Introduction
A comprehensive history and physical examination is a tool developed by and for health care providers for an integrated and evidence-based approach towards evaluating a patient’s health and determining what factors contribute to his or her condition (Benner, Hughes, & Sutphen, 2008). This paper will include a comprehensive history and physical examination of a patient that referred to the healthcare provider with a complaint of severe pain in the chest; the patient has been previously diagnosed with co-morbidities such as hypothyroidism and type 2 diabetes.
Comprehensive History
Identifying Data: Mrs. J.K., forty-five years old, female.
Chief complaint: “Severe chest pain and discomfort accompanied by the weakness in legs and arms that have been taking place for around four months on and off. I am sure that chest pain happens because of stress at work and family problems. The visit to the doctor has been placed on the back burner since I lack time to take care of myself.”
History of Present Illness
Since there is a complaint of acute pain in the chest, the OLD CART characteristics of the reported condition apply:
- O (onset): pain started occurring four months ago.
- L (location): mostly in the chest area, with accompanying numbness in arms and legs.
- D (duration): every three-four days, with the chest pain lasting for around two hours at different times during the night and day.
- C (characteristics): the pain is debilitating, which causes the patient to get dizzy or even faint in the most severe instances.
- An (aggravating factors): the chest pain is worse when the patient is active (at work or doing errands); if the patient experiences too much stress, the pain exasperates.
- R (relieving factors): the pain relieves when the patient lies down to rest and takes aspirin.
- T (treatment): nitroglycerin and aspirin to ease the pain.
Medications: occasionally took aspirin and nitroglycerin to relieve the pain; takes Armour thyroid for controlling her hormone levels.
Allergies: allergic rhinitis and dust allergy.
Past Medical History
According to Bickley (2012), the technique of history taking is one of the essential skills a nurse practitioner (and any other health provider) should master for providing effective patient care.
Mrs. J.K. is forty-five years old; she visited her physician six months ago with less severe chest pain and was prescribed nitroglycerine to relax heart arteries and allow blood to move quickly through the narrowed spaces (Mayo Clinic Staff, 2014). Mrs. J.K. stated that since that time her health has taken a turn for the worse, but she associated it with increased stress at work and the intense psychologic distress from the loss of her sister.
Currently, chest pain and occasional numbness in arms and legs are her primary health complaints. Previously, Mrs. J.K. has been diagnosed with type 2 diabetes and genetic hypothyroidism (thyroid excess), which she inherited from her mother. The patient does not report dehydration, fever, or skin rashes. However, she reported increased fatigue and blurred vision, which are also a symptom of type 2 diabetes (Wells, 2016).
Her weight has been unstable for the past six months due to mental stress: she has gained ten pounds because of overeating and not doing any physical activities. The patient stated that it was very easy for her to gain weight but losing it (even with a healthy diet and exercising) was much harder due to her thyroid problems and hormonal imbalances, which are linked to the co-morbidities of type 2 diabetes and hypothyroidism.
Past Surgical History: surgical removal of the appendix (appendectomy).
Family History
Analyzing a patient’s family history is an essential step in evidence-based screenings since it will allow the health provider to pose clinical questions that focus on the patient’s problem specifically (Dains, Baumann, & Scheibel, 2015) and determine whether the possible diagnosis was present in the immediate family.
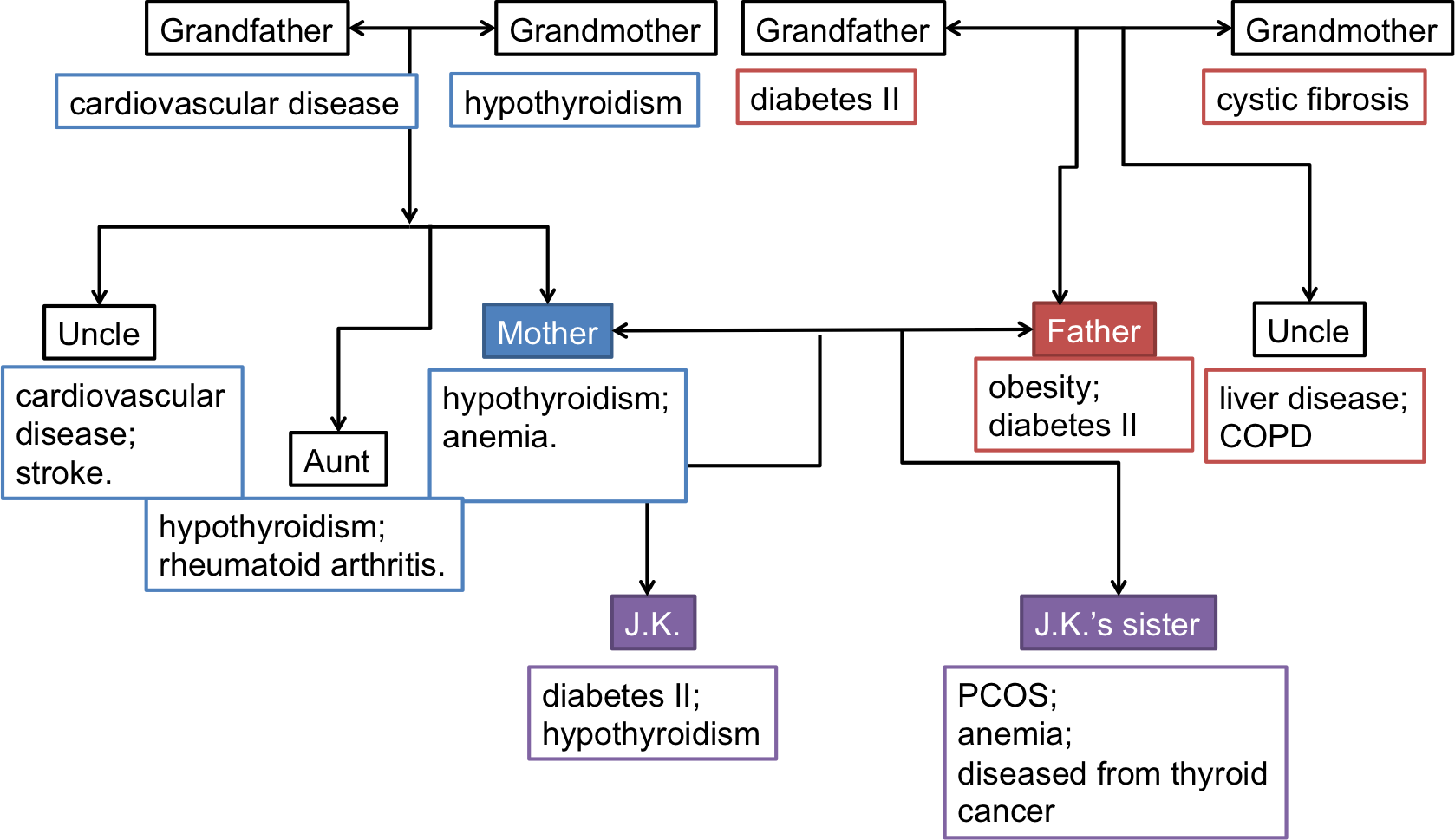
As seen from the genogram of the patient’s family history presented above, hypothyroidism and type 2 diabetes are inherited conditions; while type 2 diabetes was inherited from J.K.’s father’s side, problems with the thyroid were first detected in the patient’s grandmother. Mrs. J.K.’s grandfather on the mother’s side passed away from cardiovascular disease while from the father’s side, the grandfather passed away from type 2 diabetes.
Therefore, the fact that Mrs. J.K. has been previously diagnosed with diabetes is not surprising; she is also at risk of developing serious cardiovascular problems since her family history shows a prevalence in occurrence. It is important to mention that only the female side of the patients’ family suffered from hypothyroidism, which is a typical situation in many cases of inherited health conditions. According to Zaletel and Gaberscek (2011), family studies have confirmed a high genetic susceptibility to the disease. It is expected that Mrs. J.K.’s daughter also inherits thyroid problems; it is recommended to monitor the development of the organ from the earliest stages.
Social History
Mrs. J.K. is married and has been living with her husband for fifteen years; they have a twelve-year-old daughter. Currently, Mrs. J.K. works as a business law consultant for different clients (predominantly from her home office). The patient reported living in a family-friendly neighborhood and having a lot of acquaintances, which points to the fact that her social life is well-developed. Mrs. J.K. has recently lost her older sister to thyroid cancer, which affected the patient drastically and hurt both her mental and physical wellness.
The patient has not visited a therapist to deal with her grief due to the increased stress at work: her largest client has been going through a lawsuit so the majority of her time Mrs. J.K. currently spends working. She does not have much time for her family.
Sexual and Reproductive History
The patient reported having two pregnancies: one failed (at an early stage) and one was successful, she gave birth to her daughter when she was thirty-three years old. The sexual and reproductive history of the patient can be considered widespread for a woman of her age, no health problems such as PCOS or STDs have been diagnosed.
Health Care Maintenance (HCM) Strategies
Mrs. J.K. does not spend much time on her health maintenance due to the recent developments at work and in her personal life; she has not visited her dentist for a year. She visits her endocrinologist every six months and takes blood tests (T4, T3, and TSH) to monitor the function of her thyroid. Regarding hormones’ maintenance, Mrs. J.K. has been taking Armour thyroid for seven years after being diagnosed with thyroid disease.
Physical Examination
Review of Systems
- General: recent weight gain (10 pounds); no fever or chills.
- Vision: no significant visual changes; tiredness in eyes after working late behind the computer.
- Ears, nose, and throat: no hearing loss; dryness in the throat.
- Cardiovascular: recurring chest pains and pressure on the chest; arrhythmia; occasional shortness of breath; no cramping in thighs or varicose veins; peripheral edema.
- Respiratory: occasional shortness of breath; no cough or wheezing.
- Gastrointestinal: no abdominal pain or heartburn; regular stool.
- Genitourinary: no frequent urination or urgencies.
- Musculoskeletal: no pain in joints, no swelling; no musculoskeletal pain; no restricted motion.
- Skin: no rashes, sores, or blisters; no growth.
- Neurological: numbness in extremities (arms and legs); occasional loss of sensation; no burning.
- Psychiatric: depression, anxiety, and nervousness.
- Endocrine: occasional excessive thirst; no intolerance to heat or cold.
- Lymphatic: no abnormal bleeding.
- Immune: allergic reactions to dust; no recurrent infections.
Complete Physical Examination
Vital signs:
- Temperature: 97.8 F (36.5 C).
- Pulse: 105 beats a minute (higher than the norm) (Laskowski, 2015).
- Respiration and Blood Pressure: 170/90: high blood pressure; 26 respirations a minute (higher than the norm).
- Weight and Height: 170 cm; 170 lbs (77 kg).
- Body Mass Index (BMI): 26.6 (overweight).
General Survey
A general survey refers to the overall review of the first impressions a healthcare provider has of the well-being of the patient (Jarvis, 2012).
As seen from the analysis of Mrs. J.K.’s appearance, behavior, and mobility, she has made the first impression of a well-groomed woman that exhibits signs of psychological distress and disorientation. The mental status exam will allow the health provider to determine the reasons for her behavior and identify any underlying issues that should be addressed in the subsequent treatment.
Mental Status Exam (MSE) in Narrative Form
Mrs. J.K. is a neatly dressed woman with dark blonde hair; she is wearing all black as a gesture of grief and respect for her late sister. Her behavior is subtle and quiet, bordering on exhausted; she was encouraged to speak louder when answering questions of the nurse practitioner. Her language is clear; however, the tone of her voice indicated sadness and frustration with the health situation.
Mrs. J’s mood can be characterized as melancholic and pessimistic, when answering questions about the latest health developments, she used phrases such as “nothing will get better,” “I feel worse each time the pain occurs,” “I have no power to deal with this,” or “I don’t care.” It is evident that the patient is exhausted and deals with too many problems at the same time, which contributes to the decrease of her self-efficacy and the desire to deal with the recurring health issue.
The patient’s thought processes are currently occupied with her concerns about the upcoming trial of her largest client, the loss of her sister, and the frequent occurrence of chest pains. It seems that Mrs. J does not have enough helpful resources to manage her situation; therefore, she chooses to ignore the severe pain and continue working to occupy herself with important tasks. Unfortunately, the patient has put her health on the back burner for so much time; now the impact of her condition will be even more noticeable.
It cannot be concluded that the patient’s cognitive function is impaired; however, it is significantly affected by her grief and complications at work. Mrs. J perceives her situation as highly depressing, but she reasons that the stress causes her to have chest pain, not a serious health problem that could have been inherited (refer to the genogram section of the paper). While stress is a highly likely contributor to Mrs. J’s condition, she lacks the clarity of thought regarding her subsequent treatment and the necessity to “lay off” her work and start paying more attention to her physical and mental well-being.
Determining the patient’s judgment refers to the assessment of problem-solving skills. Mrs. J.K.’s judgment has been undermined by her family and work-related problems; however, she made the right decision to visit a healthcare provider since her condition was getting worse with each occurrence of the pain. As to her insight into the problem, some issues can be identified. For example, the patient does not understand that her condition can be extremely complex and that she might need serious treatment.
Physical Assessment
Skin: no rash, good turgor, no prominent lesions or unusual bruises; the hair of firm texture and distribution; nails of standard color without deformities.
Head: normocephalic and atraumatic; no palpable or visible scarring; no swelling in the lymph (submental, parotid, occipital, and cervical) nodes;
Eyes: Intact visual acuity ad clear conjunctive; non-icteric clear, EOM intact.
Ears: Clear EACS, intact hearing, translucent, and mobile TMs.
Nose and Sinuses: no visible external lesions, non-inflamed mucosa, no deformities in the septum.
Mouth and Throat: no visible mucosal lesions; moist mucous membrane.
Neck: the neck is supple; no bruits or adenopathy; enlarged thyroid, tender; neck lymph nodes (submandibular) slightly tender.
Respiratory nodes: clear lungs to percussion and auscultation; lymph nodes (paratracheal) non-tender.
Cardiovascular and Peripheral Vascular: no cardiomegaly; irregular rhythm and heartbeat; occasional gallops and murmur.
Abdomen: no strange sounding in the bowels, no hernia or tenderness, no masses or organomegaly; no inflammation in the lymph (celiac and superior mesenteric) nodes.
Musculoskeletal: slightly decreased range of motion and instability; no defects, masses, or tenderness; no atrophy in the neck, head, spine, or extremities.
Neurological: irregular (increased) sensation to pain and touch; no pathologic reflexes detected; average DTRs; CN 2-12 irregular.
Recommendations
While the comprehensive history and physical examination assignment do not include the diagnosis, it is recommended that the patient refers to her cardiologist for a full assessment of the cardiovascular health due to the reports of recurring chest pain and the diagnosis of the cardiovascular disease that runs in her family. Blood tests, ECG, chest x-ray, and chest Ct scan are advised for diagnosing the patient’s condition and determining the appropriate treatment options (Fischbach & Dunning, 2014).
Most importantly, Mrs. J.K. showed indications of severe psychological distress associated with increased pressure at work and the loss of her sister. It is highly recommended for the patient to visit a mental health professional to manage her condition. Mrs. J.K. should understand that taking care of both her mental and physical health.
References
Benner, P., Hughes, R., & Sutphen, M. (2008). Clinical reasoning, decisionmaking, and action: Thinking critically and clinically. In R. Hughes (Ed.), Patient safety and quality: An evidence-based handbook for nurses (pp. 1-23). Rockville, MD: Agency for Healthcare Research and Quality.
Bickley, L. (2012). Bates’ guide to physical examination and history-taking (11th ed.). New York, NY: Wolters Kluwer.
Dains, J., Baumann, L., & Scheibel, P. (2015). Advanced health assessment & clinical diagnosis in primary care (5th ed.). Louis, MO: Elsevier.
Fischbach, F., & Dunning, M. (2014). A manual of laboratory and diagnostic tests (9th ed.). New York, NY: Wolters Kluwer.
Jarvis, C. (2012). Physical examination & health assessment (6th ed.). Louis, MO: Elsevier.
Laskowski, E. (2015). What’s a normal resting heart rate? Web.
Mayo Clinic Staff. (2014). Treatments and drugs. Web.
Wells, D. (2016). Recognizing type 2 diabetes symptoms. Web.
Zaletel, K., & Gaberscek, S. (2011). Hashimoto’s thyroiditis: From genes to the disease. Current Genomics, 12(8), 576-588.