Introduction
The patient pathway or journey, also called the clinical pathway (CPW) is a medical jargon. It refers to the route followed by a sick person from the first encounter with a healthcare provider through referral to treatment completion (Aspland, Gartner, and Harper, 2021; Rogers, et al., 2019). In the context of cardiac physiology, it refers to the patient’s journey from symptoms onset to pacemaker implantation, covering presentation to secondary care, documentation of pacing indication, and referral (Rana and Afzal, 2019). In some instances, it covers the period from entry into a treatment center or hospital to discharge.
Formalizing the care pathway is advantageous for various reasons. First, it increases diagnostic efficiency and facilitates treatment commencement (Gorlicki, J., et al, 2020). For example, in cardiac physiology, it can reduce delays from documenting pacing indication to permanent pacemaker implantation. Second, formalized patient pathways ensure increased care consistency, reduced medical error risks, and decreased care costs. Extensive collaboration and input from all stakeholders, including medical practitioners and patients and their families, is needed to develop an evidence-based care pathway. According to Rotter et al (2019), although the approach does not necessarily affect in-hospital mortality or readmission, it reduces in-hospital costs, resulting in better healthcare per spent dollar. Successful implementation of CPWs requires careful consideration about barriers to change and existing facilitators.
Utilization of Patient Pathway
Medical practitioners utilize patient pathways as tools for guiding evidence-based care. In cardiac physiology, they translate clinical practice recommendations into care processes within the peculiar hospital or treatment center’s culture and environment (Rotter et al., 2019). Because it is a structured care plan, clinicians use patient pathways to translate medical guidelines into local processes, identify and detail the appropriate treatment course’s steps, and standardize care for cardiac physiology or any other clinical problem. Not surprisingly, the use of clinical pathways has been growing exponentially in many parts of the world. For example, in Europe, utilization of the approach begun in the 1990s and in 2004, the largest clinical pathways professional organization – the European Pathways Association (EPA) – was founded. EPA’s goal is to support the creation, implementation, monitoring, and evaluation of care pathways in Europe (Rotter, et al., 2019). In 2018, EPA had members in more than 50 countries, indicating its increasing importance in healthcare.
Case Study
Patient Information and Background
In June 2015, a 75-year female patient presented to the hospital with dizziness and palpitations. An ambulatory 24-hour electrocardiogram (ECG) report showed three short episodes of nocturnal sinus bradycardia with rare ventricular and supra-ventricular ectopics. On day four and six of a seven-day recording, ECG showed sinus rhythm with periods of sinus bradycardia and diurnal sinus pauses, with the longest pause being 3.5 seconds at 09:35 hours. The ECG also recorded rare supra-ventricular aberrant beats.
The patient’s symptoms at onset were palpitations and dizziness. However, with the passage of time, the symptoms worsened, with sinus pauses detected in 7 days ambulatory ECG recordings after the patient lost consciousness in syncopal episodes. 12 lead ECG showed unclear junctional rhythm p wave. Possible heart blocks on ECG also showing an indication for pacing according to American Heart Association (AHA) class 1 guideline (2018). Patient diagnosis included atrial fibrillation (AF) and paroxysmal Atrial fibrillation (PAF), both of which are Indicative of pacing. The patient has history of Parkinson’s disease, osteoarthritis, cholesterol, osteoporosis, white coat hypertension (WCH), and deafness (stapedectomy).
Symptoms Onset to Presentation to Secondary Care
Timing of first symptom could not be reliably determined for the patient. Likely, the interval from the time of the initial onset of the symptoms to presentation in hospital was long given the patient’s age. For most people, presentation to the hospital after the initial onset of symptoms is four weeks. For some, presentation in hospital happen after a previous case of hospitalization due to dizziness or syncope suggestive of bradycardia during in-patient care for other problems (Long and Koyfman, 2017; Koza et al., 2017). Notably, older patients may have other complications that force them to visit the hospital, and diagnosis during such hospital visits may reveal other conditions.
Secondary Care Presentation to Documentation of Pacing Indication
The case study patient’s interval between secondary care presentation and documentation of pacing indication was quite long. Part of the reason was that the patient needed elective pacing (and not urgent pacing) to improve the quality of her life after the initial palpitations, dizziness, and hear-beat pauses worsened. Leading symptoms for both urgent and elective pacing referrals include syncope (accounting for more than 50 percent of the cases), dizziness, and dyspnea (Sandhu and Sheldon, 2019; Kam, 2020). Urgently paced patients also tend to have a high complete heart block incidence and lower second-degree heart block incidence.
Documentation of Pacing Indication to Referral
Because the patient needed elective pacing, time to referral was significantly long. Summarily, symptoms onset to presentation in the healthcare sector took about three months, hospital presentation to pacing indication documentation took about two and a half months, and documentation of pacing indication to referral took about 35 days.
Referral to PPM Implantation
Referral to permanent pacer implantation was the final stage of the patient’s clinical pathway and took about 10 days. The actual implantation of the permanent pace marker occurred January 11, 2016, which was about seven months from the time the patient presented herself to hospital with palpitation and dizziness (1.e., 2015, June). The relative delay in the implantation of the pace maker was due to various reasons. One of them is that during the initial diagnosis, the patient’s symptoms were less serious, and the medical practitioner assured the patient that her conditioned would be monitored closely and appropriate treatment recommended. As the symptoms worsened, it became necessary to have the pacer implanted.
Tests Performed According to National Institute of Care Excellence Guidelines
Tests performed include electrocardiogram (ECG) and a transthoracic echocardiogram (TTE) procedure. The ECG test was used to record the electrical activity of the patient’s heart at rest. It provided information about the patient’s heart rhythm and rate and detected diurnal pauses, sinus bradycardia, and atrial infarction. The TTE procedure checked the heart’s chambers and blood vessels for abnormalities.
American Heart Association-Based Treatment
The patient was treated with an elective dual-chamber, rate-modulated mode (DDDR) permanent pace maker (PPM) implant indicated for heart block. The documented sinus bradycardia and diurnal pauses are also indication for pacing. The holter report from the time the patient presented to the hospital until implantation provided additional evidence for implantation of the DDDR permanent pace maker.
Patient Readmission
In 2018, the patient was re-admitted to hospital, about three years after the implantation of the pace maker, suggesting that the device did not work as planned. Notably, the device has an average lifespan of six years, which means that it was due for replacement in January 2021 (since it was implanted in January 2016).
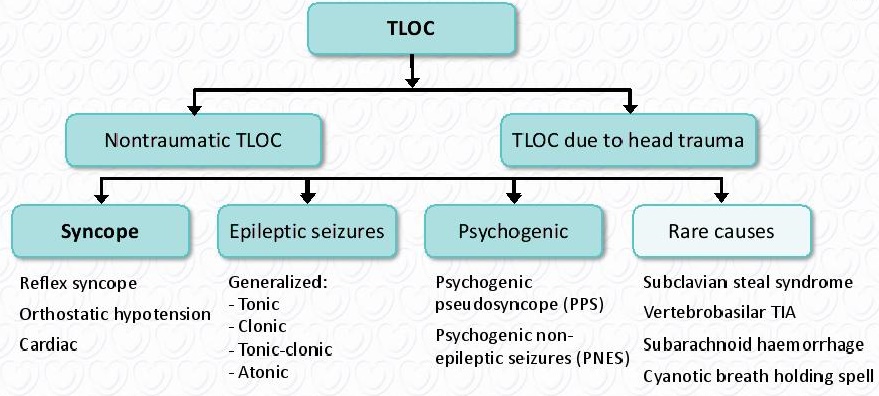
2018 ESC Guidelines for the diagnosis and management of syncope
As shown in Figure 1, syncope is a form of transient loss of consciousness (TLOC) and the medical term for fainting. It is often due to transient global cerebral hypoperfusion, characterized by rapid onset, short duration, and spontaneous complete recovery (Saurer, Mezler-Andelberg, and Weihs, 2019; Moloney, Romero-Ortuno, and Kenny, 2021). Notably, transient loss of consciousness is the real or apparent loss of consciousness typified by amnesia, loss of responsiveness, abnormal motor control, and a short duration. TOLC is syncope when reflex, orthostatic hypotension, or cardiac syncope features are present and attributes specific to other TLOC forms are absent.
Diagnosis of syncope’s starting point is the initial evaluation, which consists of history taking, physical examination, and electrocardiogram. Based on these findings, a medical practitioner may perform additional examinations if a need to do so arises. An immediate ECG monitoring is necessary when arrhythmic syncope is suspected (Ghariq et al., 2021; Gehi and Narla, 2018). Echocardiogram if previous known heart disease data is available. Carotid sinus massage, head-up tilt, and blood tests may be performed as more information about the syncope episode become available (El-Hussein and Cuncannon, 2021; Drago, 2018). These procedures are based on evidence and lead to different forms of treatment recommendations.
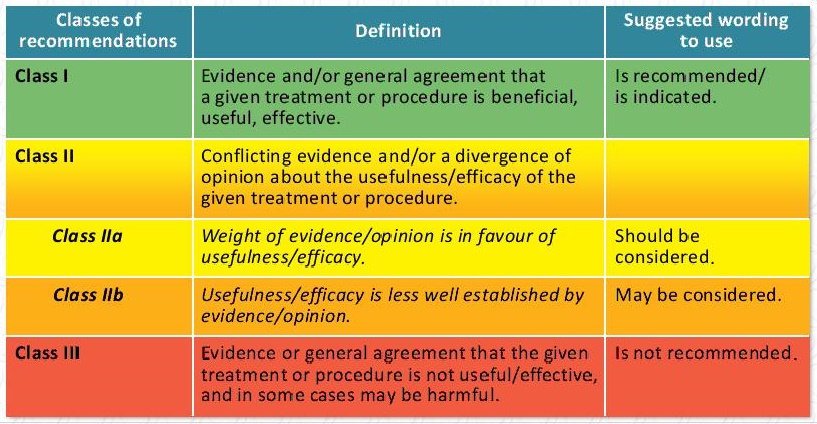
The European Society of Cardiology (ESC) has five classes of recommendations for syncope management and three levels of evidence. The five classes of recommendations include Class I, Class II, Class IIa, Class IIb, and Class III (Doman, Kisling, and Fentanes, 2021). Figure 2 below summarizes these classes and their definitions.
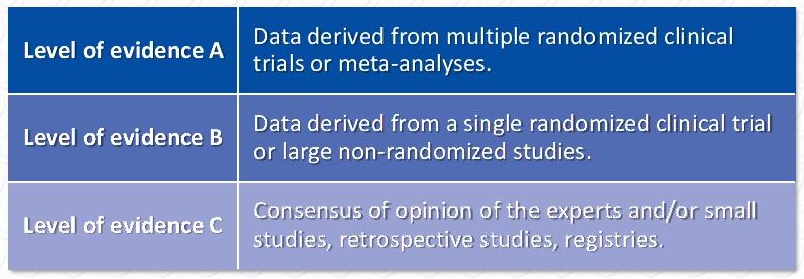
The levels of evidence measure the reliability of a given treatment approach. They range from Level A to Level C and should be considered when making treatment decisions (Ali and Grossman, 2017). Figure 3 below summarizes the three levels of evidence according to the 2018 ESC guidelines.
Examination of the Case Study According to Guidelines
Guidelines were followed in the treatment of the patient, including the implantation of the pace maker. However, the treatment did not result in desirable outcomes since the patient was readmitted to hospital in 2018. Further information on the case are examined below.
Guidelines
As per the AHA guidelines (2016), syncope is referred to mean a transient loss of consciousness (T-LOC) that result from a cerebral hypo-perfusion (Brignole et al., 2018, pp.1883). In most cases, T-LOC can be characterized by acute onset, short duration, and sometimes a spontaneous recovery from the symptoms. As the ESC guidelines reports (2018), T-LOC is the state of the real or apparent loss of consciousness with loss of awareness as characterized by forgetfulness within the unconscious state, uncontrolled motor reflexes, numbness in a short occurrence period (Gregoratos et al., 1998). Having an inter-professional team of care providers in the management of syncope has been indicated to be effective, as the team includes members including cardiologists, physicians, neurologists, and geriatric medicine, and nursing care professionals (Kryuchkova et al., 2018,p.1). According to Goldberger et al. (2019), a multidisciplinary team is useful in addressing syncope’s wider spectrum more effectively to relieve the transient loss of consciousness (TLOC). As per the AHA/NICE guidelines (2018), the diagnosis of syncope includes careful history taking, a closer clinic assessment, including lying down or when upright, and taking an electrocardiogram (Shen and Sheldon, 2017; Shen et al., 2017). Thus, most of the guidelines were observed in the case study.
The AHA 2016 guidelines require that syncope diagnosis considers the patient’s history, highlighting any family history of syncope and identifying any childhood tendencies of syncope (Brignole et al., 2018). Occurrence as either of short duration or of rapid onset, the recovery status of the patient and the state of the patients’ postural abilities (Brignole et al., 2018). By positively answering the above key determinant questions, the diagnosis of a possible syncope is rendered complete. Among the elderly, the development of syncope can be from several risk factors with the inclusion of prescription medications, medication withdrawal as well as reductions in motor functionalities (Cunnington et al., 2008). Many of the elderly patients present with cognitive problems, and as such, the evaluation of the patient’s locomotor and neurological problems, which includes the determination of the patient’s gait balance, is indicative (Gregoratos et al., 1998. p.1176). The elderly female patients’ condition was dire and needed urgent medical intervention, as is in the cardiovascular syncope state.
The patients’ blood pressure was high than normal in an overweight state (Rogers et al., 2019, pp.266). The diagnostics that were done considered electrocardiogram, which has been reported to be standard practice as syncope can be clinically diagnosed by using the electrocardiogram, the carotid massage, and the orthostatic testing mechanisms as determinants of the various causes of syncope among cardiac patients (Sutton, 2017, pp.554; Sutton, Ricci, and Fedorowski, 2020). The management plan also requested an echo after the ECG, which was also a standard management practice in the syncope pathway (Zimmermann et al., 2021, p.1). According to Wilson et al. (2018, pp.55), the American Heart Association indicates that the evaluation of syncope with echocardiography is a class II indication. As a result, the management of syncope should consider all diagnostic options.
In the syncope pathway AHA guidelines (2018), tests done must include an electrocardiogram alongside an Echo though these come at higher costs, blood tests including blood glucose levels, and urea plus electrolytes (Goldberger et al., 2019). However, dizziness is reported to have persisted in the disease management, which could have warranted the ‘patient’s referral to the ENT or neurology for possible differentials from cardiac causes (Brignole et al., 2018). The AHA guidelines (2016) also indicate patient clinical examination as being huge in the management of syncope patients (Brignole et al., 2018). In this regard, the heart murmurs reported were properly diagnosed, besides determining the patient’s blood pressure, with systolic at above 90mmHg. The treatment of cardiac syncope makes use of therapies that offered relief to the specific arrhythmia, and the study focused on treating the syncope.
Benefits of the Tests to the Patient
The patient was elderly, and therefore, these interventions could have proven beneficial for managing the patient’s condition. Furthermore, De Ruiter et al. (2018) note that elderly persons are at more risk of developing syncope syndrome as a result of the increased risks of blood flow changes within the cerebral blood vessels. Studies have indicated that Holter monitoring is a preference for recurrent syncope or pre-syncope occurrences of a frequency above one episode weekly (Rana, and Afzal, 2019). However, this test was not conducted despite its proven role in changing the course of syncope-related cardiac problems.
Something Else that Could Have Been Done
According to the ESC guidelines (2018), Tilt testing as a concept in determining the presence or the potential of developing low blood pressure was not conducted in the present patient case study (Brignole et al., 2018, pp.1883). The ESC guidelines (2018) also recommend the use of video materials in recording for admitted patients suspected of developing syncope, which could have been indicated for the patient. The diagnosis criteria for syncope in the patient could have made use of the syncope etiological diagnosis indications. Etiological concerns of syncope development indicate that critical questions should be asked, including questions intending to identify the circumstances just before the attack, including the patient’s position and activity (Cunnington et al., 2008). Questions about the onset of the attack, if there had been any witnesses, the end of the attack, and questions intending to establish the patient’s background.
The ESC (2018) guidelines indicate that diagnostic tests for syncope should include a carotid sinus massage, orthostatic challenges, electrocardiographic monitoring (both invasive and non-invasive), and electrophysiological study(Gregoratos et al., 1998. p.1176). In addition to these tests, adenosine triphosphate tests, the exercise stress tests, a psychiatric evaluation, and cardiac catheterization, besides the echocardiographic amongst other imaging techniques, should be used. In the case study, only the ECG was used as a diagnostic measure.
However, the intervention could have considered other options for this elderly patient, given the increased risk of falls associated with cardiac syncope among the elderly. According to McDermott and Quinn (2016), common lab tests, with the inclusion of a complete blood count, could have been useful in determining basic synoptic factors. CT scans and MRIs have also been used in many instances as a means of detecting cardiac conditions, including congenital heart conditions. According to the syncope guidelines (2018), for patients above the age of 40 years, it is important to conduct a carotid sinus massage. The carotid massage (CSM) could have been useful in this 79-year-old lady (Goldberger et al., 2019).
According to Oberman and Bhardwaj (2020), nearly half of all patients presenting with syncope in the emergency room ought to be admitted. Regardless, this patient was not admitted for in-patient management as should have been the best practice while following the protocol. In current medical practice, technology is increasingly being used to address some challenges, including the challenges of staffing. Anderson et al. (2018) note that patient monitoring can be achieved remotely from the patient’s comfort through the use of video recorders through smartphone technologies to help in determining syncope’s attack patterns. Patient education has been indicated to be a critical aspect in recovery from a myriad of disease conditions, for which syncope is one. Therefore, patient education on salt intake in hypertension and other beneficial information could have been included in the patient s management.
Dual-chamber pacemaker
According to Linde and Crijns (2021), whereas the use of pacemakers has gained much consideration with some strains of faints, cardiac pacing or the use of chamber pacemakers has been discredited in the management of syncope in many patients. The dual-chamber was appropriate for the management of syncope in the elderly patient. According to the current AHA (2016) guidelines on syncope management, the use of pacemaker implantations among older patients is an effective strategy in addressing syncope-related cardiac problems (Barón-Esquivias et al., 2020). Symptoms of a dual-chamber pacemaker include fatigue, dizziness, and chest pains. Upon review of the ‘patient’s history, dizziness was indicated as one of the problems that the patient was experiencing.
Reference List
Aspland, E., Gartner, D. and Harper, P., (2021) ‘Clinical pathway modelling: a literature review’, Health Systems, 10(1), pp.1-23.
Ali, N.J. and Grossman, S.A. (2017) ‘Geriatric syncope and cardiovascular risk in the emergency ‘department’’, The Journal of Emergency Medicine, 52(4), pp. 438-448
Anderson, T.S., Thombley, R., Dudley, R.A. and Lin, G.A. (2018) ‘Trends in hospitalization, readmission, and diagnostic testing of patients presenting to the emergency department with syncope’, Annals of Emergency Medicine, 72(5), pp. 523-532
Barón-Esquivias, G., et al. (2020) ‘Impact of dual-chamber pacing with closed loop stimulation on quality of life in patients with recurrent reflex vasovagal syncope: results of the SPAIN study’, EP Europace, 22(2), pp. 314-319. Web.
Brignole, M., et al. (2018) ‘2018 ESC Guidelines for the diagnosis and management of ‘syncope’, European Heart Journal, 39(21), pp. 1883-1948.
De Ruiter, S.C. et al. (2018) ‘Multiple causes of syncope in the elderly: diagnostic outcomes of a Dutch multidisciplinary syncope ‘pathway’, Ep Europace, 20(5), pp. 867-872.
Doman, E.R., Kisling, A.J. and Fentanes, E., (2021) “Vasovagal Syncope—Reply.” JAMA Internal Medicine (Accessed: 06 April 2021).
Drago, F., et al. (2018) ‘Use of a pediatric syncope unit improves diagnosis and lowers costs: a hospital-based experience’, The Journal of Pediatrics, 201, pp.184-189.
El-Hussein, M.T. and Cuncannon, A. (2021) ‘Syncope in the emergency department: a guide for ‘clinicians’, Journal of Emergency Nursing, 47(2), pp. 342-351.
Gehi, A.K. and Narla, V. (2018) ‘Syncope: Laying the groundwork for a path ‘forward’, JACC Journals, 4(2). (Accessed: 07 April 2021)
Ghariq, M., et al. (2021) ‘Factors facilitating and hindering the implementation of the European Society of Cardiology Syncope Guidelines at the Emergency Department: a nationwide qualitative ‘study’, International Journal of Cardiology.
Goldberger, Z.D., et al. (2019) ‘ACC/AHA/HRS versus ESC Guidelines for the diagnosis and management of syncope: JACC guideline ‘comparison’, Journal of the American College of Cardiology, 74(19), pp. 2410-2423.
Gorlicki, J., et al. (2020) “Patient care pathways in acute heart failure and their impact on in-hospital mortality, a French national prospective survey.” IJC Heart & Vasculature, 26, p.100448. Web.
Kam, K. (2020) Improving Syncope-Related Symptoms in Elderly Cardiology Outpatients by Providing Standardized Printed Patient Education (Doctoral dissertation, University of Hawai’i at Manoa). Web.
Koza, Y., et al. (2017) ‘Syncope in a patient with a dual-chamber pacemaker: what is the possible mechanism?’, Journal of Arrhythmia, 33(3), pp. 240-241. Web.
Kryuchkova, E. A., et al. (2018) ‘Diagnosis and treatment of syncopal ‘conditions’, Summary of Recommendations of European Society of Cardiology.
Linde, C. and Crijns, H.J. (2021) ‘Pacing for repeated vagal reflex-mediated syncope: an old problem with a ‘solution’,’ European Heart Journal, 42(5), pp. 517-519.
Long, B. and Koyfman, A. (2017) ‘Vascular causes of syncope: an emergency medicine ‘review’, The Journal of Emergency Medicine, 53(3), pp.322-332. Web.
McDermott, D. and Quinn, J. (2016) ‘Approach to the adult patient with syncope in the emergency ‘department’, UpToDate, Hockberger S Robert ur. UpToDate [Internet]. Waltham.
Moloney, D., Romero-Ortuno, R. and Kenny, R.A. (2021) ‘Vasovagal ‘Syncope’, JAMA Internal Medicine.
Oberman, R. and Bhardwaj, A. (2020) Physiology, Cardiac. StatPearls [Internet]. Web.
Rana, I.A. and Afzal, W. (2019) ‘Accessory cardiac conduction pathway with an unusual ‘presentation’,’ Journal of the College of Physicians and Surgeons Pakistan, 29(2), pp. S77-S79. Web.
Rogers, J., et al. (2019) ‘Referral pathways in the evaluation of ‘syncope’,’ Circulation: Cardiovascular Quality and Outcomes, 12, pp. A266-A266.
Rotter, T., et al. (2019) ‘Clinical pathways as a quality strategy.’ Improving Healthcare Quality in Europe, p.309. Web.
Sandhu, R.K. and Sheldon, R.S. (2019) ‘Syncope in the emergency ‘department’,’ Frontiers in Cardiovascular Medicine, 6, p.180. Web.
Saurer, G., Mezler-Andelberg, M. and Weihs, W. (2019) ‘P5676 Implementing a syncope ‘pathway’, European Heart Journal, 40, pp. 746-0618.
Shen, W.K. and Sheldon, R.S. (2017) ‘Assessment and treatment of ‘syncope’.’JAMA Cardiology, 2(8), pp. 920-921.
Shen, W.K., et al. (2017) ‘2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm ‘society’, Journal of the American College of Cardiology, 70(5), pp. e39-e110.
Sutton, R. (2017) ‘Should we treat severe vasovagal syncope with a pacemaker?’, Journal of Internal Medicine, 281(6), pp. 554-561. Web.
Sutton, R., Ricci, F. and Fedorowski, A. (2020) ‘Syncope: Today and ‘tomorrow’, Frontiers in Cardiovascular Medicine, 7, p.141. Web.
Wilson, J., et al. (2018) ‘A study in the diagnosis and management of syncope: a retrospective review.’ The British Journal of Cardiology, 25, pp.54-7.
Zimmermann, T., et al. (2021) ‘Development of an electrocardiogram-based risk calculator for a cardiac cause of ‘syncope’, Heart.