Roles of the WHO, the DH, and local authorities in the identification of health and diseases in the UK
In the UK, the World Health Organisation (WHO), the Department of Health (DH), and local authorities have differing roles in ensuring the containment, treatment, and prevention of diseases. The WHO provides leadership in various critical issues relating to health coupled with engaging in partnerships with the DH and local authorities in preventing diseases. It shapes the research agenda together with simulating, translating, and ensuring the dissemination of knowledge on best practices in the health care sector. In addition, the organization assesses health trends and ensures sustainability in various organizational capacities in a bid to deal with health challenges within the UK.
The DH has the obligation of ensuring that people live long and healthily. The DH offers strategic directions to the NHS coupled with the broad UK healthcare system. Through the provision of stewardships, the DH ensures that people have access to appropriate healthcare services. This goal is accomplished through its participation in developing national policies coupled with influencing various global leadership health initiatives.
The local authorities contribute to the identification of health risks and diseases in the UK population. For example, clinical commissioning groups (CCGs) provide rehabilitating care, community-based healthcare services, and respond to urgent and emergency care needs at local levels. The Department of Health (2013, p.15) adds that the CCGs participate in ‘arranging emergency and urgent care services within their boundaries and for commissioning services for any unregistered patients who live in their area’.
Epidemiology of HIV in the UK
Intervention programs are developed by the appropriate epidemiological, social, and environmental assessments. McKetin, Najman, and Baker (2012, p.2001) note that epidemiology is ‘the study of the distribution and determinants of health-related states or events in specific populations and the application of this study to control of health problems. An epidemiological assessment takes analytical and descriptive forms (Needle et al. 2011). Descriptive epidemiology entails the assessment of the occurrence of health challenges in the context of time, place, and a specific group of people. HIV and AIDS prevalence levels in the UK are described in this context.
In the UK, over 98,000 people were living with HIV and AIDs at the beginning of 2013. Averting HIV and AIDs (2013) informs that 22% of these people did not know about the infection. Averting HIV and AIDs (2013, par. 6) adds that in 2012, ‘the UK recorded new detections amounting to 6360, thus cumulating into 27,798 diagnosed cases in the same year’. By the beginning of 2013, the UK recorded 21,117 deaths of people living with the disease. Graph 1 below illustrates statistics on HIV and AIDS in the UK until 2012.
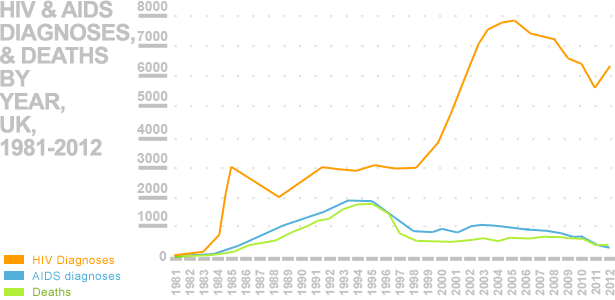
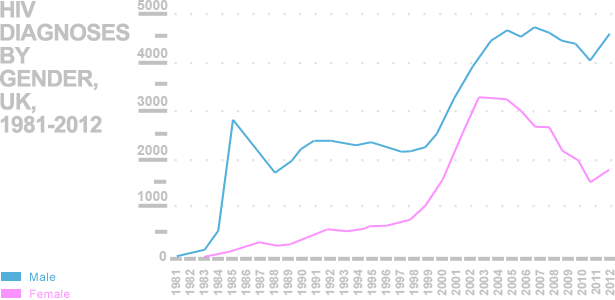
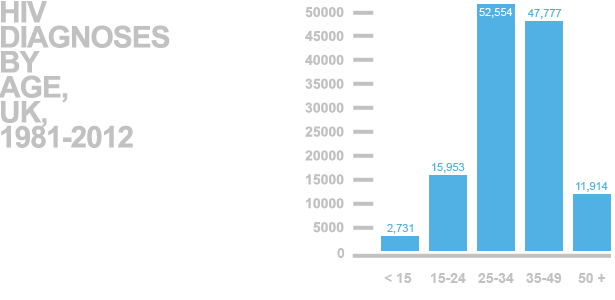
In the UK, HIV was first common among gays, people sharing needles for drugs injection, and those receiving blood and its related products. These groups comprised the high risks individuals, although the introduction of blood screening coupled with ART treatments has reduced both the number of new diagnoses and deaths related to the disease. Based on the 2012 statistics, HIV is common among men (as shown in graph 2) between 25 and 49 years, but more prevalent among 25-34 youngsters as shown in graph 3.
Yin et al. (2013, p.84) note that in ‘2013, approximately 107,800 people living with HIV died. In the same year, the UK reported 6000 new cases of infection’. 545 of these cases were among gays. By the end of 2013, 24% of those living with HIV were undiagnosed (Yin et al. 2013). This aspect implies they did not have access to ART.
Effectiveness of approaches and strategies used by NHS to control HIV
The NHS deploys different strategies and approaches to control HIV and AIDS in the UK. The most effective approaches entail preventing infection, rather than treating it. Preventive strategies entail encouraging people to avoid various risks factors like unprotected sex or sharing needles, syringes, or any other instrument for piercing the skin. However, for those already infected, the NHS deploys different preventive strategies. For example, using ART to ensure that people reduce the risk of infecting others. The effectiveness of these approaches depends on their capacity to reduce new infections and ensure that the already infected people live long just like the uninfected people.
The current priorities for the prevention and control of diseases and risk factors in the UK
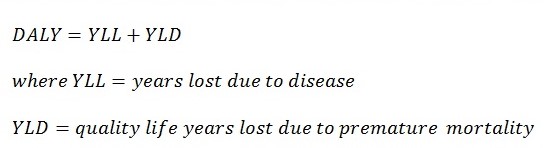
The current UK policies focus on reducing the disease burden. According to Lozano et al. (2012, p.2095), this aspect refers to ‘the impact of health problems as measured by financial costs, mortality, and morbidity of other indicators’. QALYs or DALYs quantify it. A DALY may be taken as a year of quality life lost due to diseases. The overall disease burden may then be computed as the gap occurring between ideal health and an individual’s current health status. The formula for DALYs is:
In a bid to decrease the burden of disease, the NHS and supporting partners at local levels have established various healthcare priorities. They include supporting self-health care management initiatives, primary, secondary, and tertiary prevention, and care coordination among teams for social care and the integrated healthcare system together with proper management of medicine. Good medicine management is important in ensuring cost-effective ways of administering primary care. Moreover, such management creates ways of ensuring that patients manage their health conditions effectively. Indeed, the management of medicine as a priority for the UK healthcare system aids in the reduction of medication errors, which may harm patients, thus increasing DALY.
In managing HIV/AIDS, the focus is on primary, secondary, and tertiary prevention. The primary prevention focuses on reducing new infections by encouraging the use of condoms, mouth dams, and conducting health education among different high-risk groups like MSM and people sharing injecting devices. It conducts screening and testing of HIV/AIDS to ensure that the infected individuals can start medication early enough. Secondary prevention ensures that few HIV people progress to AIDS. This aspect leads to the reduction of severity of the disease, thus giving it low DALY values. This aspect includes offering psychosocial support, education of treatment options, harm reduction through nutrition, and offering peer intervention services (El-Sadr et al. 2012). Tertiary prevention ensures that the infected people live quality lives. It ensures the rehabilitation of HIV-infected persons. For example, the UK uses ART in limiting rapid progression coupled with likely associated infections.
Currently, there is no known cure for HIV. However, medicinal and therapeutic treatment options are available. Their goals entail providing patients with relief from symptoms, pain, and stress of illness. Options like ART and OI prophylaxis ensure that patients live quality lives by curtailing progression into AIDS.
Relationship between the prevalence of HIV in the UK and the requirements of health services to support the infected individuals
The UK health service system has a primary responsibility of ensuring low-risk levels of contracting diseases coupled with ensuring quick response to treatment of individuals and the public. The prevalence of HIV is high amongst MSM and people sharing injecting needles (Lozano et al. 2013). While the nation has elaborate expertise to deal with HIV/AIDS, the prevalence level among these groups remains high due to the reluctance to seek prevention services. However, the government and social care partners have allocated high funding to local organizations and social care to help in dealing with the problems. These organizations depend on such funding to educate and rehabilitate drug addicts.
Planning is critical in ensuring ardent response to diseases including HIV and AIDS. Therefore, planning for medicine and treatment for HIV correlates directly with the reduction of prevalence levels. The accessibility to healthcare facilities is critical in increasing testing rates, which are necessary for primary, secondary, and tertiary prevention and treatment processes. These concerns have made the UK, through the NHS, not only increase its funding to local levels facilities for treating and managing HIV/AID, but also ensure that the organizations have the requisite capacities. While HIV management as a public issue in the UK is an objective of the DH, individual awareness on the need to seek health care education and treatment of HIV/AIDS relates directly to the prevalence levels. For example, individuals addicted to drugs and their abuses are less likely to make the initiative of accessing public goods (Lozano et al. 2013).
The impact of lifestyles choices on future needs for health and social care services
Lifestyles have an impact on HIV. Therefore, lifestyle choices affect future needs for health and social care services. For example, choices like diet and nutrition may increase susceptibility to contracting certain infections, which for HIV increases the progression to AIDS. Fawzi (2004) argues that limited consumption of calories and proteins lowers immunity levels. The deficiency of vitamin A, B12, and E coupled with minerals like zinc lowers CD4 cell count. This aspect implies that choices on the diet may increase the need for health and social care services through developing programs for supplying minerals and vitamin supplements to individuals as a public good.
The changing prevalence of substance use may influence health and social care service policies. For example, the increased use of recreational drugs would require the development of programs for reducing their consumption. Beach (2006) posits that evidence-based research shows that increased use of drugs not only increases risks for contracting HIV but also it raises the progression rate. For instance, cocaine increases the capacity of HIV to destroy the immune system by lowering the production of cytokines. Exercise and relaxation are important aspects in reducing work anxiety and stress. Flexible work culture ensures that people have sufficient time to attend to health needs like visiting healthcare facilities for testing and management of their health. However, excessive flexibility may increase leisure time, thus making people resort to more indulgence in risky behaviors like abusing drugs or engagement insecure relationships.
The assessment of health and wellbeing priorities for people living in London
People living in London have health and wellbeing priorities like increasing access to health information and receiving preventative health services to promote their welfare through screening and creation of new healthy lifestyles. They prioritize safety and security, mobility, and hygiene coupled with intellectual, social, and emotional needs.
From 2013, the roles of the DH changed to focus on offering governance and leadership in health care. This move left the responsibility for setting health and well-being priorities to other partners in the healthcare sector. According to the Department of Health (2013, p. 5), these are ‘commissioning groups (CCGs) and 19 commissioning support units (CSUs alongside NHS England, Health Education England (HEE), Public Health England (PHE), and the NHS Trust Development Authority (NHS TDA), and152 health and wellbeing boards’. These bodies determine the health and well-being priorities through the inclusion of all stakeholders in the development of priorities and setting mechanisms for their implementation using funding provided by the DH. This move brings together commissioners among them representatives of CCGs, senior managers, and elected people in London city councils, social care representatives, health watch representatives, and the director of public health.
The identified health and well-being priorities are right for people living in London. They cut across many risk factors of health and well-being and mechanisms of responding to them. For example, substance abuse including alcohol is a risk factor for indulgence in risky behaviors, thus increasing the prevalence levels for HIV infections. For those already infected, a priority like increasing access to preventive care services and a healthy eating lifestyle are important aspects of reducing the progression to AIDS. The priorities may not be exhausted. Emerging lifestyles and trends create additional health challenges. However, the bodies developing care policies can develop new priorities to cope with emerging problems.
Effectiveness of strategies, systems, and policies for ensuring health and well-being of service users with HIV/AIDS
Healthcare facilities in London are well equipped with expertise and necessary support equipment for testing HIV/AIDS safely, especially to other service seekers and medical personnel (Averting HIV and AIDs 2013). The service is organized such that people are prepared both emotionally and psychologically before taking tests. This aspect helps to increase the likelihood for people to come for future tests and access treatment for those testing positive.
People are not forced to take the service. Therefore, their fundamental freedom in making choices is observed. For those discontented with the service, they are given opportunities to raise their complaints to the administrations. This aspect ensures that people can push for facilities to provide quality service in terms of reliability, efficiency, and effectiveness, thus allowing them to make good choices and alternatives about their health. HIV prevention and treatment require partnerships.
The NHS requires all facilities to link and share information on evidence-based ways of responding to both HIV and its risk factors. The health and well-being of people in London are recognized by the NHS policies. Therefore, the participation of friends and families is highly encouraged to help in speeding the recovery process by providing the necessary emotional support.
Changes for improving the health and wellbeing of people living in London
Health education is a major policy that the NHS explores in a bid to ensure that people have access to reliable health information, which then helps them make informed choices. While inputs from specialists coupled with their consultation are important in developing health and well-being policies, evidence-based risk factors should be controlled. Necessary changes are important like banning the promotion of unhealthy foods like fast foods containing high calories in a bid to control obesity (Rajaratnam et al. 2010). The imposition of high taxes coupled with banning the promotion and consumption of alcohol and smoking by highly susceptible groups is necessary.
Activities implemented to encourage behavior change for minimizing health for individuals living in London
‘Change4 Life’ is one of the programs implemented by the NHS to discourage the consumption of unhealthy foods. The campaign is informative. People are given information over the television on the contents of foods that they select from stores. In England, 24% of men and 26% of women are now obese while 58 percent women and 65 percent men are classified as either obese or having excessive weight (Food and Consumer Beverage News 2015). However, the pertinent question is whether the campaign reduces these figures to the 1993 levels (13% men and 16% women). The case of France perhaps exemplifies the effectiveness of such a campaign. France lowered overweight among children by 2.6 percent between 2000 and 2007 via a similar campaign. The campaign will reduce government revenues from low sales of products that NHS labels as ‘unhealthy’. It also costs the NHS to run it on national TVs. However, these costs may be covered by the campaign’s benefits like reduced prevalence levels for obesity coupled with its treatment and management of the associated chronic ailments like diabetes and hypertension. Conclusively, running the commercial is important. Regardless of the involved costs, the promotion of good health is a priority of the NHS. However, it needs to ensure that healthy brands are attractive to the consumers in a bid to increase the appeal of the brand to them and minimize chances of selection of unhealthy brands at the consumer outlets.
Reference List
Averting HIV and AIDS: UK HIV and AIDS Statistics 2013, Web.
Beach, C 2006, ‘Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV’, Journal of General Internal Medicine, vol. 21, no.6, pp. 661-665.
Department of Health: Protecting the Health of the Local People 2013, Department of Health and Public Health England, London.
El-Sadr, M, Holmes B, Mugyenyi, P, Thirumurthy, H, Ellerbrock, T & Ferris, R 2012, ‘Scale-up of HIV treatment through PEPFAR: a historic public health achievement’, Journal of Acquired Immune Deficiency Syndrome, vol. 60, no.3, pp 96–104.
Fawzi, W 2004, ‘A randomised trial of multivitamin supplements and HIV disease progression and mortality’, New England Journal of Medicine, vol.351, no.1, pp 23-32.
Food and Consumer Beverage News: Effectiveness of Change4Life’s New Campaign 2015, Web.
Lozano, R, Naghavi, M, Foreman, K, Lim, S, Shibuya, K & Aboyans, V 2012, ‘Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010’, Lancet, vol. 380, no.12, pp. 2095–212
Lozano, R, Ortblad, K, Lopez, D & Murray, J 2013, ‘Mortality from HIV in the Global Burden of Disease study – authors’ reply’, Lancet, vol. 381, no.5, pp. 991–992.
McKetin, R, Najman, J & Baker, A 2012, ‘Evaluating the impact of community-based treatment options on methamphetamine use: findings from the Methamphetamine Treatment Evaluation Study (MATES)’, Addiction, vol.12, no.7, pp. 1998-2008.
Needle, J, Petchey, P, Benson, J, Scriven, A, Lawrenson, J & Hilari, K 2011, The Role of Allied Health Professionals in Health Promotion, NIHR, London.
Rajaratnam, K, Marcus, R, Levin-Rector, A, Chalupka, N, Wang, H & Dwyer, L 2010, ‘Worldwide mortality in men and women aged 15-59 years from 1970 to 2010: a systematic analysis’, Lancet, vol. 375, no.32, pp. 1704–1772.
Yin, Z, Brown, A, Hughes, G, Nardone, A, Gill, O & Delpech, V, HIV in the United Kingdom: 2014 Report, Public Health England, London.