According to Paulsen (2018), each patient needs extra care. The manager must consider the number of staff and the patient acuity and be aware of the staffing mix, which refers to the percentages of licensed or registered nurses (RN), licensed vocational nurses (LVN), and unlicensed assistive personnel or certified nursing assistants CNA) working at a given time. Managers must be aware of the personnel mix along with the total workforce. The provision of the best nursing care at the most affordable price requires the management to be aware of the patient’s acuity.
The staffing needs are expressed in the personnel budget because it is mainly based on a predetermined standard. This standard can be addressed in hours per patient-day (HPPD) (medical units), visits per month (home health agencies), or minutes per case (the operating room). Because the patient census, the number of visits, or cases per day never remain constant, the manager must be ready to alter staffing when volume increases or decreases (Paulsen, 2018). The standard formula for calculating nursing care hours per patient-day (NCH/PPD) is nursing hours worked in 24 hours divided by the patient census.
ICU Unit
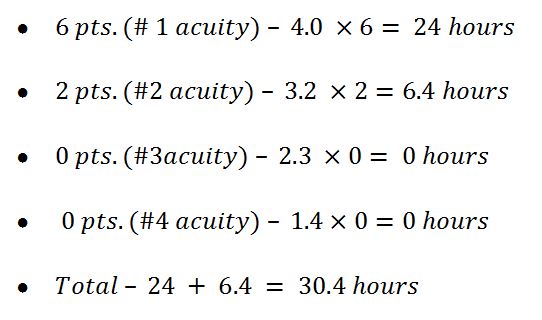
The hours needed to care for these patients are over 6.4 hours (30.4- 24=6.4 hours) the nursing workload, which means that the shift is understaffed and needs another nurse to be present.
Med Surg Unit
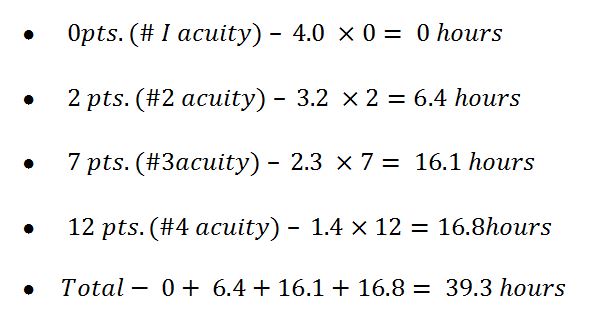
The total hours needed for nurses to care for patients are over 15.3 (39.3-24=15.3 hours) than their existing workload. The shift is still understaffed, although the difference is more than in the ICU Unit. Therefore, more nurses must be added to the shift to care for all patients adequately. The workload needs to be recalculated to staff the shift adequately. Therefore, changing the patients’ acuity level also makes their needs different.
Reference
Paulsen, R. A. (2018). Taking nurse staffing research to the unit level. Nursing Management, 49(7), 42. Web.