Introduction
Different approaches to leadership exist, and their appropriate use in healthcare is critical. Among other things, surgical settings need suitable leadership approaches (Aufegger, Shariq, Bicknell, Ashrafian, & Darzi, 2019). Shared leadership (SL) presupposes a horizontal approach to leadership, in which entire teams share tasks and responsibilities (D’Innocenzo, Mathieu, & Kukenberger, 2016). Given that team performance is enhanced through SL (D’Innocenzo et al., 2016), it is reasonable to introduce SL into a given surgical setting, which can be achieved through training (Tafvelin, Hasson, Holmström, & Thiele Schwarz, 2018). In this proposal, it is offered to use SL training to introduce SL elements into a specific surgical setting that the researcher has access to with the goal of improving team performance, as evidenced through unit-gathered data.
Background and Significance
The problem of choosing appropriate leadership styles in healthcare settings is a complex one. It is further complicated by the fact that while there is some data on different types of leadership, specific ones may be understudied; for instance, SL in surgical settings is barely covered (Aufegger et al., 2019). Simultaneously, the benefits of SL, especially in settings that require shared understanding and objectives, are well-evidenced in recent meta-analyses (Aufegger et al., 2019; D’Innocenzo et al., 2016). Surgical settings may be especially likely to benefit from SL due to the complexity of related tasks and the importance of coordinating different roles (Aufegger et al., 2019).
The surgical setting that the researcher has access to does not explicitly employ SL; also, its SL has not been measured. Therefore, its team coordination may be improved through the introduction of SL (Aufegger et al., 2019; D’Innocenzo et al., 2016). Furthermore, with the small amount of research on the topic, it is reasonable to proceed with studying it. Thus, the proposed research is significant for the given setting and research on surgical leadership.
PICOT, Evidence Review Questions, and Timeline
PICOT 1 (clinical problem): in a surgical unit team (P), does an SL training (I) improve critical team performance (O) as compared to pre-training data (C) over four weeks before and after the training (T)?
PICOT 2 (innovation): in a surgical unit team (P), does SL training (I) improve SL score (O) as compared to pre-training outcomes (C) four weeks after the training (T)?
The setting (P) is a surgical floor team in an institution that the researcher has access to; currently, it does not use SL, and its baseline SL has not been measured (C). The training (I) will be adjusted to fit the needs of the project with speed and setting as the most critical features. The literature that discusses training and SL training will be used to that end (Tafvelin et al., 2018). The SL Perception Scale (O) by Wood (2005) will be used to test the outcomes of the training. This scale has been tested by Wood (2005); the Cronbach alpha was greater than 0.70 for all items, and factor analysis showed that the measures were sufficiently distinct. The team performance outcomes (O) will be based on the data that are already being collected by the unit. The timeline is rather short (T), but it is determined by the needs of the project.
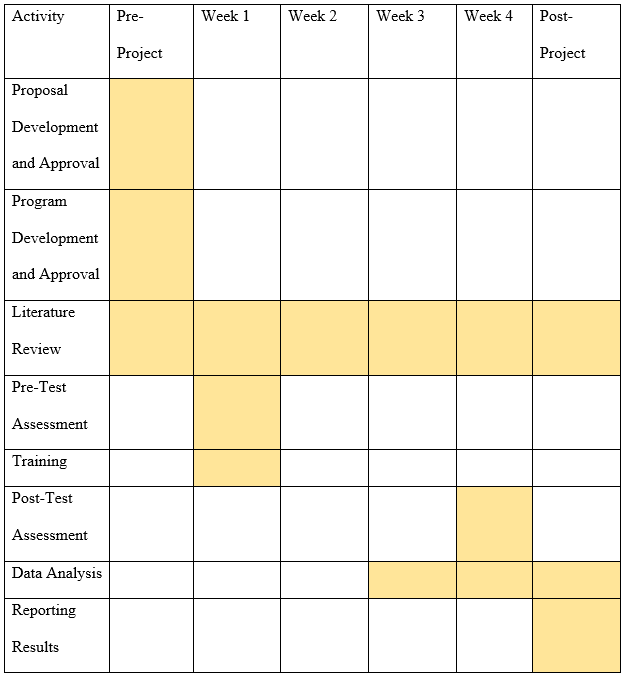
Table 1 presents the approximate timeline, which shows that the project will take up four weeks, but certain activities will be carried out before and after it. Specifically, project approval with the Institution Review Board, adjustment of the training, and obtaining permissions may take some time. However, the project itself will involve following the unit for four weeks and testing pre- and post-training SL perceptions for that period. For team performance, the unit-gathered data for four weeks before and four weeks after the training will be considered.
Search Strategy
The current search strategy consists of accessing databases that are typically used in healthcare research, as suggested by the relevant literature, for example, Polit and Beck (2017). The keywords are SL, surgery, surgical units, and surgical floors. The currently performed search can be seen in Table 2.
Table 2. Search Strategy.
A literature search in one of the most well-established medical databases, which is PubMed (Polit & Beck, 2017), suggests that SL in surgery units is not very well-covered. However, at least one recent article presents a literature review on SL that incorporates surgery-related considerations (Aufegger et al., 2019). Many more diverse articles (from meta-analyses to correlational studies) discuss SL or surgery in terms that can be used for a synthesis of the literature (D’Innocenzo et al., 2016; Goksoy, 2016; Forsyth & Mason, 2017; Tafvelin et al., 2018). Only recent articles were included to ensure the use of up-to-date data, which is recommended by healthcare research literature (Polit & Beck, 2017). Thus, the proposed project can be substantiated with very recent studies, but more research on SL in surgery is necessary, which justifies working in that direction.
References
Aufegger, L., Shariq, O., Bicknell, C., Ashrafian, H., & Darzi, A. (2019). Can shared leadership enhance clinical team management? A systematic review. Leadership in Health Services, 32(2), 309-335. Web.
D’Innocenzo, L., Mathieu, J., & Kukenberger, M. (2016). A meta-analysis of different forms of shared leadership–team performance relations. Journal of Management, 42(7), 1964-1991. Web.
Forsyth, C., & Mason, B. (2017). Shared leadership and group identification in healthcare: The leadership beliefs of clinicians working in interprofessional teams. Journal of Interprofessional Care, 31(3), 291-299. Web.
Goksoy, S. (2016). Analysis of the relationship between shared leadership and distributed leadership. Eurasian Journal of Educational Research, 16(65), 295-312.
Polit, D.F., & Beck, C.T. (2017). Nursing research: Generating and assessing evidence for nursing practice (10th ed.). Philadelphia, PA: Lippincott, Williams & Wilkins.
Tafvelin, S., Hasson, H., Holmström, S., & Thiele Schwarz, U. (2018). Are formal leaders the only ones benefitting from leadership training? A shared leadership perspective. Journal of Leadership & Organizational Studies, 26(1), 32-43. Web.
Wood, M. S. (2005). Determinants of shared leadership in management teams. International Journal of Leadership Studies, 1(1), 64-85.