Comprehensive History
Identifying Data
A.L.
Chief Complaint
“I have recently fallen from my bike and hit my head. I was wearing a helmet, but I still have headaches and cannot fall asleep for a long time when going to bed.”
History of Present Illness
The patient has a complaint of persistent headaches, which started to occur after he fell from his bicycle. He fell and hit his head two weeks ago, and the pains began appearing a day after the accident. Thus, he has been having headaches for approximately two weeks. Moreover, the patient states that he cannot fall asleep due to headaches and struggles to get enough sleep to function properly. The headaches can occur during the day and get worse in the evening, as the patient works with computers and often strains his eyes, which is an aggravating factor. He does not mention any other possible symptoms. Relieving factors: A.L. has limited his time working with the computer and stopped biking for some time. He drinks green and chamomile tea as a natural remedy. He takes over-the-counter pain relievers when the headaches are disturbing his sleep.
Medications
The patient uses pain-relieving medications to deal with headaches and falls asleep. Otherwise, he does not mention any other prescribed or over-the-counter medications.
Allergies
The patient has a mild form of allergy to seafood. He does not report having any medicine-related allergic reactions.
Past Medical History
Two years ago, the patient fell off his bicycle during a biking trip and strained his arm muscles as a result. He also had some accident-related neck injuries and was hospitalized to eliminate the possibility of a concussion. A.L. was treated for the injuries and underwent physiotherapy for his arm. Physiotherapy lasted for three months, during which he seemed to recover all of his strength and agility.
Past Surgical History
The patient has no history of major or minor surgeries.
Family History
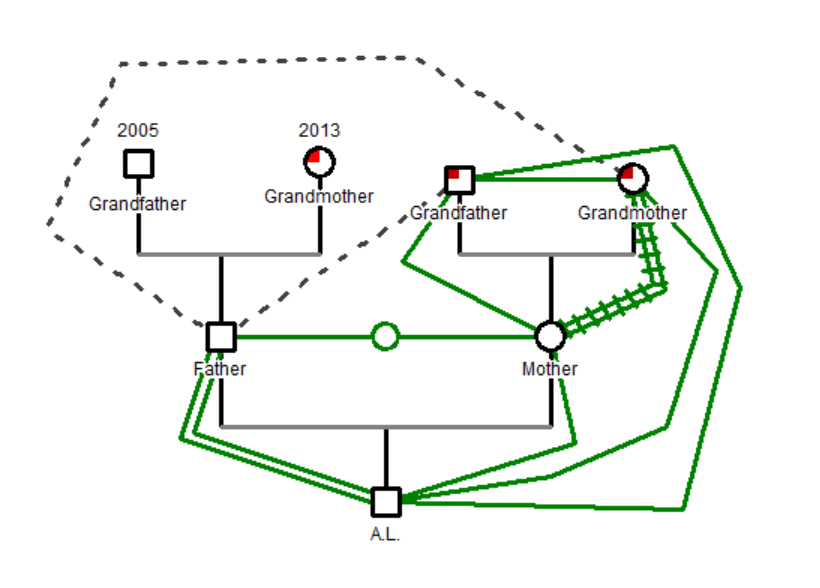
The patient’s great-grandparents’ health history is not recorded anywhere. As can be seen in Figure 1, A.L.’s grandparents from the father’s side passed several years ago. His grandmother passed away due to complications from a heart attack at the age of 84, and the grandfather died in a car crash. Both grandparents did not have any hereditary conditions. A.L.’s grandparents from the mother’s side are still alive, both having hypertension and mobility problems due to old age. The patient’s parents are alive. The mother is a medical worker with no apparent medical issues apart from fatigue due to a busy work schedule. The father is a former construction worker with occupation-related allergies – he recently developed an allergic reaction to dust and had to leave his workplace. Currently, he is working with his son in the business of selling sporting goods.
Social History
The patient likes biking and often goes on biking and hiking trips with his friends. He leads a healthy lifestyle, abstaining from drinking alcohol. A.L. does not smoke or use any illicit substances. He works as a small online retailer, selling bicycles and hiking equipment. Apart from his active hobbies, he also likes to travel. A.L. lives alone in an apartment in the city.
Sexual and Reproductive History
The patient is heterosexual. He is currently single, his last long relationship ended two months ago, and he did not meet anyone else during this period. He has no children.
Health Care Maintenance (HCM) Strategies
The patient is interested in maintaining his health. He often visits doctors for regular check-ups, including dental care. Moreover, he frequently visits physiotherapists and massage therapists to check the condition of his muscles.
Review of Systems
The patient’s systems seem to be in great condition. There are no obvious reasons for the patient to have headaches. The physical assessment reveals no problems with the patient’s functioning.
Complete Physical Examination
Vital Signs
- Weight: 142 lbs.
- Height: 5’8”
- BMI: 21.6
- Temp.: 97.9 F
- Pulse: 62
- BP: 117/73
- Respiration: 12
Mental Status Exam (MSE)
The patient appears well-nourished and groomed. A.L. is dressed in clean clothes; his hair is well-kept. However, he seems to be somewhat tired. His behavior is not erratic, and he seems to be fully aware of his surroundings. He answers questions with limited articulation but in a logical and coherent way. His language is consistent, and he communicates without any complications.
The patient is concerned about his headaches and wants to receive treatment. Although he appears tired, he does not have any serious behavioral issues. His mood is stable, and he does not express any dissatisfaction in an aggressive or distraught way.
The patient has no problem explaining his situation and states that he is not experiencing any acute pains during the examination. Perhaps, his stable condition allows him to formulate his thoughts clearly. The patient’s thought process seems to be logical, as he answers questions and provides only necessary and relevant information.
A.L.’s responses are rather quick, but he takes time to think over his answers and recall past events. He is aware of his actions and words and also knows about the dangers connected to his active hobbies. His interaction with the environment does not reveal any cognitive issues.
The MSE does not reveal any problems with the patient’s mental state (Matuszak, McVige, McPherson, Willer, & Leddy, 2016). He does not appear to have any issues with his thought process, communication, reaction time, and actions. While he does not have a headache at this present moment, his mental state may be stable at other times a well.
Skin
The patient’s skin is pink, warm, and soft to touch. The patient has tanned zones on his face, neck, legs, and lower arms as a result of frequent outdoor activities. There are no sunburns in these areas. The rest of the skin is paler in tone. The surface of the skin is smooth and dry, especially in the elbow area. The patient’s nails are pink and have no deformations or colored spots. A.L.’s hair is thick, dark, short, and curly. It appears to be healthy and well-nourished, with no visible issues or infestations. All of the signs indicate that the patient’s skin, hair, and nails are healthy (Jarvis, 2015).
Head
The head is symmetrical without any apparent injuries. The trauma that the patient had two weeks ago is not present; there are no spots or deformations. The posterior auricular and occipital lymph nodes seem normal to palpation (Jarvis, 2015).
Eyes
The patient’s vision is acute. The eyes have white sclera. The pupillary light reflex of the patient is fast. The patient blinks to light and responds to motion. The cranial nerves (CN) II are normal. The pupils constrict to light and dilate appropriately. Eye movements are proportional to any activities, The CN III-IV and VI are checked. Eye closure is standard; the CN VII is intact.
Ears
The ears are symmetrical, their canals are clear. The hearing function is normal, the CN VIII is intact, and the patient has passed the Whispered Voice Test (Jarvis, 2015).
Nose and Sinuses
The nose has a normal color and asymmetrical shape. The sinuses are clear, and the palpation does not reveal any obstruction or aching sensation.
Mouth and Throat
The patient’s mouth is symmetrical. The lips are somewhat dry; the tongue is pink, does not have any injuries, and has a rough texture. The smell is normal. The CN IX and X are intact because the patient has passed the Motor Function Test (Jarvis, 2015).
Neck
The patient is able to move his head with no problems; there are no muscle pains during movement. The posterior cervical and superficial cervical lymph nodes are normal to palpation (Jarvis, 2015).
Respiratory
The patient’s breathing is regular and effortless. There are no obstructions in the respiration. The supraclavicular lymph nodes are normal.
Cardiovascular and Peripheral Vascular
The pulse rate is near the lower limit of the normal range, which can be explained by the fact that the patient is a physically active man and a semi-professional athlete. The patient’s BP seems normal, although he has a family history of hypertension. The pressure measurement reveals no problems with BP.
Abdomen
The abdomen is soft, non-tender. Normal bowel sounds are present in all four quadrants to auscultation. Lumbar lymph nodes are normal (Jarvis, 2015).
Musculoskeletal
The patient’s muscle movement is normal, although one arm is not as flexible due to the previous injury. Neck movements are normal, indicating no injuries from former accidents. There is no discomfort in moving arms and legs. Crossed-arm adduction and resisted arm extension reveal no significant differences and cause no pain (Malanga & Mautner, 2016).
Neurological
The patient’s reactions are of normal speed. The mental functioning is stable, and the patient is fully aware of the situation and his surroundings. The CN I-XII are intact (Jarvis, 2015). The patient’s neurological system has no problems.
References
Jarvis, C. (2015). Physical examination and health assessment (7th ed.). Philadelphia, PA: Elsevier Health Sciences.
Malanga, G. A., & Mautner, K. (2016). Musculoskeletal physical examination: An evidence-based approach (2nd ed.). Philadelphia, PA: Elsevier Health Sciences.
Matuszak, J. M., McVige, J., McPherson, J., Willer, B., & Leddy, J. (2016). A practical concussion physical examination toolbox: Evidence-based physical examination for concussion. Sports Health, 8(3), 260-269.