Introduction
Cancer in general is a disease caused by genes that have mutated or adapted in a different way that was intended. When the genes that control the reproduction and division of cells become damaged, cell replication and division takes place at an uncontrollable rate. Growths begin to develop in the surrounding tissue which eventually leads to the formation of cancerous cells in the body. All studies performed in cancer research have shown that the many forms of cancer are genetic because they are triggered by altered genes. However, only a small percentage of human beings inherit cancer within their family generations as the gene mutations are transferred from one generation to another (Diane Publishing 12).
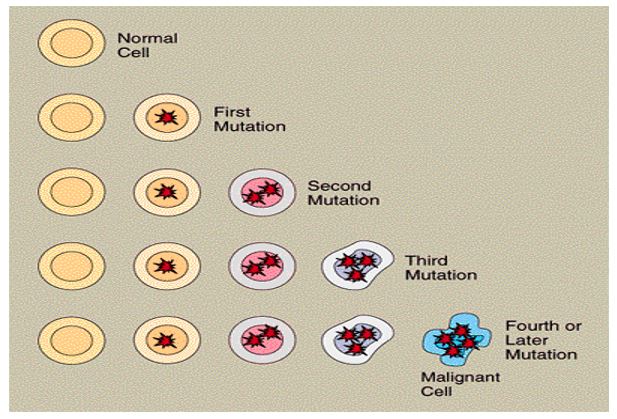
Most forms of cancer are usually caused by random mutations that occur in the body cells of an individual during their lifetime. Such mutations can be caused by a variety of factors with the most common being improper cell replication or division. Exposure to environmental agents that are hazardous in nature such as radiation or nuclear energy is also a contributing factor to cell mutations within the body. The development of cancer within the body from a normal to a malignant state usually occurs in a series of steps that are controlled by a specific set of genes referred to as oncogenes. These genes usually encourage the growth of cells within the human body but in the event they become damaged, altered or mutated, they spur the uncontrollable growth of cells within the body which leads to tumor growths (Diane Publishing 12).
Other genes that contribute to the growth of cancerous cells are the tumor-suppressor genes that ensure that cell growth has been restrained within the human body. When these cells are over expressed or inactivated by a mutation, they allow cell division to take place at an uncontrollable rate. Tumor suppression genes are the most common causes of breast and ovarian cancer as well as Li-Fraumeni syndrome and retinoblastoma. Other genes that trigger cancer in human beings are the DNA repair genes which when they fail to trigger the repair of mutated or altered cells, they lead to the accumulation of many cell mutations in thousands of sites within the body which eventually lead to the development of cancer. The diagram below demonstrates the mutations that various gene cells go through in the human body and how these are transferred from one generation to another. The diagram demonstrates how cell progression moves from a normal to a malignant to a metastatic state and how these stages are controlled by a different set of genes (Diane Publishing 13).
Breast Cancer
Breast cancer is a disease that is manifested by the abnormal division of cells within the breast. Breast cancer occurs when the genes that make up the breast tissue accumulate mutations in their cells that go on for a long period of time. When a vast number of cells carry gene mutations, the growth and development of cells within the breast tissue becomes next to impossible. Every time a cell goes through cell division, the gene mutations are usually transferred to the newly created cells. This means that every cell division leads to the growth of gene mutations and cell alterations in millions of other cells that exist within the human body. These cell mutations and alterations change the functions of healthy cells within the breast tissue that in the end lead to the growth of rogue cells referred to as cancer. Cancerous cells are not like any bacteria, fungi, or viruses that might affect the cells of an individual’s body. Cancerous cells are instead normal cells that have been irrevocably damaged or altered (Ricks 127).
The cell mutations as mentioned earlier are transferred from one generation of the family to another or they can be acquired from a range of assaults that alter the normal functionality of a human being’s genetic material. These assaults come from different sources such as changes in the body’s own hormones, radiation, or exposure to chemicals that might damage the functioning of the body’s genes. With regards to breast cancer, genetic mutations play a big role in increasing the risk of a person developing breast cancer. It is deemed to be caused by genetics because it occurs after the gene mutations have taken place in a person’s cells (Ricks 127).
The assaults that cause breast cancer in human beings are not as obvious as those that cause lung cancer that have been attributed to cigarette smoking and those that cause thyroid cancer that have been attributed to the exposure of thyroid cells to radiation. Doctors have been unable to determine the main causes of breast cancer that have led them to assess the risk factors that might predispose a person to breast cancer. One of the most commonly used risk factor includes assessing the genes of women or men who have a family history of breast cancer. Doctors have viewed that inheriting a genetic predisposition that leads to the formation of breast cancer might mean that an individual is at a higher risk of developing breast cancer when compared to an individual from a family that had no genetic predispositions. Studies have shown that people who have a genetic predisposition to breast cancer develop mutations from birth. This explains why many breast cancer cases are reported in people within the 30 to 50-age bracket (Ricks 128).
Other risk factors that are used in determining the likelihood of an individual developing breast cancer include a biopsy that reveals the presence of typical hyperplasia or LCIS, a gene mutation in the BRCA1 or 2 genes, early periods that begin before the age of twelve, menopause that occurs after the age of 55, post menopausal obesity and taking hormone replacement therapies. Some of these risks contribute in a slight way to the development of breast cancer with the most common causes of breast cancer being mutations in the BRCA1 and 2 genes (Ricks 126). Other testing criteria that are used to determine whether an individual has breast cancer include testing an individual from a family that has a known mutation of the BRCA 1 and 2 genes, assessing the personal history of the individual (Chung and Haber 41).
The most common form of breast cancer is referred to as ductal cancer and it leads to tumor growths in the cells that line the milk ducts. Another type of breast cancer is referred to as hereditary breast cancer that is associated with inherited gene mutations that exist within a family. Hereditary breast cancers are deemed to occur earlier in life when compared to the non inherited or sporadic cancer cases that occur at a later period in life. Researchers have estimated that more than 178,000 new cases of breast cancer are diagnosed every year around the world (Chung and Haber 41).
The relationship between breast cancer and genes
The National Cancer Institute based in United States estimates that the number of people who have inherited gene mutations that lead to the development of breast cancer account for 5 to 10% of the 211,000 cases of breast cancer that occur in the US. This means that a large majority of breast cancer cases were caused by reasons that were and could not be easily explained by medical research. The Institute however supported research evidence performed by medical practitioners and scientists that stated that breast cancer was related to a gene mutation carried from one generation to another. Dr. Mary-Claire King made a historic discovery in 1990 that would determine whether there was a link between genetics and breast cancer. King identified a gene that was similar in family members that had breast cancer and this gene was deemed to be the main cause in families that had rare forms of breast cancer in both the male and female members (Ricks 129).
King discovered that the gene had similar series of mutations among the family members who had breast cancer despite the fact that is was varied in a general population. King together with other research scientists referred to this gene as breast cancer 1(BRCA1) which led to the mutations of inherited genes that would lead to the development of breast cancer. The BRCA1 gene according to King encoded a protein that was used to repair broken DNA cells when they failed to repair themselves. When the BRCA1 gene mutated, the damaged DNA cells could not be repaired which led to the uncontrolled division of cells that led to cancerous cell formations. Breast cancer that existed in families according to King’s research was associated with inherited mutations in BRCA1 genes (Chung and Haber 41).
King’s research paved the way for more research and studies that were conducted to determine whether there was a relationship between breast cancer and genes. The results of these studies revealed a number of genes that had a slight if not modest impact on the development of breast cancer and genes that elevated the risk of a person developing breast cancer. The genes that presented an elevated risk of developing breast cancer included breast cancer 2 (BRCA2), TP53, CDH1, STK11 and PTEN while those that presented a slight risk of developing breasts cancer included ATM, AR, RAD 50 and 51, BARD1, BRIP1, PALB2 and ERBB2 (Chung and Haber 41).
Some scientific work has shown that the inherited variants of the BARD1, ATM, CHEK2, RAD50 and 51 genes are associated with a more elevated risk of developing cancer. However, not all studies have shown that there is a connection between some of these inherited variants and the risk of developing breast cancer. Only studies that have focused on the ATM and CHEK2 genes have presented evidence that there is a connection that exists between developing breast cancer and inheriting the gene variations. Although 5 to 10% of breast cancer cases are attributed to penetrant cancer predisposition genes, individuals who have an inherited gene mutation are at a higher risk of developing breast cancer and other forms of cancers over the course of their lifetimes (Chung and Haber 41). The table below demonstrates the genes that are associated with a hereditary predisposition to breast cancer
(Source: Chung and Haber 42)
BRCA2 according to early studies was associated with cancerous cells that were found in similar phenotypes and clinical behaviors. BRCA2 just like BRCA1 is hereditary in nature and apart from breast cancer; it causes ovarian cancer, prostate cancer and pancreatic cancer. The mutations that occur in BRCA1 and BRCA2 account for over 80 to 90% percent of hereditary breast cancer cases in the world. Research work has shown that BRCA1 and BRCA2 are the major genes that are related to breast cancer within a predisposed family generation. These two genes function as tumor suppressor genes in controlling the reproduction of cells within the body but they fail to repair any broken DNA cells during the cell division process that leads to the formation of cancer. The BRCA1 and BRCA2 genes encode large amounts of proteins that are used in multiple cellular pathways and in the maintenance of genome integrity. When these two genes mutate, the risk of developing breast and ovarian cancer becomes higher especially in families that have a BRCA gene mutation (Chung and Haber 41).
Four years after Dr. Mary-Claire King’s discovery, researchers in the University of Utah identified the exact location of the gene mutation (BRCA1) that led to cancer. The gene mutation, BRCA1, was identified to reside on chromosome 17 while later studies revealed that BRCA2 was located in chromosome 13. When these two genes are healthy, they are able to function as tumor suppressors that control the division of cells within the body. When these two genes have any form of mutation or alteration in their gene formation, the individual faces a higher risk of developing breast cancer because the tumor suppression ability of the gene has been altered or changed, allowing for the growth of tumors (Ricks 130).
A study conducted by the New York Breast Cancer Study Group on a thousand women of Jewish descent revealed that mutations in either of their BRCA1 or BRCA2 presented an 82 percent chance of the women developing breast cancer during their lifetime. The study also revealed that when the BRCA1 gene mutated, an individual had a 54 percent chance of developing ovarian cancer in their lifetime. The study also revealed that women who were physically active during their teenage years could delay the onset of breast cancer in their formative years. The research revealed that physical exercise reduced the levels of estrogen available to cells that would lead to the formation of cancerous cells in the breast tissue (Ricks 131).
The results of the study demonstrated that gene mutations in the BRCA1 gene were more than likely to predispose a person to either breast or ovarian cancer. Any alterations that occurred in the BRCA1 gene while it resided on chromosome 17 would be accountable for over 5% of new breast cancer cases recorded in a year. While studies have shown that individuals inherit the gene mutations that cause breast cancer, most cases of breast cancer are associated with genetic changes that might occur on a person’s breast. This means that genetic changes are the most common causes of breast cancer instead of inherited breast cancer within a family. Therefore, gene mutations in the BRCA1 and BRCA2 genes which are found in nearly half of the families that have a high incidence of developing breast cancer account for 80 % of breast cancer and ovarian cancer cases in the world (Genetics par.16).
The chances of a person getting hereditary breast cancer are usually determined by the type of genes that they have inherited. Any mutations that take place in the BRCA1 and BRCA2 genes are usually inherited in an autosomal dominant pattern within a family that has the breast cancer causal gene. This means that any one copy in the BRCA gene mutation is more than likely to increase a person’s risk of developing breast cancer. The most important aspect that needs to be considered in determining the relationship between breast cancer and genetics is that individuals inherit an increased risk of getting cancer rather than an increased risk of getting the disease itself. It is also important to note that not everyone who inherits gene mutations to the BRCA1 and BRCA2 genes is likely to develop breast cancer (Genetics par.16).
The likelihood that an individual has a mutation in their BRCA1 and BRCA2 genes is determined by whether an individual has been diagnosed with breast cancer before the age of 50, whether female members of the same family have had breast cancer or ovarian cancer before the age of 50, whether the family is of a Ashkenazi Jewish descent which has a higher predisposition to breast cancer that other races. Most women who develop breast cancer do not usually have an inherited gene mutation in their BRCA1 and BRCA2 genes. Breast cancer in these women usually occurs from other gene mutations or sporadic mutations within their bodies (Genetics par. 10).
Conclusion
The discussion has dealt with determining the relationship that exists between breast cancer and genetics. The study has revealed that there are various genes that elevate the risk of a person developing breast cancer during their lifetime and these genes include the BRCA1, BRCA2, CDHQ, STK11, and TP53. The most common genes that elevate the risks of a person developing breast cancer have been identified as the BRCA1 and BRCA2 genes. The study has shown that every human being has BRCA1 and 2 genes, as they are important in suppressing tumor growths. When these genes are however faced with some mutations or alterations, they became unable to repair any broken DNA cells and they are also unable to suppress the growth of tumors. This means that cancerous cells are more than likely to occur when the BRCA1 and BRCA2 genes undergo some mutations. The existence of these two genes in the human body and their relationship to the elevated risks of developing breast cancer demonstrates that there is a relationship that exists between genetics and the development of breast cancer.
References
Chung, Daniel, and Daniel, Haber. The Massachusetts general hospital guide to clinical cancer genetics. New York: Springer Science, 2010. Print.
Diane Publishing. Understanding gene testing. New York: DIANE Publishing Company, 2004. Print.
Genetics. Breast cancer. 2011, Web.
Ricks, Delthia. Breast cancer basics and beyond: treatments, resources, self-help, good news, updates. California, US: Hunter House Publishers, 2005. Print.