Introduction
Johns Hopkins Hospital is one of the most recognizable health facilities in America. It is known for the diversity of medical services offered and a high number of patients who seek them. However, the daily operations of the hospital’s operations and the safeguard of its patients’ safety and quality standards are hinged on the proper management of its electronic health records (EHR) (Johns Hopkins Medicine, 2018b).
Therefore, efficient EHR management is part of the institutions quality management plan, which is designed to put the interests of patients first by making the hospital accountable for the delivery of high-quality healthcare services. This strategic goal aligns with its mission, which is to push the boundaries of discovery through transformation and innovation (Johns Hopkins Medicine, 2018d).
The alignment of Johns Hopkins quality improvement goals and vision stems from the tenacity of its quality improvement processes (Hickey & Brosnan, 2012). The strategic goal of the hospital’s quality improvement plan also aligns with its mission, which is to improve the standards of excellence in medical education, research and clinical care (Johns Hopkins Medicine, 2018d). Stated differently, an improvement in quality standards helps to elevate the hospital’s standard of excellence in the provision of quality care.
Lastly, Johns Hopkins Hospital is guided by four core values of excellence and discovery, leadership and integrity, diversity and inclusion as well as respect and collegiality (Johns Hopkins Medicine, 2018d). The strategic goals of the quality improvement plan support one core value – excellence.
Johns Hopkin’s quality improvement plan also supports the hospital’s quest to meet the requirements of several legal provisions influencing the safety of health services offered at the facility. For example, through continuous improvement in quality standards, the hospital is able to meet the requirements of the Patients Quality and Safety Improvement Act of 2005, which requires health workers to report issues involving patient safety that compromise the ability to provide quality health services (Sadeghi, Barzi, Mikhail, & Shabot, 2013).
The quality improvement plan also allows the organization to abide by quality standards provided by the Centers for Medicare and Medicaid, Agency for Healthcare Research and Quality, and Food and Drug Administration among other public health agencies that have a mandate to ensure quality standards are observed at the hospital (Sadeghi et al., 2013).
Current Situation – Quality Improvement
Johns Hopkins Hospital has a good record of quality standards. EHR management is a key part of its quality improvement plan because the hospital’s management has strived to make sure this aspect of quality performance aligns with national and international standards on the same. This is why the hospital’s EHR system (Epic) is internationally known and widely used in America (Johns Hopkins Medicine, 2018b).
The Epic system is considered a superior way of managing data in the healthcare sector because it allows service providers to monitor quality issues across a wide range of clinical areas (Johns Hopkins Medicine, 2018b). Through the implementation of this system, Johns Hopkins Hospital has received several awards for providing quality and holistic healthcare services. Some of them include “Top Performer on Key Quality Measures, Magnet designation for nursing, HomeCare Elite, and Delmarva Foundation Excellence Awards” (Johns Hopkins Medicine, 2018b, p. 1). The U.S. News and World Report have also ranked the hospital as a leader in the provision of quality healthcare services (Johns Hopkins Medicine, 2018b).
Measures and Indicators of Quality
Johns Hopkins Hospital has six key quality measures – patients’ experiences, infection prevention, core measures, surgical volumes, the quality of care ratings, and pediatrics (Johns Hopkins Medicine, 2018c). Patients’ experiences are evaluated based on survey data provided by patients who have received care at the facility (Johns Hopkins Medicine, 2018c). Data obtained in this way makes it possible for evaluators to compare current and future results.
Comparatively, “core measures” evaluates how well the facility complies with national and international standards of quality, while the quality of care ratings is an internal performance measure, which evaluates the hospital’s quality performance measures, such as ambulation (Johns Hopkins Medicine, 2018c).
The number of surgeries completed at the facility is also an important quality measure at Johns Hopkins Hospital because it undertakes periodic reviews of the number of surgical procedures undertaken and the wellness levels of the patients served (Johns Hopkins Medicine, 2018c). Infection prevention is also deemed an associated measure of quality at the facility. It refers to the procedures undertaken by health workers in controlling infections, such as washing their hands before and after surgical procedures (Johns Hopkins Medicine, 2018c).
Lastly, “Pediatrics” as a measure of quality at the facility is associated with national standards of treatment and may involve an analysis of how well patients receive care (such as pain management) or how much time they have to wait to receive health services (wait times) (Johns Hopkins Medicine, 2018c).
Presentation of Data
Johns Hopkins Hospital does not have a publicly accessible record of its quality performance. Furthermore, few independent agencies have documented historical records of the hospital’s quality standards. Consequently, most of the information available for review pertains to its ranking in quality awards, such as the Centers for Medicare and Medicaid Services’ five-star rating of quality performance, which gave the facility a three-star rating (Johns Hopkins Medicine, 2018a).
Associated methods that can be used to obtain institution-specific data relating to the hospital could include institutional surveys, an analysis of its administrative and billing records, as well as an analysis of medical records generated and used by health practitioners at the facility (Ernst et al., 2010). Data obtained in this way could be analyzed using software, such as the Statistical Packages for Social Sciences (SPSS) and Microsoft Excel. The software are useful for data analysis because they can review large quantities of data.
Methods for Collecting and Analyzing Data in the Future
The above-mentioned data collection and analysis strategies are more efficient than past techniques, which required the physical analysis of health records. Furthermore, they have enabled health professionals to analyze large quantities of data – an activity that was difficult to achieve in the past because of the manual processing of health information. In the future, the collection and analysis of data through mobile phones could become a preferred method of data collection because it is convenient to obtain data using personal gadgets.
The growth of smartphones, data collection applications, and text messaging techniques provide a promising range of platforms through which data collection using mobile phones could occur. The use of such techniques could significantly improve people’s understanding of quality performance at Johns Hopkins Hospital and other similar health facilities. However, the use of mobile phones in data collection and analysis is currently premature. Instead, they should be used at a time when an interface for merging personal and institutional data is developed.
Targets
Johns Hopkins Hospital has a good record of developing quality improvement initiatives. However, since this process is continuous, the organization needs to adapt to the healthcare environment and changing patients’ dynamics by setting new targets of quality improvement. The list below outlines realistic evidence-based targets that the institution could follow in improving its quality management plan.
- Reduce wait times by 5% annually through improved efficiencies in organizational processes for the next five years.
- Improve patients’ experiences by promoting cultural diversity in the healthcare setting through improved staff training.
- Improve the quality of care ratings by aligning institutional health processes to international quality standards.
Quality Improvement Strategies
Quality improvement strategies are often employed by different healthcare organizations to bridge patient safety and quality gaps (Institute of Medicine, 2001). They may involve numerous changes to organizational processes, such as variations in workflow processes, scheduling systems, and care structures, relative to available quality improvement and service tools (NHS Institute for Innovation and Improvement, 2010).
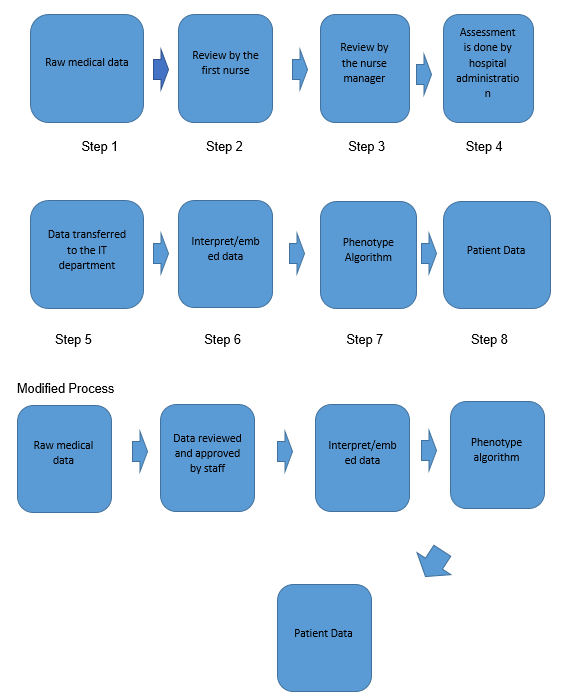
Eight key processes characterize the management of EHR data at Johns Hopkins Hospital. They include the generation of raw data, a review of statistics by a first nurse, a similar analysis of the same data by a nursing manager, an assessment of health information by hospital administrators, transfer of data to the information technology department, interpretation of statistics, its transformation to phenotype algorithm, and lastly the generation of patient data. These processes define the main characteristics of the Epic system, which is the main data management software for the hospital (Johns Hopkins Medicine, 2018b).
The lean value mapping technique is a useful tool for quality management at Johns Hopkins Hospital because its EHR management process contains several areas of redundancy. Cookson, Read, Mukherjee, and Cooke (2011) say the model is preoccupied with the elimination of non-value adding processes to improve system flows. Using the linear mapping tool, it is possible to simplify Johns Hopkins’ EHR management structure into five key steps – generation of raw data, staff approval, interpretation of information, a transformation of statistics by phenotype algorithm, and the generation of final patient data. Using the lean value stream mapping technique, the review of data by different cadres of staff has been minimized from three processes to one.
This proposal is supported by the possibility of integrating data analysis and review processes using a common platform that would integrate the input of nurses, their managers, and hospital staff. The process creates a common integrative framework that gives an opportunity to any of the three groups of medical staff to edit data transparently. Doing so reduces the probability of human error or data manipulation because there would be checks and balances made by other staff members whenever one of them modifies a piece of medical information.
Based on the reliance on the lean value stream technique to come up with the modified process map of Johns Hopkins’ EHR management, it is integral to point out that the major area of wastage identified in this review is the systematic editing of patient data by three sets of medical staff – nurses, their managers, and hospital staff. Instances of data overproduction are also identified in steps 2, 3, and 4 of the process map outlined in figure 1 because the same information is recorded severally.
Consequently, there are redundancies in data management because different members of staff review the data at different stages. Based on these areas of inefficiencies, value-added processes emerge through the seamless integration of the second, third, and fourth processes. Collectively, their functions are integrated into one seamless editing platform that amalgamates their contributions in the EHR data management process.
Figure 1, which is the process map, shows the initial and modified process maps. Collectively, it could be relied on to institute system-level changes in EHR management and minimize quality and safety performance gaps at Johns Hopkins Hospital.
Process Map – Management of EHR
References
Cookson, D., Read, C., Mukherjee, P., & Cooke, M. (2011). Improving the quality of emergency department care by removing waste using lean value stream mapping. International Journal of Clinical Leadership, 17(1), 25-30.
Ernst, M. M., Wooldridge, J. L., Conway, E., Dressman, K., Weiland, J., Tucker, K., & Seid, M. (2010). Using quality improvement science to implement a multidisciplinary behavioral intervention targeting pediatric inpatient airway clearance. Journal of Pediatric Psychology, 35(1), 14-24.
Hickey, J. V., & Brosnan, C. A. (2012). Evaluation of health care quality in advanced practice nursing. New York, NY: Springer Publishing Company.
Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century.
Johns Hopkins Medicine. (2018a). Patient safety and quality. Web.
Johns Hopkins Medicine. (2018b). Epic at Johns Hopkins medicine. Web.
Johns Hopkins Medicine. (2018c). Patient safety and quality. Web.
Johns Hopkins Medicine. (2018d). Johns Hopkins medicine strategic plan. Web.
NHS Institute for Innovation and Improvement. (2010). Quality and service improvement tools: Process mapping – An overview. Web.
Sadeghi, S., Barzi, A., Mikhail, O., & Shabot, M. M. (2013). Integrating quality and strategy in healthcare organizations. Burlington, MA: Jones & Bartlett Learning.