What is postoperative fever?
It is temperature rise above the normal temperature (38 C) on two consecutive days after the surgery. The systematic approach and differential diagnosis help institute proper management and narrowing down differential analysis.
Possible causes of Postoperative Fever
Also known as Rule of W, they include:
- Wound Infection
- Venous thromboembolism (Walking)
- Urinary tract infection (Water)
- Drug fever (Wonder drug)
- Atelectasis (Wind)
Take Action
- Know who to call when you get fever
- Follow instructions carefully regarding medication and changing bandages
- Wash hand with warm water and soap before touching the incision
Postoperative fever Criteria
- Temperature less than 36 C or more than 38 C
- Heat beat rate higher than 90BPM
- Respiratory rate higher than 21 per minute
- White blood cells less than 4 x 10/L or more than 12 x 10lL
Types of postoperative fever
- Immediate Fever: occurs mostly between 0 to 1 day after surgery, or hours within postoperative days (POD).
- Acute Fever: it occurs between 1 to 7 PODs
- Subacute Fever: occurs between one to seven weeks
- Delayed Fever: occurs more than four weeks
Clinical Governance
NHS introduced six pillars of governance to support and help healthcare practitioners offer high-quality and safe care to patients.
Also, the six pillars of clinical governance were introduced to create suitable perioperative environment.
Six pillars of clinical governance include:
- Clinical audit
- Education and training
- Risk Management
- Openness
- Clinical effectiveness
- Information management
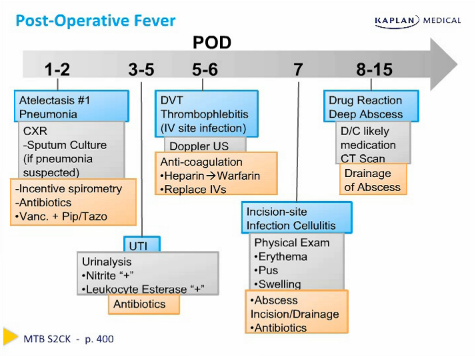
Risk Assessment/ Diagnostic
- Careful physical examination, particularly on possible sources of infections
- Diagnosis to be performed on time onset and clinical presentation
- Assessment of Blood cultures, Chest X-rays, and wound cultures, and urine culture to check nosocomial infections presence if suspected.
- Monitoring vital signs
- Check patient’s notes on intraoperative complications, patient comorbidities, anesthesia, and timing of procedure
- Perform leg’s venous doppler to eliminate deep vein
- An ultrasound assessment DVT
The format of the learning resources used in this essay to raise awareness of risks related to a patient developing fever after surgery is the poster. This paper will elaborate on the role of clinical governance and risk management strategies, the ways to minimize the risks, and why the above poster was used to address postoperative fever. The local Healthcare Trust Policy (2019) clearly states that all medical practitioners should ensure that patients receive the necessary physical assessment after surgery to check temperature rise and symptoms or signs of other postoperative complications. This is because healthcare practitioners can support patients recovering from surgery and post-surgery complications.
For the prevention, management, and treatment of postoperative fever effectively, patients and medical experts such as nurses and physicians have to play their part. According to Abdelmaseeh (2020), several data from different surgical procedures show that 20% to 90% of patients suffer from postoperative fever. Postoperative fever is associated with an increase in the length of stay, mortality, and hospital costs (Field et al., 2019). In other words, postoperative fever increases the treatment costs. Further, Field et al. (2019) also stated that the types of operative fever mainly depend on the surgical procedures; thus, medical practitioners must perform the physical medical examination. As patients continue to undergo surgery, physicians and nurses should advise patients to use incentive spirometry, which effectively prevents atelectasis.
As one of the postoperative complications, postoperative fever occurs in all surgical floors. However, on all surgical floors, the fever is usually controlled by a team of different medical professionals (Maday et al., 2016). Nurses are usually the first people to discover the fever because they monitor patients’ temperature most of the time. After the surgery, the majority of the patients are immobile, and they cannot distinguish the type of fever they are having; some even fail to realize that they have high-temperature rise due to postoperative pain. For this reason, patients depend on perioperative nurses and other medical practitioners to act as their advocates. Actually, this is why Risk Management (RM) exists to help patients receive quality care and prevent postoperative complications. According to Wakefield (2018), it is a systematic process that reduces or prevents potential risks. Most hospitals tend to avoid risks, and healthcare practitioners tend to do their best to minimize the damage when the risks occur.
Additionally, Risk Management can also be regarded as a framework that helps NHS organizations be responsible, maintain high standards of care, and improve the quality of services, primarily by creating a suitable clinical care environment (Price et al., 2020). Moreover, Price et al. (2020) stated that risk management comprises clinical governance aspects, such as risk reporting, audit, risk assessment, guidelines, and training. For the successful execution of risk management, five steps must be followed strictly. These steps include locating the hazard, finding the appropriate approach of conducting consultation with the staff, and locate controls that are in place and those are needed. Lastly, the risk assessment must be reviewed and updated where necessary.
According to Veenstra et al. (2017), clinical governance is a systematic approach that improves and maintains patient care quality within the National Health Services (NHS). Pillars of clinical governance help medical practitioners to identify, report, audit, assess, and prevent the risk. The pillars of clinical governance ensure that staff receives appropriate medical training (Veenstra et al., 2017). However, for clinical governance to be effective, especially in cases that involve postoperative fever, different medical professionals and patients will have to work together. Willingness to work together will help both parties to learn and reflect on errors and find the appropriate solution to prevent their reoccurrence.
Moreover, as illustrated in the above poster, clinical governance can also create a suitable perioperative environment for patients and staff. One of the clinical governance pillars is to educate and train medical practitioners; therefore, creating the poster to raise postoperative awareness is to achieve and fulfill the role of patient advocate (Cleary & Duke, 2019). Similarly, creating the poster is raising postoperative fever awareness and giving professional educations to patients and healthcare providers.
Using the poster to raise awareness about postoperative fever is essential as it is long-lasting and reaches a broad audience. Meanwhile, using the poster to display the information about postoperative fever does not mean that many people will gain knowledge about the issue. According to Papanas et al. (2019), posters are also used in medical sectors to reduce education systems costs, which are most costly. Consequently, it will allow medical staff, patients, and their families to learn the type of change required for postoperative fever prevention and treatment to be effective.
Conclusively, medical posters are necessary educational materials that raise risk awareness, show that trust protects patients’ rights to receive the best medical treatment, and the ways that patients and medical practitioners can use to reduce, manage, and prevent such risks. In the healthcare sector, the public needs assurance that NHS care of high quality and such assurance can be given by clinical governance. From the paper, it is apparent that, apart from improving and safeguarding the standard of care and the effective implementation of management strategies, clinical governance can help reduce the number of patients suffering from postoperative fever, and in so doing, improve patient care.
References
Cleary, S., & Duke, M. (2019). Clinical governance breakdown: Australian cases of willful blindness and whistleblowing. Nursing Ethics, 26(4), 1039-1049.
Field, N. C., Raviv, N., & Adamo, M. A. (2019). Utility of postoperative fever workup after craniosynostosis repair. World Neurosurgery, 132, e430-e433.
Maday, K. R., Hurt, J. B., Harrelson, P., & Porterfield, J. (2016). Evaluating postoperative fever. Journal of the American Academy of Physician Assistants, 29(10), 23-28.
Papanas, N., Georgiadis, G. S., Demetriou, M., Lazarides, M. K., & Maltezos, E. (2019). Creating a Successful Poster: “Beauty Is Truth, Truth Beauty.” The International Journal of Lower Extremity Wounds, 18(1), 6-9.
Price, T., Tredinnick-Rowe, J., Walshe, K., Tazzyman, A., Ferguson, J., Boyd, A., Archer, J., & Bryce, M. (2020). Reviving clinical governance? A qualitative study of the impact of professional regulatory reform on clinical governance in healthcare organisations in England. Health Policy, 124(4), 446-453.
Veenstra, G. L., Ahaus, K., Welker, G. A., Heineman, E., van der Laan, M. J., & Muntinghe, F. L. (2017). Rethinking clinical governance: Healthcare professionals’ views: A Delphi study. British Medical Journal Open, 7(1).
Wakefield, E. (2018). Compassion fatigue in the perioperative environment. Journal of Perioperative Nursing, 31(2), 21-24.