Comprehensive History
Identifying Data: Ms. J. A.; 27 years old.
Chief complaint: “Debilitating fatigue accompanied by shortness of breath, dizziness, and chest pain. Cannot spend too much time on my feet because I get lightheaded. Dizziness can get worse because of sudden physical activity such as standing up too quickly or having to go up the stairs. During periods, symptoms become even more pronounced. Recently, I have been getting extremely dark under-eye circles despite sleeping nine to ten hours a day.”
History of Present Illness
O (onset): have constantly been feeling tired for the last five months.
L (location): head and chest.
D (duration): every two to three days, sometimes the fatigue is worse than usual.
C (characteristics): weakness does not allow focusing, working, or even staying active.
A (aggravating factors): physical activity, periods, long times without food.
R (relieving factors): high in nutrients food can help, especially fruit such as oranges.
T (treatment): no treatment has been implemented.
Medications: vitamin C supplements and occasional aspirin.
Allergies: no allergies reported.
Past Medical History
Ms. J. A. has been seeing her gynecologist regularly due to severe cramping during periods as well as heavy bleeding. Have been prescribed aspirin and hormonal contraceptives to regulate her cycle. The patient stopped taking contraceptives six months ago due to sight effects such as weight gain, mood swings, and migraines, which are very common (Smith, 2018).
Past Surgical History
Ms. J. A. has not been subjected to any surgeries.
Family History
It is expected that the review of the patient’s family history will reveal more information regarding her likely diagnosis since some health conditions are usually inherited from family members (Cirino & Ho, 2013).
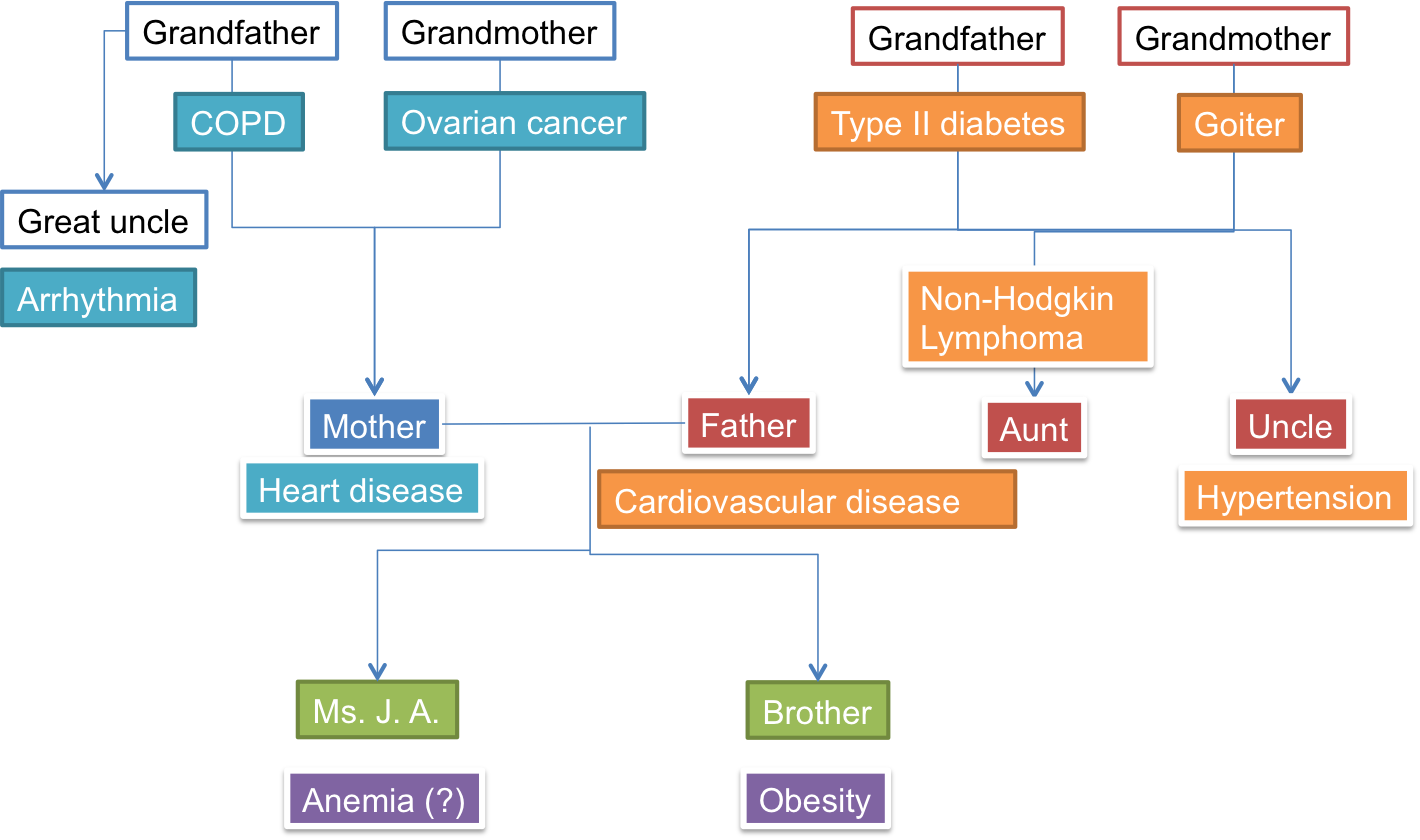
As seen by Ms. J. A.’s family history, there is an evident trace of complex heart conditions that affected her relatives. Since the patient’s grandfather passed away at from heart disease, her mother has been diagnosed with this condition, and her father also has the same diagnosis, it is essential to recommend to Ms. J. A. to take cardiovascular health seriously. There are some serious health problems in the patient’s grandmother and aunt since both of them were diagnosed with cancer, so it is recommended for Ms. J. A. to get regular check-ups, especially with regards to reproductive health and the proper functioning of lymph nodes. The entire family history shows that the patient should not delay further screening and diagnosis that can reveal conditions that might be inherited.
Social History
The patient is twenty-seven years old, single, and does not have children. She rents an apartment by herself and is currently saving money to buy a small house. The patient works in the sphere of online advertising. Ms. J. A. does not have to go to the office, so she works predominantly from home. Her family lives in another state so that the patient cannot see them regularly. However, her younger brother has moved to her town, which made Ms. J. A. very happy. Recently, the patient lost her grandfather to a heart attack; the stress associated with the loss contributed to her deteriorating wellbeing. Also, the patient has been experiencing extreme pressure at work because of a large project with an important client, but her fatigue prevented her from committing to the project 100%.
Sexual and Reproductive History
The patient is aware of her issues with reproductive health and is on the continuous monitor by her doctor. She reported having one pregnancy at twenty-three, which ended in a miscarriage.
Health Care Maintenance (HCM) Strategies
Ms. J. A. reported that the maintenance of health care was hard for her due to stress and fatigue that prevents her from being active. Every six months, she visits a dentist to maintain oral health and takes a blood test to monitor her hormone levels (progesterone, estrogen, testosterone).
Review of Systems
The review of the patient’s systems shows that some of them function properly while others don’t. The physical assessment gives and an indication that Ms. J. A. may suffer from anemia, which is a condition characterized by a low number of blood cells that gets worse during such circumstances as periods (blood loss) and physical activity (stress for the body) (Mayo Clinic Staff, 2017). It is important to discover the reason for the patient’s possible anemia (e.g., iron deficiency, vitamin deficiency, chronic conditions, etc.). Also, the review of the patient’s family health history pointed to the need for Ms. J. A. to pay more attention to cardiovascular and reproductive health since these two issues were very prominent in her genogram.
Complete Physical Examination
Vital Signs
Temperature: 95 F (35.8 C).
Pulse: 78 beats per minute.
Respiration and Blood Pressure: 90/60 (low blood pressure); 15 respirations per minute (lower than the norm)
Weight and Height: 165 cm; 130 lbs (59 kg).
Body Mass Index (BMI): 21.67 kg/m2 (normal).
Mental Status Exam
The patient appears to be slightly disheveled; despite wearing neat clothes, she is not wearing makeup and appears to have not washed her hair for a couple of days. She is slightly disoriented in the surroundings and cannot be particularly articulate when expressing her thoughts.
There are no signs to show that the patient could have any serious behavioral issues. She admits to being extremely concerned with her condition and regrets not contacting a health provider earlier.
Ms. J. A. seems nervous and lacks focus, probably because of the constant stress and fatigue. Nevertheless, her thought-response coordination is on a normal level, which means that the patient thinks logically and provides appropriate answers to questions.
No evident cognitive dysfunctions have been found during the examination; however, the patient took some time before responding to questions. However, no issues with encoding or decoding of relevant messages have been discovered.
Ms. J. A.’s examination revealed no significant complications with her state of mind; despite the slow reactions, her articulation can be considered normal. All signs revealed during the assessment showed that the patient’s severe stress and tiredness contributed to the decreased well-being and the possible diagnosis of anemia, which is also characterized by mental complications (e.g., confusion, feeling unsure or indecisive, mild anxiety or depression) apart from physical characteristics.
Physical Examination
Skin: J. A. has pale skin, with severe under-eye circles, which makes her appear tired and lackluster. The skin’s texture is within the normal range and gives an appropriate response to touch. The surface of the skin is cool and slightly dehydrated on the arms and legs; the patient’s skin on the face is dry and flaky on the cheeks. The patient’s nails do not appear to be in a normal condition; the surface is irregular, with some nails peeling and flaking. J. A. has medium-length hair of thin appearance; there are some signs of dandruff due to dry scalp skin.
Head: the patient’s head is of symmetrical shape, with no visible signs of any injuries. Also, the patient’s lymph nodes located in the head are of the normal range and do not appear to be tender.
Eyes: the patient’s pupils dilate and constrict as normal; blinking motions appear to be within the normal range. Visual acuity is lower than normal, possibly due to Ms. J. A.’s exhaustion.
Ears: earlobes are proportionate without any visible deformities; ear canals are clear, EOM intact.
Nose and Sinuses: normal, non-inflamed mucosa, no external lesions that are visible, no septum issues.
Mouth and Throat: the patient shows not to have any mucosal lesions; the mucous membrane is moist and within normal characteristics.
Neck: the patient’s thyroid gland is of a normal range, not tender; the neck is supple with no adenopathy; submandibular lymph nodes are non-tender.
Respiratory: non-tender paratracheal lymph nodes; the lungs are clear.
Cardiovascular and Peripheral Vascular: occasional cardiovascular murmur, gallops, regular but slow heart rhythm.
Abdomen: no irregular bowel sounds, no tenderness, and masses; both superior mesenteric and celiac lymph nodes are not inflamed.
Musculoskeletal: no restricted range of motion, visible tiredness in hands and legs; the examination revealed no evident atrophy in the extremities, spine, and neck. The patient shows no defects and masses in the musculoskeletal system.
Neurological: decreased sensation to touch and pain. The patient is disorientated; her speech is slow; although, comprehension, naming, and recognition are within the normal range. CN II: the patient’s visual fields are full of confrontation; the fundoscopic exam showed normal results (disks are sharp). The patient’s pupils are normal (3,5 mm) and react to light briskly. CN III-VI are within normal range: the facial sensation is intact.
References
Cirino, A. L., & Ho, C. Y. (2013). Genetic testing for inherited heart disease. Circulation, 128(1), 4-8.
Mayo Clinic Staff. (2017). Anemia. Web.
Smith, L. (2018). 10 most common birth control pill side effects. Medical News Today. Web.