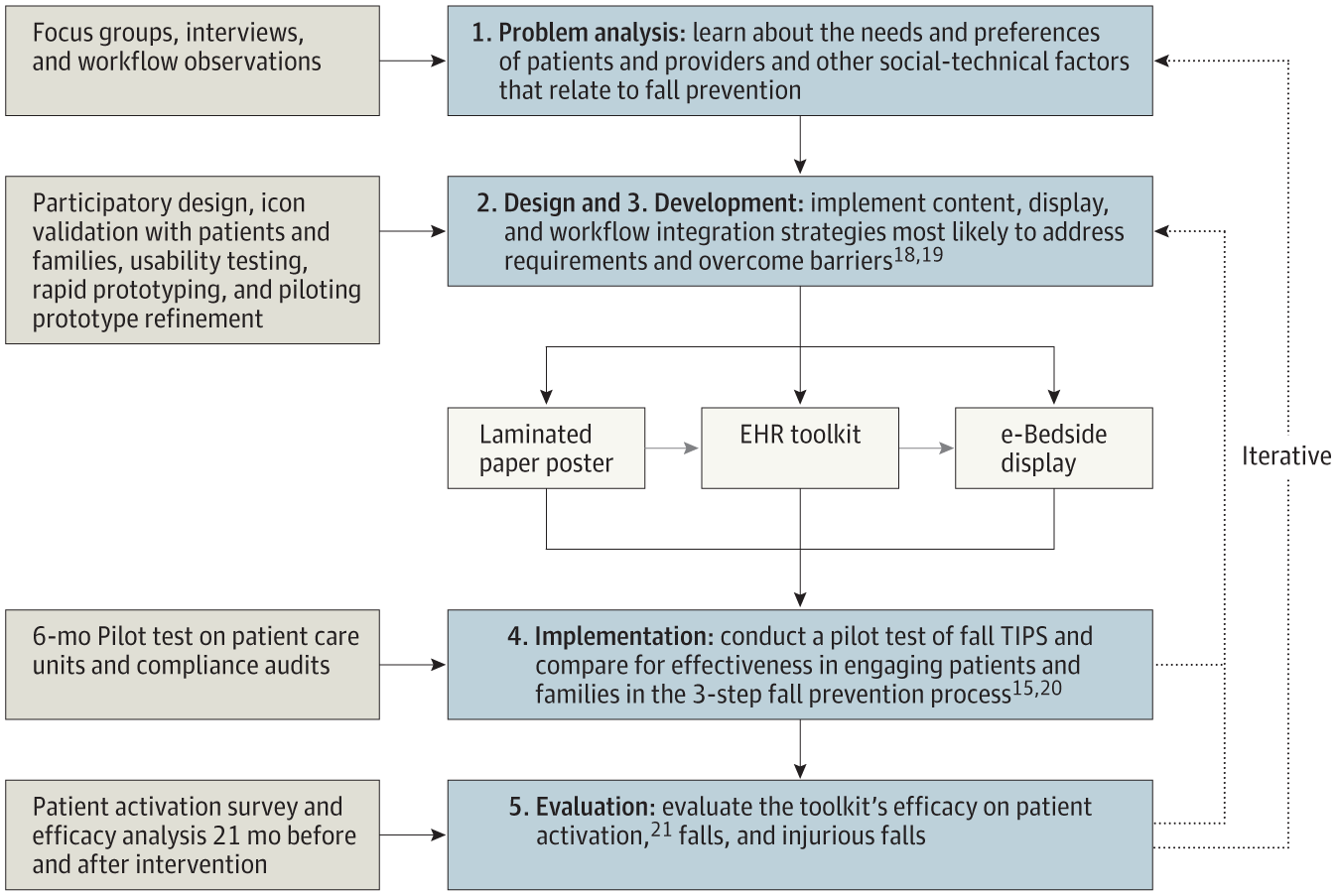
Other authors express the same results as Fowler and Reising. According to Dykes et al. (2020), a patient-centered approach is remarkable in linking patient-specific risk factors with interventions most efficient to prevent falls. Unlike the standardized approach, it bridges the disparity between nursing fall risk assessment, individual fall prevention interventions, and patient engagement in fall prevention simultaneously in a short period (Dykes et al., 2020).
Conversations with the patient and focusing on an individualized approach will help guide elders and their loved ones toward better health and well-being (Honaker, 2021). Nonetheless, confirming these words would require more in-depth research based on observations and experiments.
Conclusions
In conclusion, the primary goals and objectives of the practice project were successfully achieved. The PICO(T) Question and literature review provided the basis for precise and reliable conclusions. In contrast to the standard fall prevention approach, a patient-centered approach allows elderly patients to face less risk of falls. Implementing this approach for at least one month is reasonable for seeing desirable results.
References
Dykes, P. C., Burns, Z., Adelman, J., Benneyan, J., Bogaisky, M., Carter, E., Ergai, A., Lindros, M.E., Lipsitz, S.R., Scanlan, M., Shaykevich, S., & Bates, D. W. (2020). Evaluation of a patient-centered fall-prevention tool kit to reduce falls and injuries: a nonrandomized controlled trial. JAMA Network Open, 3(11), 1-22. Web.
Fowler, S. B., & Reising, E. S. (2021). A replication study of Fall TIPS (Tailoring Interventions for Patient Safety): A patient-centered fall prevention toolkit. MedSurg Nursing, 30(1), 28-34. Web.
Honaker, J. (2021). Fall prevention: patient-centered outcomes. American Speech-Language-Hearing Association. Web.