Animal-Assisted Therapy
Animal-assisted therapy is a type of therapy that employs animals for motivational and educational purposes, to facilitate treatment and improve social, emotional, or cognitive state of patients. However, there is also a number of scientific works pointing out the gaps in research concerning animal-assisted literature, which are made worse with their methodological weaknesses and the inconclusive nature of the results.
This papers studies animal-assisted therapy and how effective it is for retrieving better patient outcomes for people with terminal diseases, as opposed to the traditional palliative care methods?
Change Model Overview
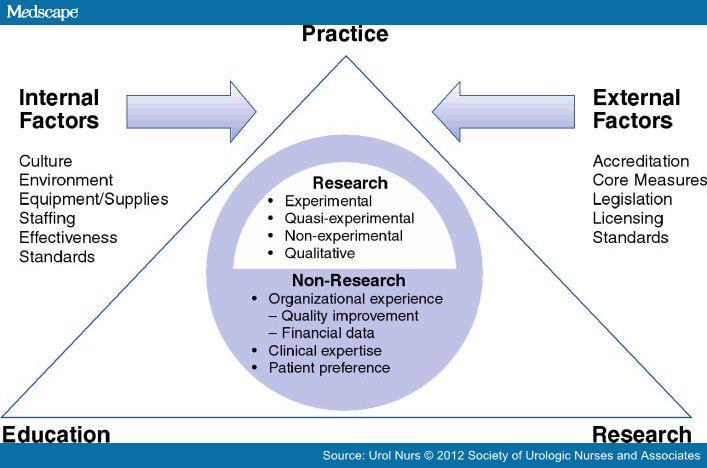
Johns Hopkins Nursing Evidence-Based Practice Process is the approach for effective clinical problem solving and decisions-making. It includes three-step framework, called PET, designed to help healthcare staff and practicing nurses develop best practices. These steps include practice question, evidence, and transplantation.
Practice Question
Step 1: Recruit Interprofessional Team
To conduct a high-quality assessment of the animal-assisted therapy, a diverse team of stakeholders is needed, which will be able to analyze both human and animal factors, their interactions, needs, and impact they have on the relationship. The team members would be composed of a research and a practicing nurse to organize data according to the PET steps, veterinarian, psychotherapist, a general practitioner physician, oncologist.
Step 2: Develop and Refine the EBP Question
The purpose of this Evidence-Based-Practice is the assessment of animal-assisted therapy as an influencing factor in reduction in depression levels, pain, and similar symptoms, management of emotional issues and spiritual needs in patients with terminal diseases, and how effective it is in comparison to standard palliative care or hospice therapy.
Step 3: Define the Scope of the EBP
A growing number of medical research is looking into the application of animal-assisted therapy medical settings, and are evaluating their effectiveness as a complementary, interprofessional intervention. The use of animals has proven to be able to decrease heart rate, blood pressure, respiratory rates, stress, depression, anxiety, and is seen as a cost-effective psychological, physiological, and emotional aid in a variety of healthcare areas.
However, while it has proven to facilitate the described above relaxation responses, few studies have validated its ability to alleviate “total” pain in palliative care settings with terminal patients. This gap in research makes it harder to evaluate its actual effectiveness in this field, and maximizing its potential (Marcus, 2013).
Steps 4 and 5: Determine Responsibility of Team Members
To study the effectiveness of animal assisted therapy on terminal patients, and how they compare to traditional medical care, a qualified psychotherapist would be needed to assess the effect of animals on the patients’ psychological well-being. In the same vein, the insight of an oncologist and a general practitioner physician would be needed to understand the physical, social, and mental hardships the terminal patients find themselves going through, as well as the traditional approaches that are used in this situation to handle their pain. A veterinarian would be needed to assess the animal’s role in the treatment. The research nurse on the team would be able gather the collected data from the mentioned above, in order to design best practices for animal-assisted palliative care using the Evidence-Based-Practice, and a practicing nurse would develop a plan for the integration of these practices into the terminal patient care.
Evidence
Steps 6 and 7: Conduct Internal/ External Search for Evidence and Appraisal of Evidence
This paper synthesizes and analyzes results from several past research articles, which rely on quantitative and qualitative methods of data aggregation and analysis. The studies analyze the application of animals in the medical setting, in particular when dealing with terminal patients, which aim to fill in the gaps in this area for research and create
The studies used in the paper were peer-reviewed, of high quality, and well accredited. The research papers based their conclusions on anecdotal and statistical data. The strength of this research is that it analyzed the data in the studied research and uses it to fully explore the practice question and alleviate it from different perspectives.
Steps 8 and 9: Summarize the Evidence
On the one hand, a number of studies have reported significant pain and emotional distress relief reported by terminal patients. Scientific analysis of the effect has discovered decreased levels of catecholamines, which are secreted during stress, an increasing the endorphin levels, which reduce the perception of pain and create a positive feeling in a manner similar to morphine.
The research compared the effects of human volunteers working with terminal patients, quiet procreative time alone (reading magazines), and the effect of therapy animals (dogs in the research). Overall, the best results were from the dog visits, with 70 percent of the patients reporting therapy as earthier afterwards, and 50 and 20 percents for volunteers and time spent alone (Marcus, 2013). “The Study Symptom Reduction Identified After Offering Animal-Assisted Activity at a Cancer Infusion Center” conducted a similar survey to determine how patients reacted to 10-15 minutes of therapy dog visits. Out of 121 pet therapy surveys, 56 were answered, and all patients referred to the experience as positive. It noted symptomatic improvements, regardless of various identifiers (Marcus, Blazek-O’Nei ll, & Kopar, 2014). The aspect of pain reduction was further explored in the study by Engelman (2013). This study used qualitative research to collect anecdotal evidence from palliative care patients, and provided examples of somatic pain reduction in patients as a result of interactions with therapy animals (Engelman, 2013).
On the other hand, a study “Furry and Feathered Family Members—A Critical Review of Their Role in Palliative Care” positioned that while animal companions may have a positive impact on terminal patients, the impact decreases the closer a person is to death, with human interaction becoming more important (Chur-Hansen, Zambrano, Crawford, 2015).
Step 10: Develop Recommendations for Change Based on Evidence
Based on the collected data, use of animal companions is significantly effective during the majority of the palliative care process. Integration of this therapy on a larger scale is bound to improve the patient mental well-being, and help them tackle their maladies better. However, the stage of the patient’s sickness and his preferences should also be accounted for.
Translation
Steps 11, 12, 13, 14: Action Plan
The final step of the PET process is translation, which evaluates the recommendations based on collected data in the evidence phase, and builds a strategy for their practical recommendation
- Use the patient case studies to develop a better understanding of the effects of animal therapy at different stages of terminal diseases in patients.
- Use the frameworks of the studied research to quantitatively compare the patient reactions to animal-assisted and traditional palliative care.
- Assess the current use of animal therapy in the country.
- Determine if improvement is possible through expansion of this area of care.
Steps 15 and 16: Evaluating Outcomes and Reporting Outcomes
The desired outcome for this research is a comprehensive understanding of the animal assisted therapy usefulness, and, consequently, use of Evidence-Based-Practice model to develop a treatment plan that would provide the maximum effectiveness.
Steps 17: Identify Next Steps
In order to gain a full comprehension of the practice question, the team would need to continue with the research by accounting for the discovered data, and use qualitative and quantitative research to conduct a more focused research, based on primary data, and held over a prolonged period of time, to assess the patient reactions at different stages of their care.
Step 18: Disseminate Findings
The most efficient way to educate the internal organization stakeholders would be by presenting the findings to them in the form of presentations and briefings, supported by patient and medical practitioner accounts. Outside the company, more attention can be drawn to this issue by publishing peer-reviewed medical articles in accredited journals and by speaking in medical panels, to receive coverage with the practitioners.
Conclusion
Animal assisted therapy provides a palliative care units with numerous benefits. While it cannot replace human interaction, it is still very effective at improving the mental and, in limited cases, physical well-being of terminal patients, by distracting them from their discomfort and providing a soothing effect to their psyche.
It is definitely an area of care that needs more research and attention, and which should be more widely employed.
References
Chur-Hansen, A., Zambrano, S. C., & Crawford, G. B. (2014). Furry and feathered family members—a critical review of their role in palliative care. American Journal of Hospice & Palliative Medicine, 31(6), 672-677. Web.
Engelman, S. (2013). Palliative care and use of animal-assisted therapy. OMEGA, 67(1-2), 63-67. Web.
Marcus, D. A. (2013). The science behind animal-assisted therapy. Current Pain and Headache Reports, 17(4), 322-328. Web.
Marcus, D. A., Blazek-O’Neill, B., & Kopar, J. L. (2014). Symptom reduction identified after offering animal-assisted activity at a Cancer Infusion Center. American Journal of Hospice & Palliative Medicine, 31(4), 420-421. Web.