Introduction
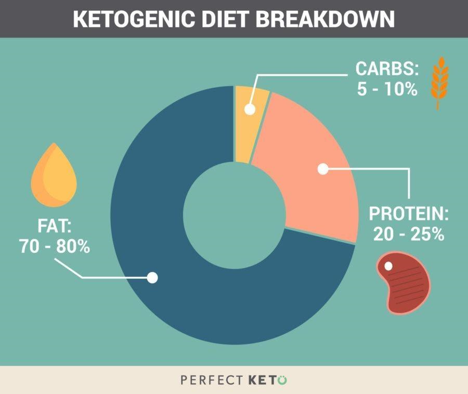
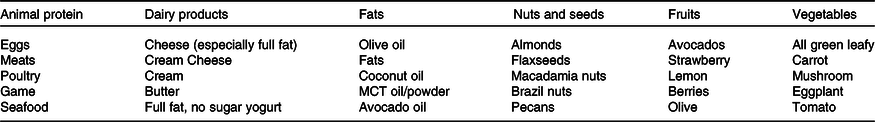
The ketogenic diet (KD) comprises high fat, low carbohydrate, and moderate protein. A standard KD encompasses about 70-80% fats, 5-10% carbohydrates, and 15-20% proteins (Zhu et al., 2021, p. 2). Some KD foods may include eggs, high-fat dairy products, seafood, and avocados (Ashtary-Larky et al., 2021, p. 1900). However, individuals adhering to this diet often avoid starchy vegetables, grains, fruits, and high-sugar foods.
The KD deprives the body of carbohydrates, resulting in fat metabolism in a process called ketogenesis. This leads to the production of ketones used as a primary fuel source rather than glucose. This metabolic state is known as ketosis and is characterized by the presence of acetone, β-hydroxybutyrate, and acetoacetate, which meet the body’s energy demands. In this case, the need for KD has been driven by various factors, especially its health benefits.
The diet was initially developed to treat refractory epilepsy among young children. Nevertheless, the recent existence of multiple studies linking KD to treating numerous chronic illnesses such as obesity, diabetes, cancer, and neurodegenerative disorders has considerably increased its demand. Another element that has led to the need for KD is the increased health awareness among individuals, as more people wish to adopt healthy diets and lifestyles.
KD has several benefits, including weight loss, which is critical in obesity management. In this case, the low-carbohydrate diet and suppressed appetite reduce body weight, blood glucose, and cholesterol levels among obese individuals. In addition, carbohydrate restriction significantly lowers glucose concentration and glycated hemoglobin, assisting individuals with type 2 diabetes to effectively regulate their blood glucose without needing insulin.
Similarly, KD helps in cancer management by suppressing the growth of cancer cells, which are highly reliant on glucose for development. Since the tumor cells have severe mitochondrial defects, they cannot use ketones as energy sources, resulting in metastasis inhibition while ensuring the efficient functioning of the normal cells. Equally, KD lessens triglyceride and cholesterol levels, lowering the risk of cardiovascular diseases.
KD significantly improves oxidative stress and mitochondrial dysfunction, which are the primary triggers for most neurodegenerative diseases such as epilepsy and Alzheimer’s disease. The diet also enhances insulin sensitivity and decreases insulin levels, lowering the incidence of polycystic ovary symptoms among women. Not to mention, KD reduces inflammation, which helps to treat acne issues and has anti-aging effects.
However, on the downside, KD has multiple adverse effects, such as the ‘keto flu,’ which is characterized by nausea, fatigue, headache, dizziness, irritability, and vomiting. Additionally, KD causes severe nutritional deficiencies due to the lack of critical minerals, vitamins, and fiber, predisposing individuals to impaired immune systems. It also exposes individuals to chronic complications due to the high fat content.
The diet may cause congenital disabilities; hence, it is not recommendable for women during the pre-pregnancy and pregnancy periods. Other diets opposed to KD include the Zone, Paleo, Mediterranean, and South Beach. Although KD shows much potential as a therapeutic intervention for several health conditions, additional research is needed to prove its efficacy and safety for diverse populations.
Literature Review
Diet as a treatment approach has become integral today as the world continues to grapple with various chronic diseases. Exercising a healthy diet has been established as a key intervention toward preventing, delaying, and managing various health complications, including type 2 diabetes (Gropper, 2023, p. 664). As a result, there has been an increased need for individuals to modify their diets to avert or manage different ailments. The high demand for dietary modification has led to the prominence of low-carbohydrate diets, particularly the ketogenic diet, which shows great potential in treating multiple illnesses and improving individuals’ overall health outcomes.
Ketogenic Diet
In recent years, the adoption of the ketogenic diet, also known as the keto diet, has gained more prominence among different populations across the globe. KD is a high-fat, moderate protein, and extremely low carbohydrate diet (Zhu et al., 2021, p. 1; Zhou et al., 2022, p. 10429; Batch et al., 2020). The diet focuses on limiting the intake of carbohydrates to less than 25 to 50 grams daily (Li & Heber, 2020, p. 386; Crosby et al., 2021, p. 1; Batch et al., 2020). According to Li and Heber (2020), in a typical KD, only 5% of calories should come from carbohydrates, while 75% and 20% ought to be derived from fats and protein, respectively. These findings are supported by Zhu et al.’s (2021) study, which indicates that a keto diet comprises 70-80% fats, 5-10% carbohydrates, and 15-20% proteins (see Figure 1).
Some recommended KD foods include seafood, eggs, avocados, and high-fat dairy products (see Figure 2). Nevertheless, individuals practicing KD are advised to refrain from grains, fruits, starchy vegetables, rice, and pasta, among other sugar-containing foods and beverages.
Ketogenesis and Ketosis
The restriction of carbohydrates associated with KD results in changes in the body’s metabolism. Carbohydrate deprivation and glycogen depletion trigger the body to undergo an endogenous production of glucose from glycerol, lactate, and amino acids glutamine and alanine in a process called gluconeogenesis (Ashtary-Larky et al., 2022, p. 1900).
According to Batch et al.’s (2020) study, gluconeogenesis can only be maintained for three days for individuals engaging in a low-carbohydrate diet (LCD), necessitating the need for additional energy sources to meet the body’s demands. As a result, the ketogenesis process becomes indispensable for survival. Ketogenesis is a mechanism in which stored fats are oxidized, producing ketones, which are used as the primary fuel source instead of glucose (see Figure 3).
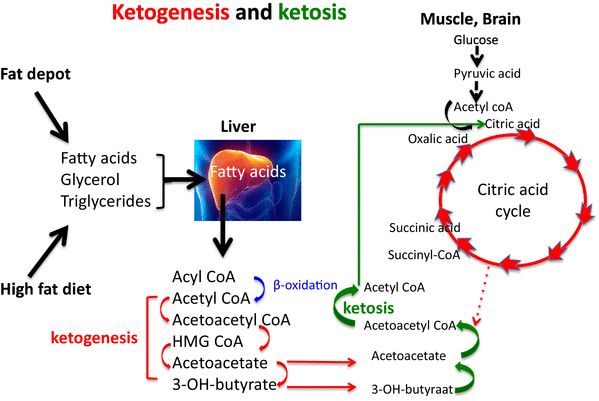
Ketogenesis results in ketosis, a metabolic state in the body characterized by significant levels of ketones. During ketosis, three types of ketone bodies, acetone, β-hydroxybutyrate, and acetoacetate, are formed and utilized by the body to meet its energy demands (Dowis & Banga, 2021; Merrill et al., 2020; Brouns, 2018, p. 1305). In this case, all cells containing mitochondria, such as the muscles and brain, can replenish their energy with ketone bodies.
Causes Leading to the Need for a Ketogenic Diet
Various factors have contributed to the need for the keto diet. Russel Wilder initiated the idea of KD in 1921 to manage refractory epilepsy among children (Gołąbek & Regulska-Ilow, 2022, p. 1; Zhu et al., 2021). Following its development, KD became a popular epilepsy treatment approach for almost a decade before the invention of antiepileptic drugs such as diphenylhydantoin.
Nevertheless, over the years, KD has again gained popularity, mainly due to its health benefits. In recent years, there have been surging cases of chronic health complications such as obesity, type 2 diabetes, cancer, and other neurological disorders. Hence, numerous studies linking KD to treating and managing these chronic disorders have increased demand for this diet (Li et al., 2022; Batch et al., 2020).
According to Ludwig (2019), another contributing factor to the extensive interest in KD is the increased health awareness among the masses (p. 1354). Individuals are increasingly becoming cognizant of the significance of adopting healthy lifestyles and diets. Thus, since KD provides a means for people to eat healthily while still enjoying high-fat foods and other delicacies, it has become a preferred diet for many.
Benefits of the Ketogenic Diet
The ketogenic diet, characterized by low carbohydrates, has been found effective in improving weight loss, which can help manage obesity. Compared to low-fat diets, KD is more effective in weight loss (see Figure 4).
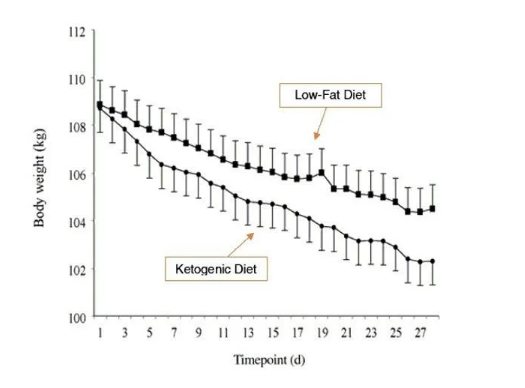
The KD diet reduces body weight, blood cholesterol, and body mass index (BMI), resulting in significant weight loss among obese individuals (Zhou et al., 2022, p. 10429; McGaugh & Barthel, 2020; Crosby et al., 2021). The weight loss is attributed to a decreased appetite due to the increased satiety impact of proteins or appetite suppression by the ketones, particularly the β-hydroxybutyrate (Ludwig, 2019, p. 1355). Additionally, the weight loss may be due to reduced lipogenesis caused by enhanced insulin resistance and heightened lipolysis.
Similarly, Zhu et al.’s (2021) research shows that high energy consumption from increased gluconeogenesis and heightened metabolic efficiency linked with saturated fat intake can result in weight loss. A 2022 study by Gołąbek and Regulska-Ilow further indicates that KD can enhance lipid markers, glycemic control, and glycated hemoglobin (HbA1c) levels among obese people, improving overall health. Thus, KD suppresses appetite and increases gluconeogenesis, leading to significant weight loss, which is critical in managing obesity.
Keto has become fundamental in diabetes management, resulting in positive health outcomes. Individuals with diabetes fail to utilize insulin properly, leading to fluctuations in their blood sugar levels. However, carbohydrate restriction, like in the case of KD, can considerably decrease the glucose concentration and HbA1c in the body, eliminating the need for insulin among people with type 2 diabetes (Dowis & Banga, 2021). In addition, Crosby et al.’s (2021) findings show that KD reduces appetite and promotes weight loss, thus aiding in diabetes management. This is because depressed appetite and significant weight loss help to improve obesity, a major risk factor for type 2 diabetes (Li et al., 2022; Zhou et al., 2022).
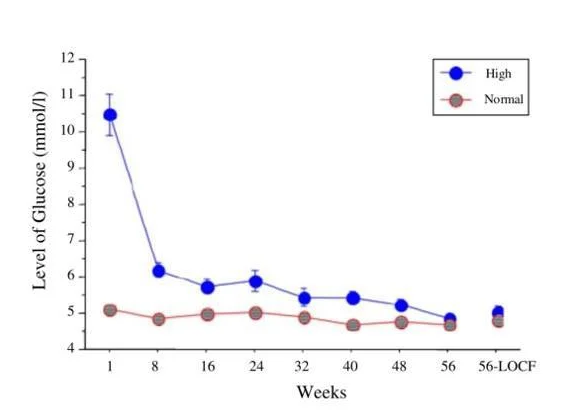
Similarly, ketogenesis suppresses blood lipids, reducing the risk of type 2 diabetes. The buildup of certain lipid metabolites triggers lipid-induced insulin resistance, leading to diabetes. Hence, ketosis eradicates this risk. Equally, a very low-carbohydrate keto diet (VLCKD) considerably improves hyperinsulinemia, lowering the incidence of type 2 diabetes (Foley, 2021, p. 465; Choi, Jeon, and Shin, 2020, p. 2005). The efficacy of KD in reducing blood glucose levels is demonstrated in Figure 5 below.
KD has emerged as a critical therapy in cancer treatment. Tumor cells utilize glucose for continued growth; therefore, LCD limits energy supplies to these cells, slowing their development (Talib et al., 2021, p. 558; Crosby et al., 2021; Ludwig, 2019, p. 1356). Since tumor cells have mitochondrial defects, they cannot use ketones as energy sources, inhibiting metastasis. As a result, KD can starve the tumor cells while ensuring the continued functioning of the normal cells (see Figure 6).
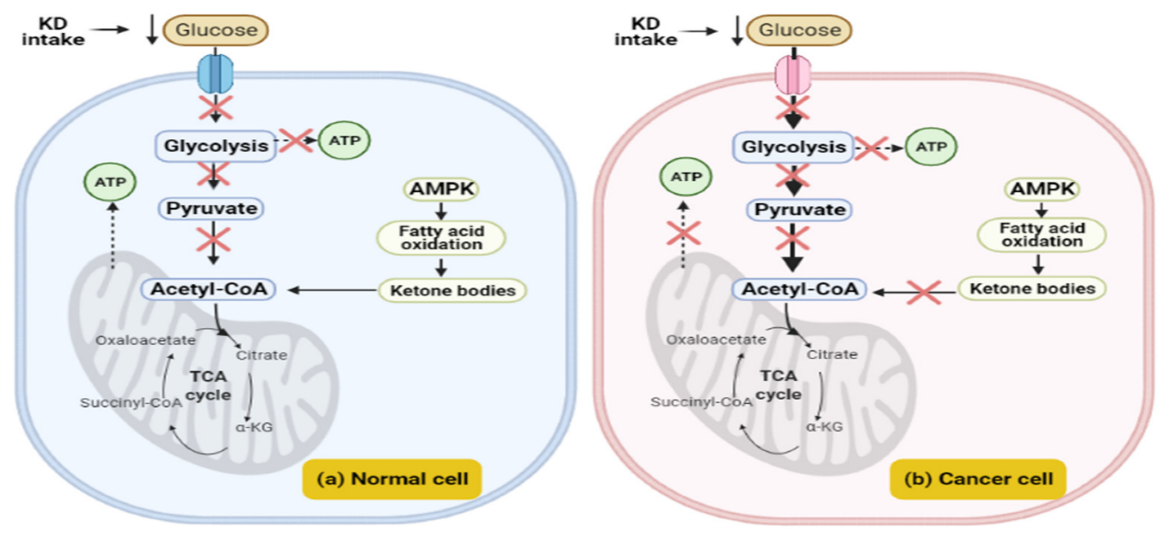
This makes the tumor cells extremely vulnerable to radiation and chemotherapy (Dowis & Banga, 2021). In addition, KD lowers insulin production, a hormonal driver for certain tumors, and decreases cell proliferation signals, preventing tumor growth (Ludwig, 2019; Dowis & Banga, 2021, p. 1654).
Similarly, ketones also impede inflammation, which acts as a tumor trigger. KD may not independently cure cancer, but it can be combined with other treatments, including phosphoinositide 3-kinase inhibitors, increasing their efficacy (Zhu et al., 2021). Thus, KD suppresses tumor growth and boosts cancer treatment efficacy, improving patient outcomes.
Despite the popular misconception that high-fat diets increase the susceptibility to cardiovascular disorders (CVDs), KD has been associated with reducing the risk of these diseases. According to Gołąbek and Regulska-Ilow (2022), KD helps prevent and manage CVDs. The authors highlight that the diet lowers carbohydrate intake and effectively regulates glycemic control, reducing the incidence of CVDs.
In addition, the ketones produced during ketogenesis have been shown to have anti-inflammatory effects, which prevent cardiovascular complications (Mohammadifard et al., 2022, p. 3499). Similarly, KD lowers triglycerides, cholesterol levels, and low-density lipoprotein while increasing the high-density lipoprotein, thus decreasing the risk of CVDs (Ludwig, 2019, p. 1355; Dowis & Banga, 2021). Hence, KD is beneficial in lowering the risk of CVDs.
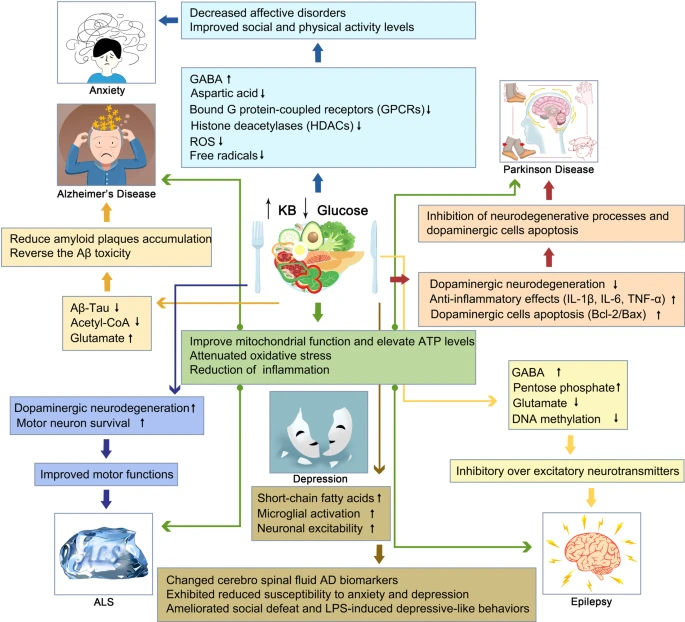
Keto diets have shown the potential to treat several neurodegenerative disorders. The findings from Zhu et al. (2021) and Alharbi and Al-Sowayan’s (2020) research indicate that KD improves mitochondrial dysfunction and oxidative stress, which triggers most neurodegenerative diseases. The ketones produced in an LCD offer neuroprotective properties to the brain, which assist in treating disorders such as refractory epilepsy and Alzheimer’s Disease (AD). KD’s altered metabolism has anti-seizure impacts and safeguards against Aβ neurotoxicity by increasing ATP production and lowering the excitability of neurons (Zhu et al., 2021; Crosby et al., 2021).
Additionally, KD enhances insulin sensitivity and decreases inflammation in the brain. The diet can also elevate the amount of neurotransmitter GABA, which calms the brain and prevents depressive-like traits and anxiety disorders (Zhu et al., 2021). In addition, KD enhances motor symptoms and protects against the loss of dopaminergic neurons, helping manage Parkinson’s disease. Equally, KD’s ability to improve oxidative stress and mitochondrial dysfunction has been critical in treating Amyotrophic Lateral Sclerosis. Therefore, KD can be used as a prospective treatment for multiple neurodegenerative diseases, as illustrated in Figure 7 below.
Adopting a KD can considerably help manage polycystic ovary symptoms (PCOS) among women. Paoli et al. (2020) depict that insulin resistance triggers PCOS pathogenesis (p. 1). Therefore, KD can help enhance insulin sensitivity and reduce insulin levels, lowering the hyperandrogenism associated with the disorder. These findings are supported by Zhu et al.’s study, which asserts that apart from addressing insulin sensitivity, KD can also decrease weight loss, which is critical for women with PCOS (2021, p. 7).
Similarly, Baldwin and Tan’s (2020) study indicates that KD decreases body weight and inflammation, thus blocking or reducing the exacerbation of acne (p. 57). In this case, LCD lowers the glycemic index and glycemic load, which acts as the pathogenesis of acne. Furthermore, a study by Lin, Liu, and Hung (2021) depicts that KD has anti-aging effects (p. 2). The calorie restriction coupled with the impact of the β-hydroxybutyrate ketone increases individuals’ lifespan through epigenetic regulation (Lin, Liu, and Hung, 2021; Alharbi & Al-Sowayan, 2020, p. 302). Therefore, KD improves PCOS symptoms, helps in acne management, and presents anti-aging benefits.
Harmful Effects of Ketogenic Diet
Despite the numerous benefits linked with KD, the diet has several adverse effects on individuals. The initiation of KD has been associated with multiple side effects commonly called ‘keto flu.’ Keto flu symptoms include vomiting, headache, low exercise tolerance, dizziness, fatigue, and constipation (Crosby et al., 2021; Alharbi & Al-Sowayan, 2020; Shalabi et al., 2021).
These findings are supported by Zhu et al.’s (2021) research, which further states that several short-term negative effects, such as dehydration, metabolic acidosis, diarrhea, irritability, and hypoglycemia, may be witnessed during the first few weeks of KD (p. 13). Nevertheless, these symptoms usually resolve as the body adjusts to the ketogenic state. KD has been associated with long-term adverse health effects on individuals. Research indicates that the high fat content linked with KD may result in excess fat accumulation in the liver, causing hepatic steatosis (Batch et al., 2020).
Similarly, KD is low on essential nutrients such as fiber and vitamins A and E, resulting in nutritional deficiencies that predispose individuals to impaired immune functions (Crosby et al., 2021; Batch et al., 2020). The lack of crucial minerals such as calcium, potassium, magnesium, and iron may weaken bones and heighten individuals’ risk of infections. Equally, Zhu et al.’s findings show that high fat intake results in the buildup of LDL cholesterol, a risk factor for cardiovascular complications (2021, p. 13). Other long-term impacts of KD may include anemia, nephrolithiasis, cardiomyopathy, and neuropathy (Zhu et al., 2020; Crosby et al., 2021, p. 7). Therefore, KD poses severe health impacts to individuals in the long term.
According to McGaugh and Barthel (2020), KD may severely affect pregnant women. The authors highlight that low-carbohydrate diets in pregnant women can predispose them to the risk of congenital disabilities. In this case, the impacts of KD on pregnancy may include stillbirths, spina bifida, and anencephaly (p. 87).
Additionally, Crosby et al.’s (2021) study discusses KD’s effects before conception and during the periconceptional period. Based on the authors’ findings, low-carbohydrate foods during pre-pregnancy and pregnancy can heighten the risk of congenital disabilities and gestational diabetes, respectively. Research indicates that women who consume diets with low carbohydrate levels a year before conceiving have a 30% likelihood of delivering infants with neural tube defects (Crosby et al., 2021; McGaugh & Barthel, 2020).
Infants born to women on KD before or during pregnancy also had reduced levels of folic acid. Regarding gestational diabetes, research shows that women consuming diets with low carbohydrate levels have a 27% higher propensity for the condition than those on a high-sugar regimen (Crosby et al., 2021). Thus, the keto diet increases the risk of congenital disabilities and diabetes among pregnant women.
The prolonged consumption of KD may lead to the development of chronic diseases. According to Crosby et al.’s findings, the foods recommended for KD, such as red meat, have been shown to increase cancer risk (2021). Alternatively, fruits, whole grains, and vegetables associated with reduced all-cause mortality and cancer risk are eliminated from the diet.
Similarly, KD has been established as a significant contributor to Alzheimer’s disease (Crosby et al., 2021; Zhu et al., 2020). KD is characterized by saturated fat intake, a risk factor for AD. Hence, consuming saturated fats associated with KD can predispose individuals to chronic illnesses such as cancer and AD.
Individuals who use KD as a therapy may be exposed to several adverse effects, resulting in the deterioration of their health. Patients using KD as a treatment approach can experience gastrointestinal complications such as emesis, constipation, gastroesophageal reflux, and abdominal pain (Zhu et al., 2021; Lin, Liu, and Hung, 2021). In addition, KD has been linked to aggravating the health conditions of individuals with type 1 diabetes. Since this disorder is considerably associated with metabolic irregularities, ketosis and hyperketonemia may increase the risk of complications. Similarly, a study by Zhu et al. (2021) indicates that animal model research demonstrated that KD might intensify the risk for hypertension and cause endothelial dysfunction, resulting in renal failure.
Due to the reduced glucose levels and increased lipid metabolism, the keto diet causes overactivation of the renin-angiotensin-aldosterone system. The existence of ketones lowers endothelial nitric oxide synthase, resulting in hypertension and endothelial malfunction. Not to mention, KD can also exacerbate interstitial fibrosis and impair cognitive behavior among individuals (Zhu et al., 2021). Therefore, KD can harm individuals, resulting in severe health complications.
Benefits vs. Harmful Effects
Despite its renewed prominence, KD presents positive and negative impacts on individuals. On one hand, the diet has proven pivotal in weight loss due to the low-carbohydrate intake and suppressed appetite. This makes it indispensable in treating obesity and type 2 diabetes (Ludwig, 2019; Ashtary-Larky et al., 2021). On the contrary, KD lacks essential nutrients such as vitamins A and E and calcium. The prolonged deficiency of such nutrients may impair immune function and increase an individual’s risk of infections (Batch et al., 2020; Crosby et al., 2021).
Another benefit of KD is that it improves insulin sensitivity, which is crucial to persons with type 2 diabetes (Choi, Jeon, and Shin, 2020). Alternatively, KD’s initiation has been associated with ‘keto flu,’ where individuals may experience adverse effects such as headaches, vomiting, fatigue, nausea, and dizziness (Crosby et al., 2021; Alharbi & Al-Sowayan, 2020; Shalabi et al., 2021). Thus, although KD has numerous benefits for individuals, its consumption is associated with adverse effects and acute nutritional deficiencies.
KD is instrumental in reducing inflammation and alleviating various chronic disorders. In this case, ketones have been shown to have anti-inflammatory effects, which are crucial in improving diseases such as cancer, CVD, and neurodegenerative illnesses (Dowis & Banga, 2021; Zhu et al., 2021). Alternatively, the high-fat content linked to KD has been highlighted as a major contributor to the development of terminal disorders.
Crosby et al.’s (2021) study indicates that saturated fat intake significantly increases the risk for AD, while consuming red meat may increase an individual’s susceptibility to cancer (p. 5). Diets containing high fats have also been linked to an increased risk of kidney stones and hypertension (Zhu et al., 2021). Therefore, considering KD’s positive and negative impacts, individuals should consult with healthcare providers before initiating the diet to ensure that it is appropriate and safe for their health.
Other Diets as Opposed to Keto
Several other dietary patterns have different carbohydrate and fat ratios. A study by Landry, Crimarco, and Gardner (2021) shows that Zone, Paleo, and South Beach can be classified as low-carbohydrate diets. In this case, the Zone diet comprises 30% proteins, 40% carbohydrates, and 30% fats. According to Sears, Perry, and Saha (2021), the Zone diet has superior anti-inflammatory properties critical in healing injuries triggered by inflammation (127).
On the other hand, the Paleo diet (PD) consists of 30% proteins, 35% fats, and 35% carbohydrates (Frączek et al., 2021, p. 1019). It mainly consists of vegetables, grass-fed meat, nuts, fungi, and roots while excluding legumes, dairy products, and grains. Similar to the case of KD, PD has several health benefits, including treating obesity, blood lipid disease, and diabetes, among others.
According to Landry, Crimarco, and Gardner (2021), the South Beach diet involves cutting off nearly all carbohydrates for a fortnight. Then, it progresses to moderate LCD, allowing for 30% of calorie intake from carbohydrates. Therefore, Zone, Paleo, and South Beach diets emphasize low to medium fats as opposed to KD.
The Mediterranean diet (MD) is another LCD with several health benefits. The findings from Landry, Crimarco, and Gardner’s (2021) study show that MD recommends consuming nuts, seeds, olive oil, fatty fish, and avocados. Merrill et al.’s (2020) discussion corroborates the research, further highlighting that a low-carbohydrate Mediterranean diet (LCMD) helps in weight loss and lowers glycated hemoglobin and triglycerides (p. 135).
A study by Gardner et al. (2020) compared the impact of KD and MD on glycated hemoglobin among persons with prediabetes and type 2 diabetes. The findings concluded that there was no difference in the HbA1c values between KD and MD. However, the results showed improvement from baseline on both diets, with KD exhibiting greater triglyceride reduction than MD.
The authors also stress that excluding fruits, grains, and legumes makes KD less sustainable than MD. Zone, Paleo, South Beach, and Mediterranean diets restrict fat intake, resulting in critical health benefits. Although KD may have better health outcomes than other low-fat diets, it is stricter on carbohydrate intake, making it challenging for individuals to adhere to.
Conclusion
The Keto diet greatly restricts carbohydrate and protein intake while increasing high-fat consumption. The diet’s health benefits have contributed to its increased demand. The carbohydrate restriction and suppression of appetite associated with KD help in weight loss, which is critical in managing obesity and type 2 diabetes. In addition, the altered metabolism and the existence of ketones have contributed to KD’s therapeutic effects for various diseases such as CVD, cancer, Alzheimer’s disease, epilepsy, PCOS, Parkinson’s disease, acne, and Amyotrophic lateral sclerosis. Nevertheless, adherence to KD is associated with severe nutritional deficiencies, congenital disabilities, and exposure to chronic illnesses such as cancer and AD.
Other low-carbohydrate and low-fat diets, such as Zone, South Beach, and Paleo, have been shown to have several health benefits. Although KD has excellent potential as a therapeutic approach for chronic illnesses, more research is needed to offer high-quality clinical evidence regarding its efficacy and safety in dealing with different health complications. In addition, the diet can be modified to make it more tolerable and lessen its side effects.
Reference List
Alharbi, A. and Al-Sowayan, N.S. (2020) ‘The effect of ketogenic diet on health‘, Food and Nutrition Sciences, 11(04), pp. 301–313. Web.
Ashtary-Larky, D. et al. (2021) ‘Ketogenic diets, physical activity and body composition: A review‘, British Journal of Nutrition, 127(12), pp. 1898–1920. Web.
Baldwin, H. and Tan, J. (2020) ‘Effects of diet on acne and its response to treatment‘, American Journal of Clinical Dermatology, 22(1), pp. 55–65. Web.
Batch, J.T. et al. (2020) ‘Advantages and disadvantages of the ketogenic diet: A review article‘, Cureus 12(8), e9639. Web.
Brouns, F. (2018) ‘Overweight and diabetes prevention: Is a low-carbohydrate–high-fat diet recommendable?‘, European Journal of Nutrition, 57(4), pp. 1301–1312. Web.
Choi, Y.J., Jeon, S.-M. and Shin, S. (2020) ‘Impact of a ketogenic diet on metabolic parameters in patients with obesity or overweight and with or without type 2 diabetes: A meta-analysis of randomized controlled trials‘, Nutrients, 12(7), p. 2005. Web.
Crosby, L. et al. (2021) ‘Ketogenic diets and chronic disease: Weighing the benefits against the risks‘, Frontiers in Nutrition, 8 (702802), pp. 1-11. Web.
Dowis, K. and Banga, S. (2021) ‘The potential health benefits of the ketogenic diet: A narrative review‘, Nutrients, 13(5), p. 1654. Web.
Foley, P.J. (2021) ‘Effect of low carbohydrate diets on insulin resistance and the metabolic syndrome‘, Current Opinion in Endocrinology, Diabetes & Obesity, 28(5), pp. 463–468. Web.
Frączek, B. et al. (2021) ‘Paleolithic diet—effect on the health status and performance of athletes?‘, Nutrients, 13(3), p. 1019. Web.
Gardner, C.D. et al. (2022) ‘Effect of a ketogenic diet versus Mediterranean diet on glycated hemoglobin in individuals with prediabetes and type 2 diabetes mellitus: The interventional keto-med randomized crossover trial‘, The American Journal of Clinical Nutrition, 116(3), pp. 640–652. Web.
Gołąbek, K.D. and Regulska-Ilow, B. (2022) ‘Possible nonneurological health benefits of ketogenic diet: Review of scientific reports over the past decade‘, Journal of Obesity, 2022, (7531518), pp. 1–7. Web.
Gropper, S.S. (2023) ‘The role of nutrition in chronic disease‘, Nutrients, 15(3), p. 664. Web.
Landry, M.J., Crimarco, A. and Gardner, C.D. (2021) ‘Benefits of low carbohydrate diets: A settled question or still controversial?‘, Current Obesity Reports, 10(3), pp. 409–422. Web.
Li, S. et al. (2022) ‘The effect of periodic ketogenic diet on newly diagnosed overweight or obese patients with type 2 diabetes‘, BMC Endocrine Disorders, 22(34), pp. 1-6. Web.
Li, Z. and Heber, D. (2020) ‘Ketogenic diets,’ JAMA, 323(4), p. 386. Web.
Lin, T.-Y., Liu, H.-W. and Hung, T.-M. (2021) “The ketogenic effect of medium-chain triacylglycerides,” Frontiers in Nutrition, 8 (747284). pp. 1-5. Web.
Ludwig, D.S. (2019) ‘The ketogenic diet: Evidence for optimism but high-quality research needed‘, The Journal of Nutrition, 150(6), pp. 1354–1359. Web.
Mawer, R. (2017) ‘10 Graphs That Show the Power of a Ketogenic Diet‘, Healthline, Web.
McGaugh, E., & Barthel, B. (2022). ‘A review of ketogenic diet and lifestyle‘, Missouri Medicine, 119(1), 84–88. Web.
Merrill, J.D. et al. (2020) ‘Low-carbohydrate and very-low-carbohydrate diets in patients with diabetes‘, Diabetes Spectrum, 33(2), pp. 133–142. Web.
Mohammadifard, N. et al. (2022) ‘The effect of ketogenic diet on shared risk factors of cardiovascular disease and cancer‘, Nutrients, 14(17), p. 3499. Web.
Sears, B., Perry, M. and Saha, A.K. (2021)’ Dietary technologies to optimize healing from injury-induced inflammation‘, Anti-Inflammatory & Anti-Allergy Agents in Medicinal Chemistry, 20(2), pp. 123–131. Web.
Shalabi, H. et al. (2021) ‘Ketogenic diets: Side effects, attitude, and quality of life‘, Cureus 13(12), e20390. Web.
Talib, W.H. et al. (2021) ‘Ketogenic diet in cancer prevention and therapy: Molecular targets and therapeutic opportunities‘, Current Issues in Molecular Biology, 43(2), pp. 558–589. Web.
Wohlgemuth, R. (2020) ‘The science behind going keto‘, Bioscope, Web.
Zhou, C. et al. (2022) ‘Ketogenic diet benefits to weight loss, glycemic control, and lipid profiles in overweight patients with type 2 diabetes mellitus: A meta-analysis of randomized controlled trials‘, International Journal of Environmental Research and Public Health, 19(16), p. 10429. Web.
Zhu, H. et al. (2022) ‘Ketogenic diet for human diseases: The underlying mechanisms and potential for clinical implementations‘, Signal Transduction and Targeted Therapy, 7(11), pp. 1-21. Web.