Introduction
A plethora of scholarly studies proves that obesity in children may be treated using healthy nutrition, adequate physical activity, and a stable psychological condition. At the same time, little attention paid to the formulation of evidence-based practices, and many nurses encounter problems with stimulating children to practice healthy lifestyles (Sim, Lebow, Wang, Koball, & Murad, 2016).
In this connection, motivational interviewing (MI) is one of the promising options that may be used to encourage children to control their weight. The purpose of this paper is to propose the study of motivational interviewing benefits in preventing childhood obesity in the context of the literature review method.
Significance of the Practice Problem
The growth in the prevalence of obesity in the child population of many countries over the past ten years became a non-infectious epidemic. The results of the recent study suggest that 17 percent of children aged between 2 and 19 are overweight, and the number of obese children doubles every three decades (Ogden et al., 2016). With the spread of obesity and overweight, such severe diseases as diabetes mellitus (DM), hypertension, coronary heart disease, various cancer types, and others tend to occur (Finkelstein, Graham, & Malhotra, 2014). Of the diseases associated with obesity, 2.5 million people die annually worldwide (Ogden et al., 2016). Overweight in childhood is often transformed into obesity in adults, which, in turn, represents a serious threat to health.
The identified problem creates the additional burden in economic and financial terms (high treatment costs), ethical issues (attitudes to obese patients by other children), and social barriers (communication and self-esteem difficulties) (Bean et al., 2015; Christie & Channon, 2014; Dawson et al., 2014). The legal aspect of the problem refers to the need to adjust policies and laws to assist the target population, while the latter also becomes vulnerable in terms of national security. Thus, the observed epidemic increase in the spread of overweight and obesity in the US requires a serious attitude on the part of healthcare organizations and care providers.
PICOT Question
- P (population) – school-age children at a high risk of obesity;
- I (intervention) – motivational interviewing;
- C (comparison) – a standard obesity prevention program;
- O (outcome) – proper weight management;
- T (time) – 1 year.
PICOT: In school-age children at a high risk of obesity, how does using motivational interviewing compared to a standard obesity prevention program impact proper weight management over a 1-year timeframe?
Theoretical Framework
The theoretical framework of cognitive-behavioral therapy (CBT) will be utilized for the proposed study, as it explains how certain behavioral patterns may be transformed positively. Aron Beck elaborated on the CBT in the nursing area and proved that it is effective. The theory allows, if necessary, to correct the unconscious inference of a patient with the desired behaviors. The interviewer does not teach a patient how to think correctly but assists him or her in understanding whether the usual type of thinking helps or hinders. The key to success is the active participation of a patient, while the principle of feedback is also important.
Synthesis of the Literature
MI is a style of communication with a patient that uses methods such as reflective listening and joint decision-making to identify how and why patients need to change their lifestyle. Borrelli, Tooley, and Scott-Sheldon (2015) found that MI about parent-child health interventions is likely to improve various types of behaviors, including diet and physical activity. These authors stated that interviewing allows making children and their parents closer to each other.
According to Christison et al. (2014), consider that MI in combination with the Family Nutrition and Physical Activity (FNPA) Screening Tool can contribute to the identification of obesogenic behaviors in children. From the financial and economic perspectives, Finkelstein et al. (2014) provide a qualitative study to assess the costs of treating obese children, which results in identifying $19 000 as an average spending per children compared to $12 660 for adolescents with normal weight. Ogden et al. (2016) explore the prevalence of childhood obesity within 20 years and state that it tends to grow steadily.
A range of studies illustrates that MI is effective in reducing BMI in overweight and obese children. As reported by Resnicow et al. (2015), the randomized-controlled trial allowed revealing that the intervention group significantly reduced it. The study by Bonde, Bentsen, and Hindhede (2014) is one of the first large-scale studies showing a significant reduction in BMI by MI implemented by pediatricians and nutritionists.
Consistent with the mentioned authors, Mallonee, Boyd, and Stegeman (2017) state that research shows that MI can be a powerful tool in the treatment of obesity in children. The value of the intervention lies in the fact that interviewers should imagine at what stage a person is and talk with him or her according to specific needs and open new opportunities or contradictions that were hidden from a child.
The important role of childhood obesity prevention through nutritional changes is also noted in the literature. Zhou, Emerson, Levine, Kihlberg, and Hull (2014) state that out of 15 studies that met the eligibility criteria of the systematic review were positive towards the role of obesity prevention interventions in childcare settings. The authors identify future research on costs, limitations, and follow-up reporting. Sim et al. (2016) made a review of the available literature related to child prevention, concluding that there is some evidence that proves the role of MI in nutrition improvements, yet it should be interpreted with caution due to different anthropometric data of children. Natale et al. (2014) also target role modeling and lifestyle habits of parents that critically affect children, especially those of preschool-age.
Some of the collected articles point to the potential of MI in treating childhood obesity in general. For example, according to Dawson et al. (2014), 1 session of MI used to provide feedback to parents of obese children was sufficient to encourage the former to start making changes. The weight feedback is discussed by Brown, Halvorson, Cohen, Lazorick, and Skelton (2015) focus on parenting strategies and behaviors practices in the family as the antecedents of obesogenic factors, which are regarded as effective.
The researchers evaluate the impact of motivational interviewing applied by primary pediatricians, nurses, and MI counseling nutritionists. Christie and Channon (2014) review the evidence published from 2006 to 2011 that integrated data about the last 20 years of research. The above authors state that there is great potential for MI in addressing both adult and child obesity. Also, Wang et al. (2015) found that school-based and home-related interventions should be combined to achieve success, which is shown in the extensive research funded by the National Institutes of Health and the US Agency for Healthcare Research and Quality (AHRQ).
Similar results are obtained in the study by Seburg, Olson-Bullis, Bredeson, Hayes, and Sherwood (2015): a comprehensive approach to weight management should be based on a range of interventions. Consistent with the above studies, Bean et al. (2015) who investigated brief MI sessions in enhancing diet and physical activity consider that it is a valuable method of treating obesity, especially among African-American children.
One of the differences that can be specified in the literature is a focus on children’s resistance to behavioral changes related to obesity prevention. As for gaps in the literature, one may identify several studies that demonstrate limitations to MI about child obesity prevention. Gorin et al. (2014) discuss the attempts to increase physical activity in children that have shown a low success rate. These researchers wanted to better understand the motivating factors for physical activity, which can shed light on the development of the best interventional change strategies. Hung et al. (2015) who performed a meta-analysis claim that the overall observation of school-based programs shows the inefficiency of obesity prevention programs, among which MI is also noted.
On the contrary to the majority of articles, Amiri, Kazemian, Mansouri-Tehrani, Khalili, and Amouzegar (2018) found that MI may be ineffective in some children, while the causes of such a trend are to be discovered in the future studies. In the course of the 24-month follow-up of a randomized controlled trial, Broccoli et al. (2016) discovered that MI was unsuccessful as the difference in the participant’s BMI indicators was insignificant. This large study that involved 372 families demonstrates that there is a need to specify long-term interventions that would work in a long-term period.
Practice Recommendations
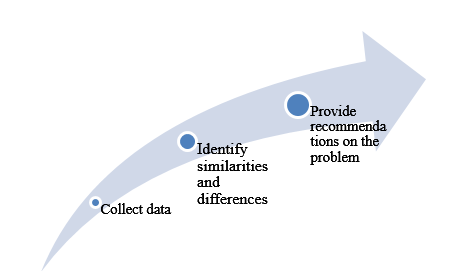
Based on the literature presented in the previous section, it is possible to anticipate that the research question will lead to a positive answer – MI improves obesity prevention. In this regard, it is possible to state that the evidence, including its consistency, quality, and quantity, seems to be sufficient to explore the given problem in detail and make appropriate recommendations for practical change. The algorithm for the proposed project may be viewed in Figure 1.
Bean et al. (2015), Borrelli et al. (2015), Christie and Channon (2014), Dawson et al. (2014), Natale et al. (2014), Seburg et al. (2015) recommend using MI to parent-child health interventions. Christison et al. (2014) suggest that MI should be used to reveal obesogenic child behaviors. Bonde et al. (2014), Mallonee et al. (2017), Resnicow et al. (2015) assume that MI is effective to reduce BMI in obese children.
Amiri et al. (2015), Broccoli et al. (2016), Brown et al. (2015), Dawson et al. (2014), Gorin et al. (2014) recommend conducting further research on the role of MI. Finkelstein et al. (2014), Hung et al. (2015), Ogden et al. (2016), Sim et al. (2016), Wang et al. (2015), Zhou et al. (2014) assume the need for further overall research in using interaction as a way to address child obesity.
Project Description
For this proposal that presents in the form of the literature review, I will select 20 articles from peer-reviewed journals that were published since 2014. Google Search engine will be used to collect relevant sources of data. Also, some websites of global and national healthcare organizations will be accessed to contain information about statistics and the most recent trends. Such keywords as child obesity prevention, motivational interviewing, behavioral change in obesity, and obesity change patterns will be used. The fact that I have access to our digital library will facilitate the research, while the possibility of controversial ideas may be a barrier.
The required resources are journals and websites; the collected results will be encrypted and stored within five years, after which they will be deleted. I will benefit from increasing my knowledge of the recent literature on the chosen topic. The foundation for evidence-based interventions is an advantage for nursing, and on the community level, a focus on awareness of falls in older adults and preventative health will be promoted.
Project Evaluation Results
The collected data will be combined according to several topics and compared regarding the impact of MI on the weight of children who are at risk of developing obesity. In other words, their body mass index (BMI) will be used as the main summative indicator while completing tables A and B in the proposed project. In Table A, the primary evidence articles will be documented, in particular, such issues as research design, hypotheses, theoretical foundation, findings, recommendations, and the level of evidence.
Table B will include brief descriptions of systematic reviews: research questions, search strategy, inclusion and exclusion criteria, analysis, and implications. As for the formative criterion, children’s attitudes to potential behavioral change will be evaluated, and the combination of indicators will make sure that the review will be valid and reliable. The interval and continuous data will be gathered; extraneous variables will be controlled by documenting and evaluating their impact, and statistical data will not be utilized.
Discussion and Implications for Nursing and Healthcare
Many overweight children believe that they have poorer health than their non-overweight friends and are concerned about their health. However, they do not use physical activity and sports as a structured practice like physical education lessons (Seburg et al., 2015). The implications are likely to promote awareness in children that daily activities such as walking or cycling to school as an important aspect of an active lifestyle (Broccoli et al., 2016). The training and sessions used in this study can be applied in clinical settings. Limitations, biases, validity threats, and the impact of the project on both the local and national levels will be discussed.
Plans for Dissemination
The findings obtained in the course of the proposed project will be disseminated in professional and institutional communities. First of all, the results will be demonstrated to other nurses to share ideas on how the current practice of child obesity management may be improved. I will present my results by publishing it in the academic journal titled Childhood Obesity or the International Journal of Obesity within 1 year after research, which will contribute to the existing theoretical knowledge in the given field. The regional conferences may be another beneficial platform for disseminating the project results among students and scholars. Further prospects in the examination of the given topic are to be specified as a part of the study dissemination.
Summary and Conclusion
To conclude, it is essential to emphasize that this paper is a proposal of the project on MI as a way to engage children in obesity prevention practices. The significance of the problem is associated with rapidly growing overweight and obese children, which causes such diseases as diabetes, cardiovascular issues, and so on. Therefore, a relevant PICOT question was formulated, project description was prepared, and potential outcomes were identified. It is expected to contribute to nursing practice by enhancing current child obesity prevention efforts.
References
Amiri, P., Kazemian, E., Mansouri-Tehrani, M. M., Khalili, A., & Amouzegar, A. (2018). Does motivational interviewing improve the weight management process in adolescents? Protocol for a systematic review and meta-analysis. Systematic Reviews, 7(1), 178-186.
Bean, M. K., Powell, P., Quinoy, A., Ingersoll, K., Wickham III, E. P., & Mazzeo, S. E. (2015). Motivational interviewing targeting diet and physical activity improves adherence to paediatric obesity treatment: Results from the MI Values randomized controlled trial. Pediatric Obesity, 10(2), 118-125.
Bonde, A. H., Bentsen, P., & Hindhede, A. L. (2014). School nurses’ experiences with motivational interviewing for preventing childhood obesity. The Journal of School Nursing, 30(6), 448-455.
Borrelli, B., Tooley, E. M., & Scott-Sheldon, L. A. (2015). Motivational interviewing for parent-child health interventions: A systematic review and meta-analysis. Pediatric Dentistry, 37(3), 254-265.
Broccoli, S., Davoli, A. M., Bonvicini, L., Fabbri, A., Ferrari, E., Montagna, G.,… Candela, S. (2016). Motivational interviewing to treat overweight children: 24-month follow-up of a randomized controlled trial. Pediatrics, 137(1), 1-12.
Brown, C. L., Halvorson, E. E., Cohen, G. M., Lazorick, S., & Skelton, J. A. (2015). Addressing childhood obesity: Opportunities for prevention. Pediatric Clinics, 62(5), 1241-1261.
Christie, D., & Channon, S. (2014). The potential for motivational interviewing to improve outcomes in the management of diabetes and obesity in paediatric and adult populations: A clinical review. Diabetes, Obesity and Metabolism, 16(5), 381-387.
Christison, A. L., Daley, B. M., Asche, C. V., Ren, J., Aldag, J. C., Ariza, A. J., & Lowry, K. W. (2014). Pairing motivational interviewing with a nutrition and physical activity assessment and counseling tool in pediatric clinical practice: A pilot study. Childhood Obesity, 10(5), 432-441.
Dawson, A. M., Brown, D. A., Cox, A., Williams, S. M., Treacy, L., Haszard, J.,… Taylor, R. W. (2014). Using motivational interviewing for weight feedback to parents of young children. Journal of Paediatrics and Child Health, 50(6), 461-470.
Finkelstein, E. A., Graham, W. C. K., & Malhotra, R. (2014). Lifetime direct medical costs of childhood obesity. Pediatrics, 133(5), 854-862.
Gorin, A. A., Wiley, J., Ohannessian, C. M., Hernandez, D., Grant, A., & Cloutier, M. M. (2014). Steps to growing up healthy: A pediatric primary care based obesity prevention program for young children. BMC Public Health, 14(1), 72-82.
Hung, L. S., Tidwell, D. K., Hall, M. E., Lee, M. L., Briley, C. A., & Hunt, B. P. (2015). A meta-analysis of school-based obesity prevention programs demonstrates limited efficacy of decreasing childhood obesity. Nutrition Research, 35(3), 229-240.
Mallonee, L. F., Boyd, L. D., & Stegeman, C. (2017). A scoping review of skills and tools oral health professionals need to engage children and parents in dietary changes to prevent childhood obesity and consumption of sugar‐sweetened beverages. Journal of Public Health Dentistry, 77, 128-135.
Natale, R. A., Messiah, S. E., Asfour, L., Uhlhorn, S. B., Delamater, A., & Arheart, K. L. (2014). Role modeling as an early childhood obesity prevention strategy: Effect of parents and teachers on preschool children’s healthy lifestyle habits. Journal of Developmental & Behavioral Pediatrics, 35(6), 378-387.
Ogden, C. L., Carroll, M. D., Lawman, H. G., Fryar, C. D., Kruszon-Moran, D., Kit, B. K., & Flegal, K. M. (2016). Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA, 315(21), 2292-2299.
Resnicow, K., McMaster, F., Bocian, A., Harris, D., Zhou, Y., Snetselaar, L.,… Hollinger, D. (2015). Motivational interviewing and dietary counseling for obesity in primary care: An RCT. Pediatrics, 135(4), 1-11.
Seburg, E. M., Olson-Bullis, B. A., Bredeson, D. M., Hayes, M. G., & Sherwood, N. E. (2015). A review of primary care-based childhood obesity prevention and treatment interventions. Current Obesity Reports, 4(2), 157-173.
Sim, L. A., Lebow, J., Wang, Z., Koball, A., & Murad, M. H. (2016). Brief primary care obesity interventions: A meta-analysis. Pediatrics, 138(4), 1-13.
Wang, Y., Cai, L., Wu, Y., Wilson, R. F., Weston, C., Fawole, O.,… Chiu, D. T. (2015). What childhood obesity prevention programmes work? A systematic review and meta‐analysis. Obesity Reviews, 16(7), 547-565.
Zhou, Y. E., Emerson, J. S., Levine, R. S., Kihlberg, C. J., & Hull, P. C. (2014). Childhood obesity prevention interventions in childcare settings: Systematic review of randomized and nonrandomized controlled trials. American Journal of Health Promotion, 28(4), 92-103.
Appendices
Legend:
- Level I: systematic reviews or meta-analysis.
- Level II: well-designed Randomized Controlled Trial (RCT).
- Level III: well-designed controlled trials without randomization, quasi-experimental.
- Level IV: well-designed case-control and cohort studies.
- Level V: systematic reviews of descriptive and qualitative studies.
- Level VI: single descriptive or qualitative study.
- Level VII: opinion of authorities and/or reports of expert committees.