Background Information
Developed technological know-how directly relates to better-quality patient outcomes and safety. The use of upgraded technology in hospitals and healthcare facilities is growing significantly. Researchers predict an upsurge in global data to 44 zettabytes, with 80% being unstructured while 60% duplicating the original information (Mohamed, 2017, p. 4). The figures depict a massive increase in the expected use of technology in organizations such as hospitals. Amid the COVID-19 pandemic, most institutions’ operations were interrupted due to social distancing and observing the Coronavirus rules and regulations.
Most organizations have permanently terminated their employees’ employment contracts and even other organizations such as Upwork resort to working from home. According to Donthu and Gustafsson (2020), the pandemic’s effects are not only felt in the economy but also in society, resulting in dramatic changes in how businesses operate and consumers behave (p. 284). The reduced number of patients depicts the shift in hospitals’ preferences. Similarly, the increased number of outpatient visits reveals a change in the perception of people. Consequently, increased calls for additional physical and human capital and drastic use of waiting bays depict the pandemic’s impact on hospitals.
Learning Outcome
Identify and summarize the impacts of COVID-19 on patient behavior and outpatient attendance.
Demonstrate knowledge about the significance of the proposed change in the field of nursing.
Demonstrate the significance of digital transformation in the hospital to manage the shift of patient behavior and strain on the available resources such as the waiting bay.
Demonstrate and outline the importance of the Virtual Visit application in managing patient-to-physician interaction amidst the COVID-19 pandemic.
Problem Statement
The novel coronavirus has impacted hospitals and healthcare facilities, leading to increased strain on limited available resources and increased outpatient visitations. With the current COVID-19 situation and the recent apparent health statistics in Medicare, there is an escalation of outpatients by 9%, resulting in increased physical and human capital and the utilization of waiting rooms (Innovation Digital Technologies, 2020, p. 2). Furthermore, 56% of patients in rural areas are deprived of healthcare services and are vastly underserved (Innovation Technologies, 2020, p. 2). Averagely, it takes approximately two hours to have an in-person appointment and a minimum of six days to get an in-person appointment for an outpatient visit. As a result, the delivery of healthcare services has been considerably delayed, impacting patient safety. When the waiting duration for appointments is prolonged, patients may encounter adverse health outcomes and are usually left to utilize the emergency department resources (Ansell et al., 2017, p. 1). Consequently, patient satisfaction is increased when waiting durations are minimal and non-existent (Ansell et al., 2017, p. 6). Proper handling of the sick is vital in improving the general experience of care in the hospital.
Consequently, in observing COVID-19 protocol and safety measures, the number of patients coming to hospitals has reduced significantly. Moreover, patients fear coming down to Medicare facilities to limit their interaction with people, an increase in interactions raises the chances of contracting the virus (Centers for Disease Control and Prevention, 2021). As a result, patients choose to stay at home despite being faced with severe health complications that might impact their quality of life. Appendix E, Figure 1, illustrates hospital attendance before the implementation of EHealth Virtual Application System Software.
PICO Components
Problem
The number of patients coming to the hospital has reduced significantly due to the COVID-19 virus. Patients fear contracting the Corona due to high interaction between individuals in a hospital environment. As a result, there is a need for additional physical and human capital and increased utilization of patients waiting for bays to observe social distancing.
Intervention
The company has resorted to investing in digital transformation and calls for organizational change.
Comparison
Comparison is made between the periods when the company does not invest in digital transformation and when digital transformation is adopted.
Outcome
There will be an increased patient turnout and decreased duration in acquiring in-patient appointments due to the launched change. The second outcome will be reduced calls for human and physical capital utilization and utilization of waiting rooms.
Proposed Solution
Transformation is important and cannot be avoided in an organization, especially when challenges affecting organizational performance arise. Change denotes an act or a process through which a different operation is initiated in a company (Achuor, 2014, p. 5). Several influential individuals describe the process of change as significant and an action whose timing has reached. The USA’s former president once said, “Transformation will not be possible if we wait for other individuals, or if we wait for another time to arrive. We are the change we seek” (Achuor, 2014, p. 6). Guided by the same spirit, the company has decided to invest more in digital transformation, shifting from face-to-face interaction as a form of developmental change. The company views the present situation as the right time to implement such changes due to the COVID-19 pandemic. See Figures 1 and 2 in appendix A for the previous strategy and the proposed change solution.
The Purpose for Change Strategy
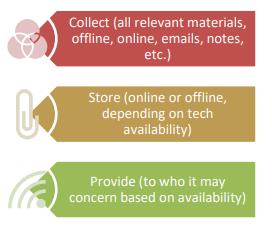
The company has resorted to investing in a more digital transformation and calls for its transformation. COVID-19 pandemic is a quick reminder that pandemics and catastrophes will continue to occur in the future (Donthu and Gustafsson, 2020, p. 284). The company has adopted the strategy to reduce the duration taken for in-patients to receive appointments and the time taken to acquire in-patient appointments for outpatient visits. Consequently, the number of patients visiting healthcare facilities has reduced due to fear of COVID-19 infection. As a result, the company has resorted to investing in digital and organizational transformations. The move will enable virtual interactions between patients and virtual medication provision, lowering the virus’s risk (Appendix B, Figure 1).
Benefits of the Proposed Solution
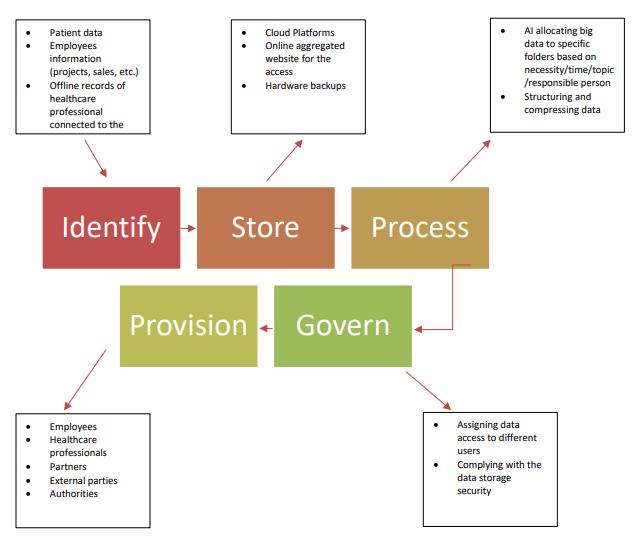
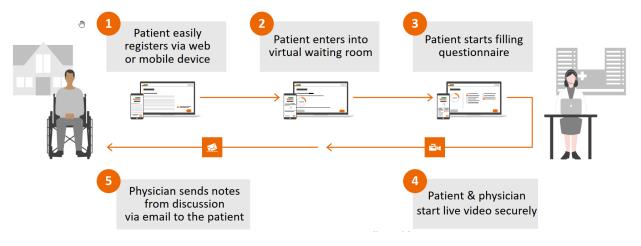
Based on the new solution, the company can separate the data flow and rely on online software to tackle massive data such as the cloud. Also, the proposed solution is to equip the company with artificial intelligence that processes and aggregates information and has simulation technology that provides information, security services for the cloud, and other linked aspects (The digital wave, n.d.). Such measures will assist the organization in processing data in an effective and structured manner. Virtual visit applications significantly influence healthcare delivery, patient care experience, and cost as there are huge demand and an increasing shift from in-patient to outpatient visits.
Evidence from Workplace and Literature
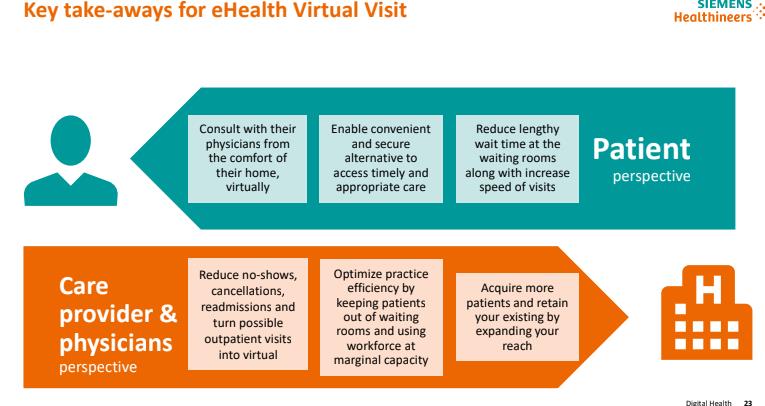
According to The digital wave (n.d), about 43% of outpatient visitation can be shifted to virtual delivery. As a result, Medicare professionals will easily expand outpatients’ services and bend the cost curve through the addition of capacity and provision of subsidized setting care. Similarly, The digital wave (n.d) suggests that due to traveling and transportation issues, 62.6% preferred virtual visits over face-to-face interactions since it is convenient, reduces the time of travel, is stress-free, and is less expensive. Virtual visits are expected to be on the rise in 2020 by 36 million (The digital wave, n.d). Consequently, according to The digital wave (n.d), virtual visits will increase patient satisfaction by 97% due to decreased lengths and peaked speed of visits. Increased patient satisfaction will result in increased patient safety and patients’ experience of care. The virtual application enables physicians to handle routine medical issues remotely, evaluate adverse cases in time, minimize the harm of delays, and reduce the risk of viral exposure in patients and physicians. Appendix D, Figure 1, depicts the key-take away of electronic health visits.
Measurement of the Proposed Change
The proposed change (Virtual Visit Application) will be measured for success in two forms. First and foremost, it will be evaluated based on practicability, impact on staff, and requirements in carrying out daily tasks. Secondly, the developmental change will be assessed based on personal progress utilizing Prosci’s AKDAR model:
- Awareness of the needed developmental change.
- Desire to contribute to and support developmental change.
- Knowledge of how to change.
- Ability to implement the much-needed behavior and skills.
- Reinforcement to support the developmental change.
The proposed developmental change will be measured according to the cumulative progress, meaning the evaluation centered on the single transition’s cumulative impact using human elements established by Prosci (SUP). Thus, the proposed change will be based on the following three aspects:
- Speed of adoption – How fast are physicians and patients adhering to the transformation?
- Utilization – The number of nurses and patients using the proposed developmental transformation?
- Proficiency – How efficient and effective are physicians and patients in the usage of the developmental transformation?
Method of Communicating the Proposed Change and Implementation Plan
The developmental change strategy is to be communicated using Kotter’s eight stages model. The company will employ Kotter’s model to ensure minimal resistance and obstacles that might arise while implementing the proposed change. Basing reference on Kotter’s model, the company will first create urgency to show others the need and importance of the transition using valid data and information. After creating urgency, the process will proceed to the second stage, constructing the guiding squad. Coming up with the guiding crew ensures the company establishes a group qualified to guide the transition process. Also, the second phase will focus on creating team functions. Under team function, the company will set clear and simple goals, brainstorm on methods, and challenge members to produce the best alternative possible. Upon completing the second stage, the company will create a vision and strategies to guide the process. Communication on the visions and strategies of the change will be made to enable understanding and buy-in. Other procedures to follow will be to empower action, establish short-term gains, build on the change, and make the change stick.
Human Factors Related to Change and Resistance to Change
During the implementation of change, the success of the transition is vital to an organization. Several factors may result in a transformation not being successful such as opposition to transformation. According to Achuor (2014), resistance to transformation may arise due to poor understanding of the proposed solution, disagreeing with how change should be implemented, and poor appreciation of the need to change (p. 13). Resistance to change has been a serious concern within the research society for decades and is proven to be the primary cause of failure in change initiatives (Amarantou et al., 2016, p. 23). Other factors resulting in resistance include predicting a lack of enough resources to support the change, lack of trust in an individual or organization, an embarrassment in admitting what is being done, and further improvement.
Staff Behavior Before and During Change
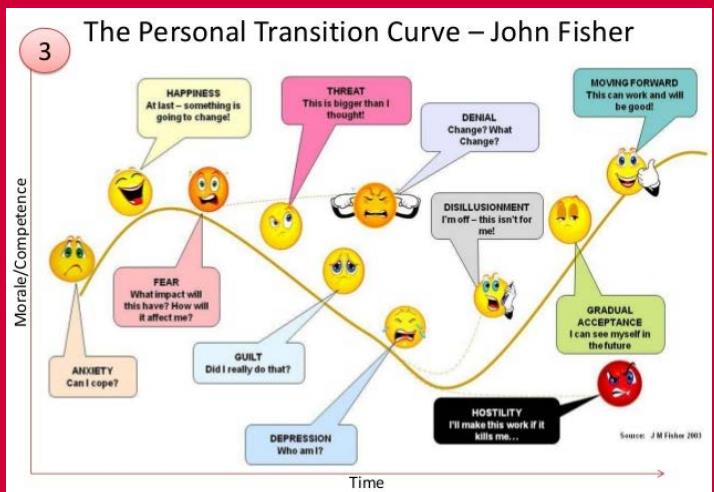
Several uncertainties normally arise in individuals when faced with a proposed change in an organization, as illustrated in the unique transition curve by John Fisher. The curve depicts several human behavior and attitude when faced with change that needs to be adopted. Appendix C, Figure 1, illustrates the personal transition curve by John Fisher. During and before the digital transformation process change, several types of staff behavior were noticed. Observed behavioral attitudes varied from one staff to another ranging from fear, denial, guilt, depression, threat, and gradual acceptance. Employees revealed fear of losing their jobs, with some expressing their concern that the recent change efforts in minimizing data processing duration imply less staff will be needed. Gradual acceptance occurred because some of the staff members were not aware of the vision of the change. As a result of explaining the visions to them, some embraced the change with time. Due to fear of losing their jobs after the change, depression was major in many semi-skilled employees.
Overcoming Resistance to Change
In overcoming human aspects related to change and resistance to the change strategy, the organization intends to ensure individual concerns about the change are discussed. Some of the company’s mitigating actions in addressing human factors related to change and resistance to change will include soliciting employees, providing f rewards and incentives, identifying new behaviors to augment the change, and prioritizing work based on available resources. To prevent resistance to the developmental changes during the transformation process, the administration and the guiding team need to ensure individuals affected by the change are involved in the decision-making process. During the proposed developmental change, employees’ attitude is primarily determined by their feelings and thought about the transformation. Human aspects associated with change might prevent successful transformation change; thus, there is a need to address them as they arise.
Reference List
Amarantou, V. et al. (2016) ‘Factors affecting “resistance to change”: an explanatory study conducted in the healthcare sector’, International Journal of Strategic Innovative Marketing, 16(40), pp. 1-40. doi: 10.15556/IJSIM.03.03.003
Ansell, D. et al. (2017) ‘Interventions to reduce wait times for primary care appointments: a systematic review’. BMC health services research, 17(295), pp. 1-9.
Centers for Disease Control and Prevention (2021) Older Adults and COVID-19.
Donthu, N. and Gustafsson, A. (2020) ‘Effects of COVID-19 on business and research’, Journal of Business Research, 117, p. 284. doi: 10.1016/j.jbusres.2020.06.008
Mohamed, A. (2017) ‘Digital transformation makes data management top priority’, CIO. Web.
The digital wave – how it impacts data management (n.d). Web.
Appendix A
Appendix B
Appendix C
Appendix D
Appendix E