Subjective Findings
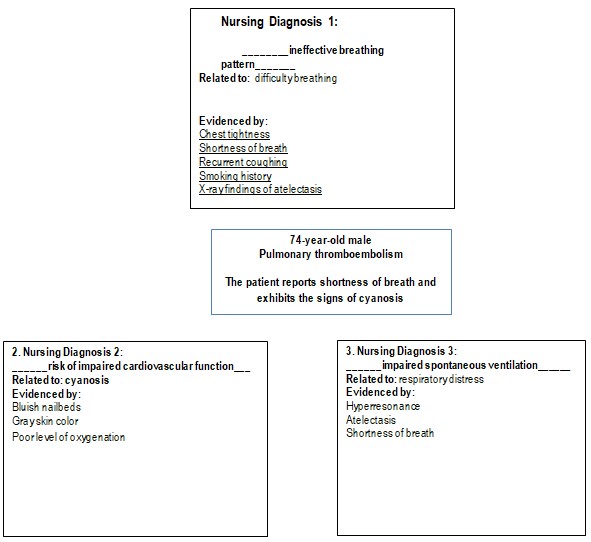
The subjective data used in nursing diagnosis typically refers to the visual examination of patients and their reported symptoms. In this case, subjective data included in the diagnosis was the reported shortness of breath and difficulty breathing that the patient indicated upon admission to the emergency department. The nurse’s subjective data input was an observation of Mr. Ritter’s anxiety, which they confirmed by watching the patient sitting in a tripod position.
Objective Findings
Objective findings of a patient’s examination informing the nursing diagnosis come from standard medical tests and evaluations. For instance, the patient’s degree of respiratory distress could be evaluated by the retracting respiration rate of 26 breaths per minute, a high pulse of 120 beats per minute, and extremely low oxygen saturation. Further objective input into the patient’s diagnosis was given by the X-ray test showing the signs of atelectasis in the patient’s lungs. Identifying hyper-resonance in the patient’s chest wall and evaluating skin and nailbed color is also objective evidence.
Pathophysiology of the Patient’s Disease Process
As the patient has a history of COPD diagnosis, it is vital to consider the pathophysiology of his disease process through the prism of potential exacerbations of COPD. Güder and Stöck (219) noted that COPD triggers the destruction and remodeling processes in the bronchiolar architecture of the patient’s lungs, leading to impaired air inhalation. The outcome of such a process is thoracic muscle exhaustion, inadequate oxygenation, and dyspnea. Because of these pathophysiological processes, COPD often leads to the development of congestive heart failure and pulmonary embolism caused by blood vessel destruction. Dentali et al. (2020) also confirmed that COPD is an independent risk factor for pulmonary embolism, posing significant health risks.
Smoking-related COPD is characterized by airway inflammation, evidenced by the increase of CD8+ T cells, macrophages, neutrophils, and B cells at later stages of COPD development (Santus et al., 2019). The primary site of COPD inflammation is small airways, the ones escaping adequate biopsy assessment, so the COPD treatment should be selected in a way that manages mechanical stress. Such an approach can reduce the risk of inflammation and asthma development (Santus et al., 2019). Another health outcome of COPD progression is pulmonary emphysema, which affects distal air spaces of the terminal bronchiole and causes abnormal enlargement. At the same time, the airway walls and lung parenchyma get destroyed, with evidenced loss of lung elasticity and accompanying pulmonary problems (Pahal et al., 2018).
References
Dentali, F., Pomero, F., Di Micco, P., La Regina, M., Landini, F., Mumoli, N., Pieralli, F., Giorgi-Pierfranceschi, M., Re, R., Vitale, J., Fabbri, L. M., Fontanella, A., & Arioli, D. (2020). Prevalence and risk factors for pulmonary embolism in patients with suspected acute exacerbation of COPD: A multi-center study. European Journal of Internal Medicine, 80, 54-59.
Güder, G., & Störk, S. (2019). COPD and heart failure: Differential diagnosis and comorbidity. Herz, 44, 502-508.
Pahal, P., Avula, A., & Sharma, S. (2018). Emphysema. StatPearls Publishing.
Santus, P., Pecchiari, M., Tursi, F., Valenti, V., Saad, M., & Radovanovic, D. (2019). The airways’ mechanical stress in lung disease: Implications for COPD pathophysiology and treatment evaluation. Canadian Respiratory Journal, 1-8.