Introduction
Surprise medical bills refer to the overcharging of patients when they receive care from out-of-network facilities, physicians, and clinicians. In most cases, patients are subjected to costs and bills above what insurers are willing to pay (H.R.3630 – No Surprises Act 116th Congress (2019-2020), n.d.). It is a form of conspiracy to gain high monetary returns from any medical service provider. This paper aims to explore the surprise medical bills given to consumers that ensue from various clinical experiences involving US patients, hospitals, and insurance providers. The paper will also present a grid with the No Surprise Act.
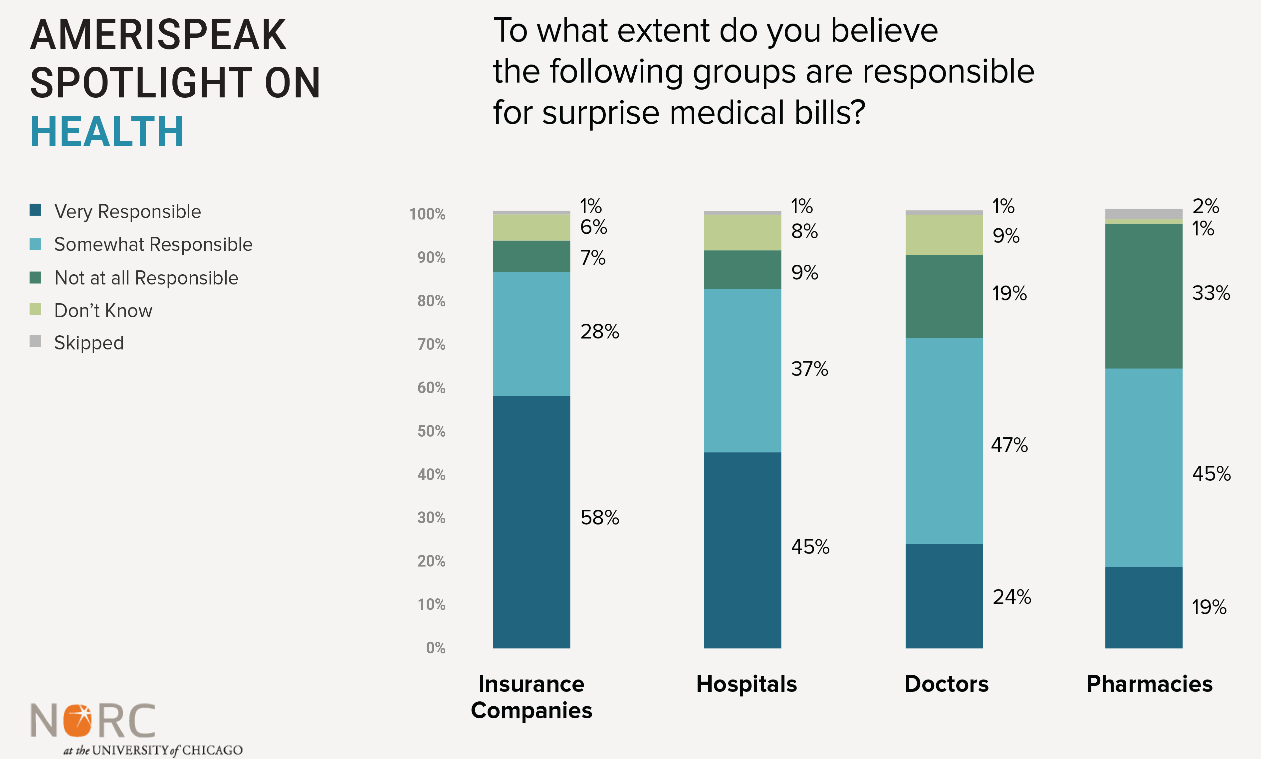
The No Surprise Act is a legislative statute that protects patients from getting ‘surprise’ bills in most cases where the outcome needs parting with a significant amount of money. About 66% of the US citizens report being worried about paying unexpected medical bills due to the nature in which the cost is calculated more so where someone received an emergency medical service (Levitt, 2022). The law was passed in December 2020 and favored the general public by having federal protection from uncertain out-of-network medical costs. Hiked medical bills are common where consumers receive care urgently without other medical options. About 57% of Americans have been surprised by medical bills that were thought to be under insurance cover (Young, 2022). 20% of the surprise bills result from the absence of a doctor from a given network. Insurers and hospitals are responsible for these unexpected charges, as shown in Figure 1 below (Young, 2022). The new law requires that a provider give at least 72 hours for a patient to sign consent for balancing medical bills that result from emergencies or acts of good faith during clinical procedures.
Legislation Comparison Grid Template
No More Surprise Medical Bills for Insured, Uninsured, and Self-paying Patients
There has been a raft of legislation testimonies that advocate for the full implementation of the Act. One of the testimonies is by the American Hospital Association (AHA) for the committee of the House of Representatives. The testimony titled ‘Hearing in protecting patients from surprise medical bills is meant to combat the unanticipated medical bills that affect the consumers economically (AHA, 2019). According to the AHA board, protecting patients is one of the key roles, and guided by clinical ethics, there is a need to end surprise medical bills (AHA, 2019). The legislative proposal was guided by the American hospital’s health system’s commitment to protecting patients from costly bills during circumstances that require medical procedures.
AHA gave scenarios where patients may get surprising medical bills. First, when there are emergency services outside the insurance network. Second, when the patient acts in good faith to get care within the network but unintentionally receives clinical care from out-of-network physicians (AHA, 2019). Additionally, it may apply where a health policy restricts coverage for urgent medical services, including in-network emergencies. Protection of patients is the key concern in this case, as all policies formulated should prevent patients from payment negotiations between insurers and the provider. Therefore, patients should have certainty in cost-sharing obligations based on balanced billing on an in-network account. The patients, in this case, have the privilege to get educated about the general ways in which insurance covers work.
The emergency department (ED) use has gone high in the last decade. More than 15% of the US population has been reported to visit ED (Adler et al., 2022). For example, if a person needs to have a medical check when they face health complications, they may seek services from the external network to prevent any mortalities. During the provision of clinical services, patients get surprising medical bills, more so the self-paying and those insured by service providers. In most cases, due to the good faith estimate, billing becomes in contention if it surpasses $400 more than the estimate (Adler et al., 2022). There is a need to fully implement the Act as one way of complementing health issues with the billing within the society.
Addressing Opponents
Opponents of the No Surprise Act base their arguments on the loss of revenue, which means collisions when it comes to interests. The controversy is evident as hospitals base their stand on the quality of care and the cost of delivering top-notch care to patients (H.R.3630 – No Surprises Act 116th Congress (2019-2020), n.d.). Thus, when there is a restriction on the payment, the firms may deliberately be unwilling to offer quality care which means the patients are at risk. To address the opponents, it is important to present the social and economic perspectives regarding this matter. First, subjecting a self-paying patient to a high medical bill means imposing indirect scarcity of resources in the future. The straining to get the cost settled affects the development of an individual economically, which may increase mortality chances (Robeznieks, 2022). Second, Hospitals should be the key facilities that save lives and offer medical care upon request without the conspiracy to manipulate patients financially. When those points are considered, it marks an important milestone in protecting consumers.
Conclusion
No Surprise Act is meant to protect patients from surprise medical bills resulting from emergency services in out-of-network settings. The key concern is to prevent paying expensive medical costs that the service providers may manipulate. AHA gave a legislative testimony on the need to protect patients. Opponents of this Act may be affiliated to returns on revenue. However, protecting consumers is the key priority that hospitals should be focused on achieving.
References
Adler, L., Trish, E., Fiedler, M., Ginsburg, P., Hall, M., & Ippolito, B. (2022). Understanding the No Surprises Act. Brookings. Web.
AHA. (2019). AHA testimony on protecting patients from surprise medical bills. American Hospital Association. Web.
Gordon, D. (2022). The No Surprises Act took effect January 1; here’s what it means for your medical bills. Forbes. Web.
H.R.3630 – No Surprises Act 116th Congress (2019-2020). Congress Gov. Web.
Levitt, L. (2022). Surprise medical bills are ending, but controversy continues. Jama Network. Web.
Robeznieks, A. (2022). The No Surprises Act is in effect. What physicians need to know. American Medical Association. Web.
Young, E. (2022). A new survey reveals 57% of Americans have been surprised by a medical bill. NORC.org. Web.