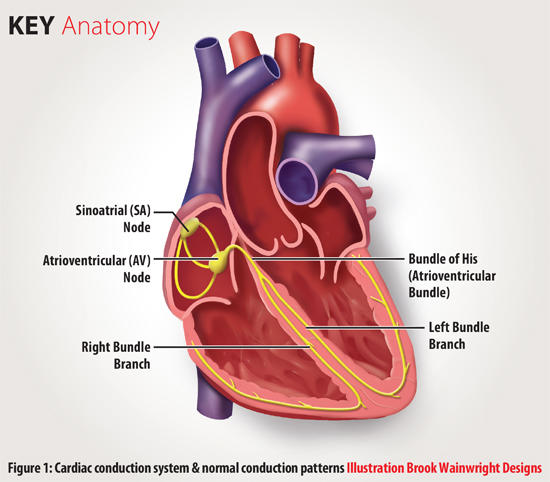
The human heart is exposed to many health problems related to impairments in the cardiac conduction system. The heart contracts under the control of the electrical signals or impulses. The normal cardiac conduction system involves the sinoatrial (SA) node, the atrioventricular (AV) node, and the bundle of His (Brown, Brywczynski, McKinney, & Slovis, 2014). The normal heartbeat begins when the electrical signal is initiated by the SA node, which is the natural pacemaker located in the upper right atrium. The signal travels through the atria to reach the AV node. According to Brown, Brywczynski, McKinney, and Slovis (2014), the AV node helps in synchronizing the pumping action of both the atria and the ventricles. After crossing the AV node, the signal passes through the bundle of His and then divides into branches that extend into the left and right ventricles. The electrical signal further travels down the branches to reach the ventricular cells causing them to contract. As a result, blood is pumped to different parts of the body.
Types of Heart Blocks and their Appearance on the ECG
First-degree heart block
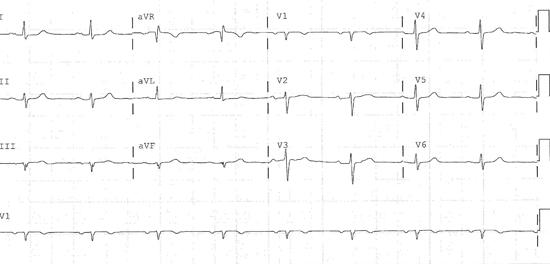
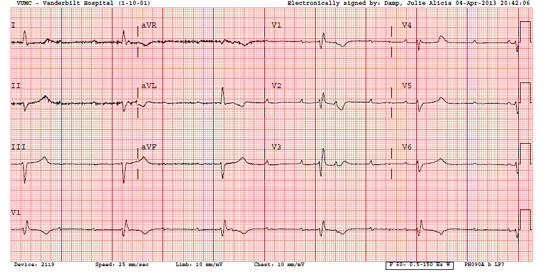
In this type, electrical impulses slow down when passing through the conduction system despite reaching the ventricles successfully. The delay in conduction occurs in the atrium, AV node, or the bundle of His (Brown, Brywczynski, McKinney, & Slovis, 2014). Sandesara (2014) explains that it is rare for first-degree heart block to cause symptoms. This type is common in athletes or individuals who take particular medications. This heart block does not require any form of treatment. On the electrocardiogram (ECG), this type of heart block manifests as prolonged PR intervals with durations exceeding 20ms (Brown, Brywczynski, McKinney, & Slovis, 2014). The prolongation remains constant with P waves preceding every QRS complex. Most of these blocks present with a narrow QRS complex, which shows that the block is in the proximal portion of the conduction system such as the AV node itself (Brown, Brywczynski, McKinney, & Slovis, 2014). Conversely, a minority of the first-degree hear blocks have a wide QRS to show that the block is in the distal portion of the conduction system.
Second-degree heart block type I
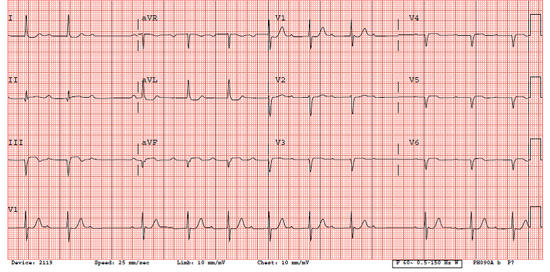
This type of heart block occurs when electrical signals are delayed more and more with every heartbeat to a level that a beat fails to reach the ventricles. This type is characterized by progressive lengthening of the PR interval that culminates in a dropped QRS complex (Brown, Brywczynski, McKinney, & Slovis, 2014). The site of the block occurs at or above the AV node resulting in the P wave and QRS complex having a normal morphology and duration. Initial heartbeats appear on the ECG with normal PR intervals, but subsequent beats manifest with progressively longer intervals to a level that the P wave fails to reach the ventricles causing depolarization.
Second-degree heart block type II
This heart block is severe than type I. Brown, Brywczynski, McKinney, and Slovis, 2014) explain that it occurs distal to the bundle of His, either in the branches or the common bundle. On the ECG, it is characterized by dropped QRS complexes or non-conducted P waves. The PR interval is constant with a widened QRS complex due to the associated bundle branch block although it may sometimes appear narrow (Brown, Brywczynski, McKinney, & Slovis, 2014). The dropped beats mostly occur at regular intervals.
Third-degree heart block
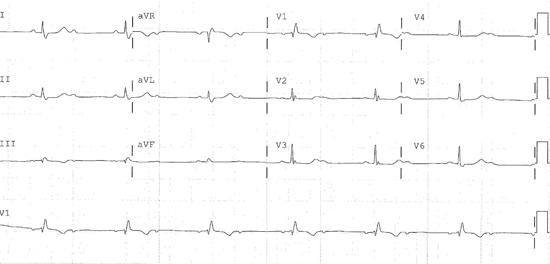
This type is a complete heart block with electrical signals from the atria failing to reach the ventricles completely. In this case, ventricles generate some impulses through a ventricular or junctional pacemaker (Brown, Brywczynski, McKinney, & Slovis, 2014). On the ECG, both the QRS complexes and P waves march regularly.
Treatment of Heart Block
Although first-degree heart blocks do not require any form of therapy, the other types may need medical intervention. Second-degree heart block may require an artificial pacemaker, which is mandatory for third-degree heart blocks (National Heart, Lung, and Blood Institute, 2012). A pacemaker is a small medical device used to monitor the heartbeat before sending electrical signals to excite the heart to beat at specific rates. The device is implanted under the skin on the chest and connected to the heart by either one or two leads passed through a vein. Sometimes, acquired heart blocks may disappear once the cause is removed. For instance, heart blocks that occur after surgery or a heart attack may disappear on recovery (National Heart, Lung, and Blood Institute, 2012). If medicines are the cause, the condition may stop occurring once the medication is stopped or its dosage is lowered to safe levels.
Summary
The heart carries the sole responsibility of pumping blood to different parts of the body under the control of the conduction system. Impulses are generated by the SA node of the right atrium. These electrical signals then travel through the AV node before reaching the bundle of His. Failure for these impulses to reach the ventricles in the usual way results in the occurrence of different types of heart block including first, second, and third-degree heart blocks. These types of heart blocks appear to present differently on the ECG. However, the use of pacemakers helps in treating both second and third-degree heart blocks.
References
Brown, A., Jeremy Brywczynski, J., Jared McKinney, J., & Slovis, C. (2014). How to recognize and treat heart block: A review for prehospital providers. Journal of Emergency Medical Services. Web.
National Heart, Lung, and Blood Institute (2012). How is heart block treated? Web.
Sandesara, C. M. (2014). Atrioventricular block. Medscape. Web.