Introduction
The mumps virus (MV), classified within the Paramyxoviridae family, is an infectious disease impacting the salivary glands and other vital organs. This research paper seeks to explore the virological aspects of the mumps virus, focusing on its structure, virulence factors, and the immune responses it triggers. Additionally, the pathology of mumps, complications, and transmission dynamics are elucidated, coupled with the prevention strategies, emphasizing the importance of the Measles, Mumps, and Rubella (MMR) vaccine. Treatment modalities, both current and potential, are addressed, highlighting antiviral agents and supportive care. Through this comprehensive exploration, a holistic understanding of the mumps virus and its implications is provided.
Description of the Microorganism
The mumps virus is a single-stranded, enveloped RNA that falls within the Paramyxoviridae family. This, therefore, explains why it is classified as a virus (Jayawardena et al., 2020). Regarding size and shape, MV has an average diameter of about 150 nanometers, and its structure is characterized by a helical nucleocapsid surrounded by a lipid envelope (Jayawardena et al., 2020). MV is widely known for causing mumps in human beings – it affects the salivary glands.
While this is the case, the morphology of MV is not discernible under a light microscope. Alternatively, electron microscopy is often employed when it comes to visualizing and observing the unique details of viral particles. This technique uses a beam of electrons as opposed to light – it provides higher resolution. Similarly, staining techniques are not applicable to mumps virus visualization, as electron microscopy allows for direct observation of the virus’s morphology and structure.
Virulence Factors
The mumps virus exhibits several virulence factors that facilitate the ability of the pathogen to infect humans. A major factor consideration lies in the MV’s ability to evade the host’s immune system. As evidenced in Jurković et al.’s (2021) study, MV has the capability to inhibit the host’s interferon response, suppressing its production, thus thwarting the host’s early immune responses.
In addition to this, MV has fusion proteins located specifically on its envelope, facilitating its entry into and exit from the host cells. The virus’ ability to disseminate within the host eventually leads to widespread infection (Jurković et al., 2021). This efficient cell entry mechanism enhances the virus’ ability to infect a wide range of cells, contributing to its systemic spread within the host. As it replicates prolifically in the salivary glands, it ends up causing swelling and inflammation.
Immunity
The MV primarily elicits an immune response from the host, involving both innate and adaptive defenses. Innate defenses comprise physical barriers such as the skin and mucous membranes. Similarly, cellular components, like the natural killer cells, collectively serve as the first line of defense against the virus.
The adaptive immune response is crucial for long-term defense against the mumps virus. Upon infection, the body generates specific antibodies, primarily immunoglobulin M (IgM), followed by immunoglobulin G (IgG), which target and neutralize the virus (Yang et al., 2020). However, this pathogen does not typically induce delayed-type hypersensitivity; instead, the adaptive immune response to the mumps virus is primarily antibody-mediated.
Pathology
MV causes mumps, which manifest as an infectious disease marked by the swelling of the salivary glands. This condition affects several tissues, among them the salivary glands. Here, the pathogen targets mainly the parotid glands on the sides of the face, leading to noticeable swelling and tenderness.
Mumps, if left untreated, may end up causing several complications. As explicated by Kohil et al. (2021), acute complications include viral meningitis, characterized by inflammation of the membranes surrounding the brain and spinal cord, leading to symptoms such as fever, headache, and neck stiffness. Chronic complications comprise orchitis in males or oophoritis in females (Kohil et al., 2021). They affect the testes and ovaries and carry the risk of long-term consequences, such as sterility. Overall, the MV infects the respiratory system, spreading through respiratory droplets. Most importantly, the virus targets respiratory mucosa and, as such, cannot be considered an opportunistic pathogen.
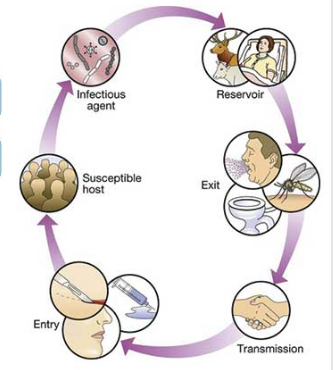
Upon a closer look at figure 1 above, it is clear that the primary reservoir for MV is humans – they serve as the main source of the virus. However, mumps is not known to be transmitted by vectors such as mosquitoes or ticks – it is spread mainly through respiratory droplets resulting from coughing, sneezing or talking. The type of transmission, as evidenced above, is through direct contact with respiratory secretions from an infected person (Li et al., 2022). The portals of entry through the respiratory mucosa – an uninfected person inhales respiratory droplets containing the mumps virus. The port of existence is saliva – the infected individuals can expel virus-laden droplets into the air when coughing or sneezing.
Prevention of Mumps
Measles, Mumps, and Rubella (MMR) is a childhood vaccine developed to protect individuals against mumps. The MMR vaccine is typically administered in two doses (Jayawardena et al., 2020) – the first dose is given between 12 and 15 months of age, while the second one is recommended starting at age 4 to 6 years. Additionally, certain at-risk groups, such as college students, healthcare workers, and international travelers who may not have previously been vaccinated, may be advised to receive the MMR. This is necessary if there is uncertainty about their immune status. Overall, the MMR contains weakened forms of the viruses, allowing it to stimulate the immune system to produce an adherence response without causing the disease. The measures that can be implemented in the event MMR is unavailable include isolation, promoting good respiratory hygiene, and encouraging frequent handwashing.
Treatment of Mumps
The main treatment option for mumps is supportive care to relieve symptoms and prevent complications. Research recommends the use of some antiviral agents since there is no specific antiviral medication approved for treating mumps. Antiviral drugs typically work by inhibiting specific stages of the viral replication cycle but cannot suppress serious complications (Kato et al., 2021). Additional therapeutic measures may include pain and fever management through over-the-counter relievers such as acetaminophen and hydration and nutrition through adequate fluid intake. In line with this, measures such as widespread vaccination and good respiratory hygiene have proven effective in reducing the incidence of mumps.
Clinical Relevance
In the context of clinical relevance, MV, as a single-stranded RNA virus, lacks the capability to develop resistance to antibiotics in a similar way as a bacterium. Therefore, the concept of multi-drug resistance (MDR) does not work against viral infections, including mumps. In essence, prevention through vaccination remains the most effective strategy against mumps. In healthcare settings, much attention should be on the adoption of evidence-based infection control measures, vaccination and public health interventions to minimize the spread of the virus.
Conclusion
The MV presents a unique set of challenges in the context of infectious diseases. Its intricate structure, virulence factors, and mode of transmission underscore the necessity for robust preventive measures. The MMR vaccine, as evidenced above, plays an important role in mitigating the impact of mumps, supported by its effective stimulation of the immune system. While treatment options remain limited, ongoing research into antiviral agents offers potential avenues for future interventions.
References
Jayawardena, N., Poirier, J. T., Burga, L. N., & Bostina, M. (2020). Virus–receptor interactions and virus neutralization: Insights for oncolytic virus development. Oncolytic Virotherapy, 9(3)1-15. Web.
Jurković, M., Slović, A., Forčić, D., Ivančić-Jelečki, J., Košutić-Gulija, T., & Jagušić, M. (2021). Influence of Ribavirin on mumps virus population diversity. Viruses, 13(12), 2535. Web.
Kato, F., Nakatsu, Y., Murano, K., Wakata, A., Kubota, T., Hishiki, T., Yamaji, T., Kidokoro, M., Katoh, H., & Takeda, M. (2021). Antiviral activity of CD437 against Mumps virus. Frontiers in Microbiology, 12. Web.
Kohil, A., Jemmieh, S., Smatti, M. K., & Yassine, H. M. (2021). Viral meningitis: An overview. Archives of Virology, 166(2), 335–345. Web.
Li, M., Liu, Y., Yan, T., Xue, C., Zhu, X., Yuan, D., Hu, R., Liu, L., Wang, Z., Liu, Y., & Wang, B. (2022). Epidemiological characteristics of mumps from 2004 to 2020 in Jiangsu, China: A flexible spatial and spatiotemporal analysis. Epidemiology and Infection, 150. Web.
Yang, L., Grenfell, B. T., & Mina, M. J. (2020). Waning immunity and re-emergence of measles and mumps in the vaccine era. Current Opinion in Virology, 40, 48–54. Web.