Safety Competency of Quality and Safety Education for Nurses
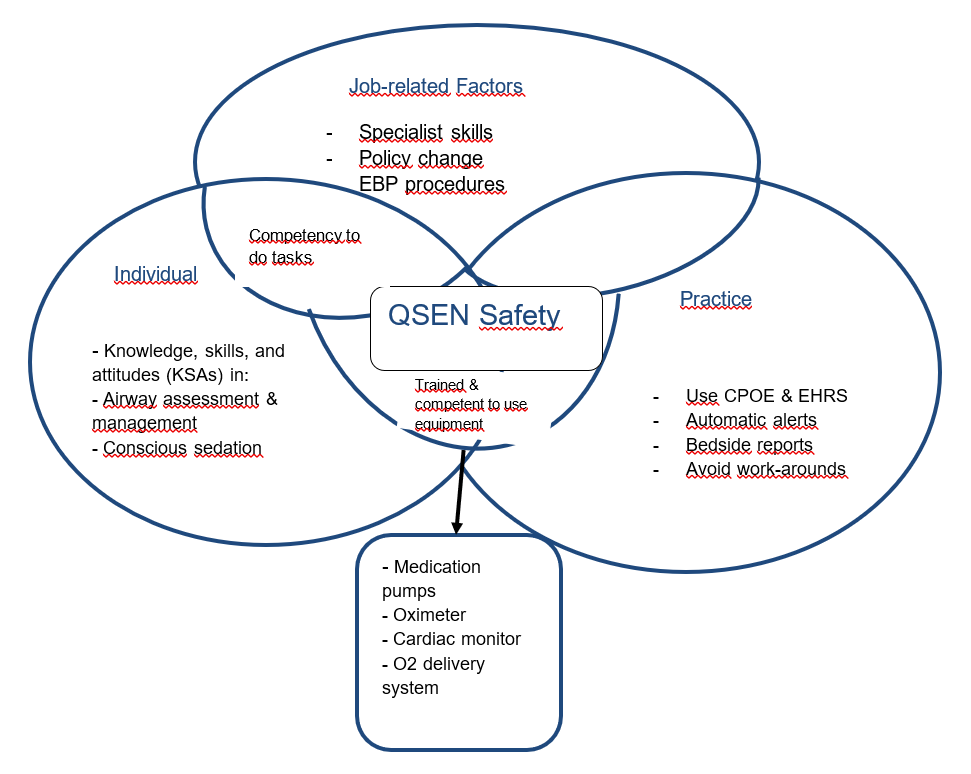
Safety is a core Quality and Safety Education for Nurses (QSEN) competency. As a professional nurse, I regard safe care as one devoid of medical errors or harm to the patient and caregivers. In practice, safety is achieved through nursing process efficiency and improved provider performance (Mansour, 2012). When caring for patients under conscious sedation, which is the focus of my practicum project, adherence to guidelines and routine monitoring would help prevent post-procedure respiratory complications. The key KSA captured in QSEN safety includes the adoption of “national patient safety resources” in nursing practice (Sherwood & Zomorodi, 2014, p. 17). I consider safety to be the utilization of conscious sedation guidelines set out by the ASA and routine monitoring to ensure vital signs are normal. Through hourly rounding, the nurse can monitor the patient’s pain, position, and vitals to prevent respiratory complications while sedated (Lee, Jang, & Park, 2016). One critical aspect of monitoring I consider important is checking the hemodynamic and O2 saturation of a sedated patient. For this reason, nurses should be knowledgeable of airway assessment and management protocols. Further, I regard the knowledge of safety-enhancing technologies, including the O2 delivery system, pulse oximeter, and cardiac monitor, as critical. During sedation, the nurse should have a clear view of the patient’s chest and mouth for a prompt response to any sign of airway obstruction. The QSEN component of safety requires nurses to use standardized practices to advance safety and reduce medical error risk. I consider standardized bedside reporting using whiteboards placed in the patient room as important for effective nursing communication. Standardized notations can be used in the shift-to-shift transfer of information related to the analgesics used, dosage level, and vital signs to promote patient safety.
Safety Promotion in Sedated Patients
Besides the routine assessment of the patient’s respiratory response and vitals, effective monitoring of sedation efficacy is an important nursing skill. According to Tobias and Leder (2011), the depth of conscious sedation can affect patient safety and comfort during radiological procedures. Pain assessment during interventional radiology can indicate the responsiveness of the sedated patient. Therefore, as a nurse, I consider the utilization of pain scoring systems an important KSA for assessing the safety of patient sedation. For patients undergoing radiological procedures, the main threat to patient safety is over-sedation, which results in repressed responsiveness (Tella et al., 2014). Sedated patients are not expected to lose complete pain sensation. Therefore, evaluating the level of pain through verbal stimuli or the use of the bispectral index (BIS) would indicate the depth of sedation. Also, the risk of adverse respiratory events is high in over-sedation cases. Taylor et al. (2011) found a correlation between airway issues and deep sedation monitored with the BIS. Further, O2 desaturation was more frequent in deeply sedated patients than in those who remain awake during radiological procedures. Therefore, as a nurse, knowledge of pain assessment is critical in promoting the safety of sedated patients during and after procedures.
Mind-map
References
Lee, N., Jang, H., & Park, S. (2016). Patient safety education and baccalaureate nursing students’ patient safety competency: A cross-sectional study. Nursing and Health Sciences, 18, 163–171.
Mansour, M. (2012). Current assessment of patient safety education. British Journal of Nursing, 21, 536–543.
Sherwood, G., & Zomorodi, M. (2014). A new mindset for quality and safety: The QSEN competencies redefine nurses’ roles in practice. Nephrology Nursing Journal, 41(2), 15–22.
Taylor, D., Bell, A., Holdgate, A., MacBean, C., Huynh, T., Thom, O.,…Pasco, J. (2011).
Risk factors for sedation-related events during procedural sedation in the emergency department. Emergency Medicine Australasia, 23, 466–73.
Tella, S., Liukka, M., Jamookeeah, D., Smith, N., Partanen, P., & Turunen, H. (2014).
What do nursing students learn about patient safety? An integrative literature review. Journal of Nursing Education, 53, 1–7.
Tobias, J., & Leder, M. (2011). Procedural sedation: A review of sedative agents, monitoring, and management of complications. Saudi Journal of Anaesthesia, 5(1), 395–410.