Introduction
Efficient linen management in the healthcare sector contributes to quality patient care. Linen affects the healthcare aspects of hygiene, comfort and environment.
- The Bible in Leviticus recognizes linen as a possible carrier of infections and directs priests on how to manage contaminated linen (New Living Translation, 2004, Lev 13:47-59).
- Hospitals with better linen management processes eliminate wastage while promoting overall patient outcomes. On the flip side, healthcare facilities with poor linen management policies struggle with high linen wastage as they lack accounting systems for the stocks they procure.
Thesis Statement
Proper inventory management practices coupled with a lean management practice would significantly reduce linen wastage in healthcare.
Process Flow Analysis
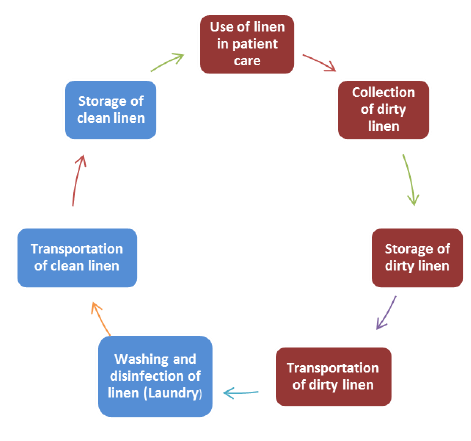
- Use of Linen. Clean linen is received from the store and used in patient wards. Each ward has a designated storage and sortation room for linen.
The storekeeper and the nurses in charge of the ward facilitate this process. - Dirty Linen Collection. All the used linen is collected for disposal or cleaning.
Soiled, used, and infectious lines are all collected as a hygiene observation practice. - Dirty Linen Storage. All the dirty linen collected must be stored, awaiting sorting and processing.
Every ward should have a storage area for soiled linen. - Dirty Linen Transportation. Once the dirty linen is sorted into groups, they are transported to the laundry for cleaning.
Different linen should remain separated during transportation to eliminate the need for sorting in the laundry. - Washing, Disinfection and Ironing of Dirty Linen. The linen is washed by the laundry staff at the laundry.
- They are also disinfected, ironed, and finally sorted in readiness for transportation and storage.
- Some hospitals wash their linen while others outsource the services to a third-party player.
- Clean Linen Transportation. Clean linen is transported to the special rooms attached to every ward for storage.
- Clean Linen Storage. This is the last step in the linen management process, where clean linen is received for storage in readiness for use.
Waste Identification
- Staff using more linen. A recent audit showed that patients were using more linen than required.
- It means the hospital must procure more than necessary every other time due to a false shortage.
- Some beds have been found with more than two bedsheets, while most have two pillows, yet one bed serves one patient.
- Disposal of reusable linen. It was also discovered that some linen that could still be used was being disposed of.
This stems from a lack of concern and inadequate education of staff on lean wastage reduction practices. - Patients leave with linen. There have also been reports that some patients might be going with hospital linen on discharge due to weak security mechanisms.
Stakeholders
- Management. The management is a crucial stakeholder in linen management that coordinates and oversees all the processes.
- The administration makes critical decisions that impact linen management; thus, its involvement is vital.
- Laundry Staff. The laundry staff facilitates the washing, disinfection and ironing of linen.
- They are instrumental in ensuring that all linen received at the laundry section is accounted for, providing a necessary check to waste management.
- In addition, if the management outsources linen management, they will be the most affected.
- Nurses. They are in charge of wards and patients hence understanding the life cycle of linen in the hospital.
- They change linen when necessary providing a vital link between storage, usage and collection.
- Besides, nurses play a critical role in the patient discharge process and could help ensure no linen leaves the ward during discharge.
- Storekeepers. They keep an inventory of dirt from the wards and clean linen from the laundry.
- Storekeepers are better placed to identify system failures that could be addressed to eliminate waste.
- They will also be affected in case the hospital digitizes linen inventory management.
Identified Barriers
- Manual tracking. The main barrier to addressing the current linen wastage stems from the current manual tracking system.
- An automated inventory system using RFID technology is necessary to ensure that every linen is tracked and accounted for to reduce wastage and enhance efficiency (Ramasamy & Hassan, 2018).
- There is also the need to adopt lean management practices by the hospital to enhance efficiency.
- Policy. The in-house system of managing linen is laced with several leaks and flaws that should be addressed through a policy change. The current staff is ill-prepared to handle linen, while some lack knowledge of reducing waste properly.
- A professional body would help minimize linen waste and improve overall quality, thus outsourcing linen management (Arisi-Nwugballa, 2016).
Potential Savings
- Elimination of waste. The automation of linen management and the adoption of lean management would significantly reduce linen wastage and thus save the hospital costs invested in buying unnecessary linen (Fitriasari et al., 2018).
- Laundry staff hiring costs. Outsourcing linen management will cut costs currently used by the hospital to maintain laundry staff.
Conclusion
- Incorporating information technology systems and adopting lean management practices in linen management could help reduce wastage.
- The critical processes in linen management that should benefit from the changes include storage, laundry and usage.
- The process should involve all the stakeholders, including nurses, laundry staff, storekeepers and the management.
References
Arisi-Nwugballa, E. A. (2016). Does outsourcing improve the quality of service in public health care institutions in South-East Nigeria? International Journal of Academic Research in Accounting, Finance and Management Sciences, 6(2), 196-203.
Aucamp, M. (2016). Housekeeping and Linen Management.
Fitriasari, N., Haryanto, T., & Yuliansyah, N. (2018). Reducing Linen Loss in Hospital Using Lean Six Sigma Approach. KnE Life Sciences, 199-206. Web.
Ramasamy, S. K., & Hassan, S. (2018). Radio Frequency Identification (RFID) Adoption in Healthcare Linen Management: A Case study at ProLinenCare. Global Business Management Review, 10(1), 47-65.
Holy Bible: New Living Translation. (2004). Wheaton, Ill: Tyndale House Publishers.