A concept map is a graphical tool for the organization and presentation of information, which helps to present the relationship between the event and different factors and to display the interaction of several elements vividly (Anderson, Day, & Vandenberg, 2011). In this paper, the concept map reflects the factors that may prevent the implementation of the practicum project and the relationship between different aspects.
The overall aim of the project is to determine strategies that can be executed to diminish the door-to-balloon time in the STEMI patients at Kendall Regional Medical Center (KRMD). As per the evidence analysis, the period between presentation at the hospital and the door-to-balloon time during primary PCI (Percutaneous coronary intervention) should not exceed 90 minutes while earlier intervention leads to better patient outcomes (Ellahham, Aljabbari, Mananghaya, Raji, & Zubaidi, 2015). However, certain external issues can interfere with the successful realization of this strategy. Figure 1 briefly reflects on them:
According to the concept map, the main factor that may significantly affect the implementation of the strategy is the lack of or insufficient funding for the organization by the government. For KRMD to be able to implement this approach, the government should provide financial and other support to the medical center for the training of its personnel and supply ambulances with the necessary equipment and supplementary materials.
If the state does not support the health care institution, KRMD will not have an optimum pre-hospital system for STEMI patients (Fergusson, Spies, Hong, Young, & Beauvallet, 2012). One of the important aspects of the insufficient financing is the inability of the company to provide its paramedics and EMS operators with protocols and to train them in the pre-hospital fibrinolysis and reperfusionstrategy, which is an essential part of the proposed solution (American College of Cardiology Foundation & American Heart Association, 2013).
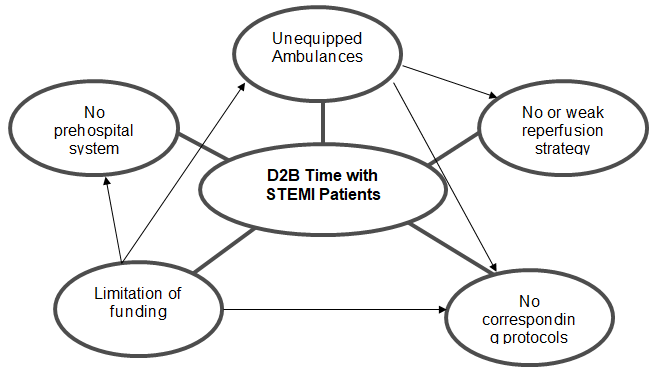
Emergency medical services are financed from the state budget, and the implementation of the new strategy requires significant investment in equipment and communications. Also, the presence or lack of equipment and supplementary forms suggests that the state does not cooperate with suppliers effectively, which could negatively affect the experience and anticipations of the stakeholders.
Furthermore, in conditions as sharp as STEMI and stroke, patients require immediate medical attention; the absence of comprehensive strategy will lead to the situation when the care providers cannot furnish a timely aid to patients (Wilson et al., 2013). In this regard, regional health authorities can facilitate the implementation of pre-hospital strategies. It will enforce higher integration with hospital services, which in turn, will assist in reducing the time of reperfusion.
According to the Lean concept, all stakeholders involved in the care provider should be empowered and subsequently, take active roles in improving quality (Lawal et al., 2014). Every nurse and physician should be vigilant to identify and address poor quality services and waste that lead to longer D2B time. However, there are external factors that can significantly complicate or postpone the implementation of the strategy to reduce the door-to-balloon time in the STEMI patients at Kendall Regional Medical Center. Consequently, the company should determine the exterior obstacles and reconsider its strategy to refine and remove the barriers that prevent the best clinical outcomes.
References
American College of Cardiology Foundation & American Heart Association. (2013). 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. Circulation, 127(1), e362-e425.
Anderson, L., Day, K., & Vandenberg, A. (2011). Using a concept map as a tool for strategic planning. Preventing Chronic Disease, 8(5), A117.
Ellahham, S., Aljabbari, S., Mananghaya, T. H., Raji, S. J., & Zubaidi, A. A. (2015).
Reducing door to-balloon-time for acute ST elevation myocardial infarction in primary percutaneous intervention: Transformation using robust performance improvement. BMJ Quality Improvement Programme, 4(1), 1-4. DOI:10.1136/bmjquality. u207849.w3309.
Fergusson, D., Spies, C., Hong, R., Young, C., & Beauvallet, S. (2012). Door-to-balloon time in acute ST segment elevation myocardial infarction. Hawaii Journal of Medicine & Public Health, 71(11), 320–323.
Lawal, A., Rotter, T., Kinsman, L., Sari, N., Harrison, L., Jeffery, C.,…Flynn, R. (2014). Lean management in health care: definition, concepts, methodology and effects reported. Systematic Review, 3, 103.
Wilson, B., Humphrey, A., Cedarholm, J., Downey, W., Haber, R., Kowalchuk, G.,… Garvey, L. (2013). Achieving sustainable first door-to-balloon times of 90 minutes for regional transfer ST-segment elevation myocardial infarction. JACC: Cardiovascular Interventions, 6(10), 1064-1071.