The sentinel event deals with a 37-year-old woman named Sady with diabetes and high blood pressure complications during the intrapartum phase of pregnancy who started developing hypertension despite her efforts to keep glucose low. The patient’s physician was able to keep her hypertension stable by monitoring her glucose and BP levels. However, when Sady went into labor, her physician was engaged elsewhere, and an alternate physician was delivering her baby. He did not take time to read Sady’s physician notes and failed to apply the magnesium the patient needed for stabilization. Sady had no energy to continue her labor and was taken to the OR, where she had a c-section and ensuing cardiac arrest. The child was delivered stillborn due to placental abruption. The staff involved in the sentinel event comprises Sady’s leading physician and the one who delivered her baby as well as OR staff.
The error occurred due to negligence when the physician who delivered Sady’s baby failed to administer the magnesium needed to stabilize her condition. This error was detected when the patient’s condition became critical, and she was taken to OR. The event was reported to the Joint Commission in order to “positively impact care, treatment, and services by helping health care organizations identify opportunities to change their culture, systems, and processes to prevent unintended harm” (The Joint Commission). The sentinel event was reported within 45 days from the time it took place. A thorough analysis of the event helped to crystallize the reasons behind it and enhance the public’s knowledge about the necessary procedures in similar cases.
As far as procedural errors are concerned, the error should have been detected when a new physician was called to deliver the baby. Before assisting with childbirth, he should have read the notes of his colleague, which would have prevented the error. Administration of the magnesium was the procedure missed that led to a sentinel event. The accreditation agency involved in this sentinel event is the Joint Commission (TJC), where the event should be reported. The agency’s purpose is to “enhance quality of care and patient safety” by disclosing the factors leading to sentinel events and elaborating the ways through which these factors can be mitigated. The agency’s reporting expectations would involve the time and place of the occurrence, its possible reasons, and the measures undertaken to minimize the damaging effects of a sentinel event.
Root Cause Analysis
Root Cause Analysis Report
To determine the cause of the event, data on the place, key participants, and the medical side of the issue should be collected. The place where the sentinel event took place is a hospital, and key participants are the physician who delivered the baby and OR team. The rationale for choosing these data lies in the fact that human error was the leading cause of the sentinel event, and it’s essential to determine why this error happened.
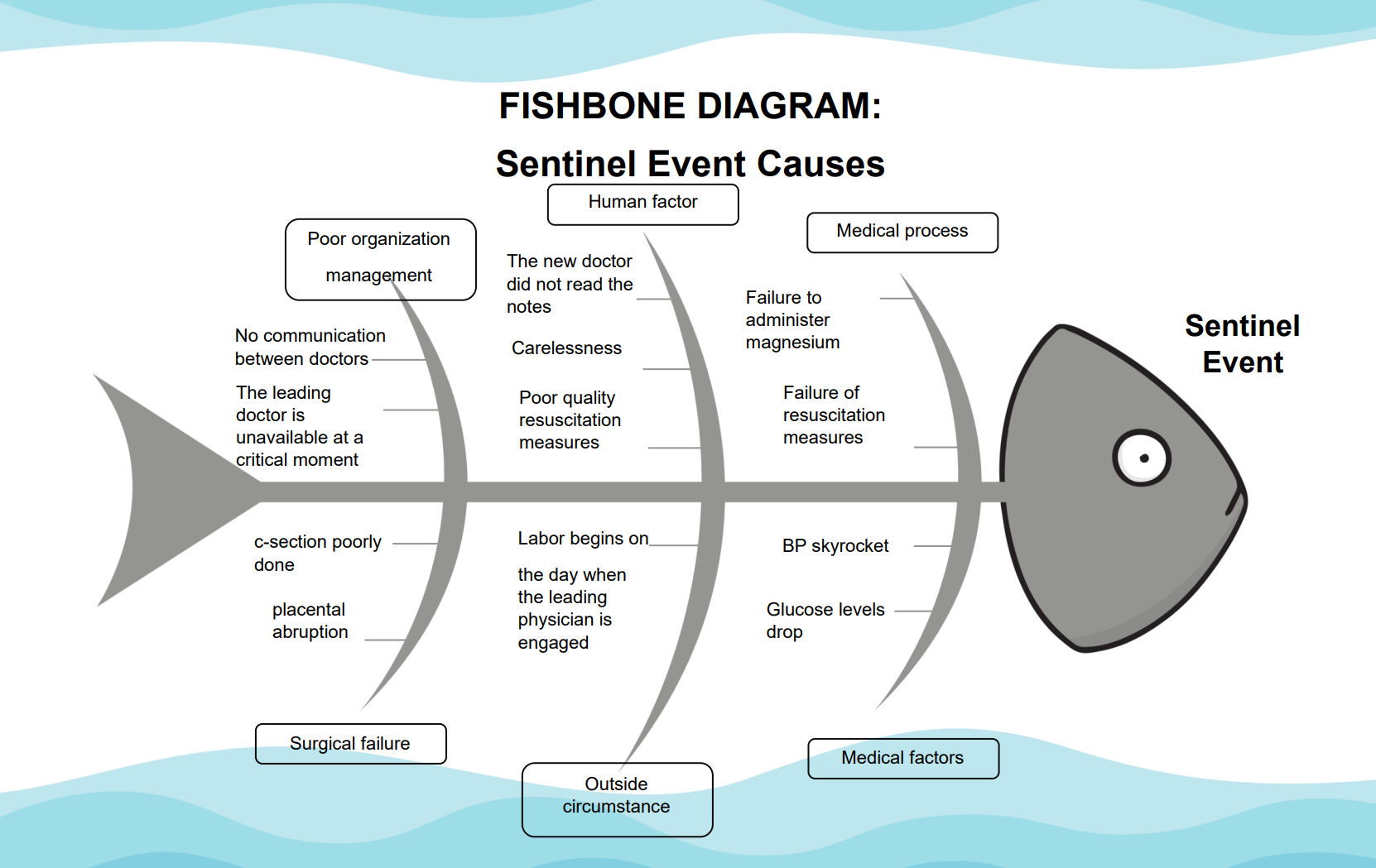
In this particular case, the sentinel event’s probable cause lies with systems error as well as human error. First of all, the patient’s labor began when her leading physician was not only unable to deliver a child but also to consult due to his or her engagement elsewhere, which constitutes a management error on the part of the hospital. Either a doctor’s consultation should have been available, or somebody should have seen to it that his notes are read by the new physician. There should have been a person responsible for Sady’s delivery, as she was a patient from a high risks group. Secondly, the doctor who actually delivered the baby failed to read the notes on Sady’s health and, moreover, lacked the knowledge to administer the right medication based on the clinical symptoms he saw.
The human factors relevant to the outcome in this particular case include negligence on the part of a new doctor, his lack of knowledge to administer the magnesium-based on the patient’s clinical symptoms, and poor surgical skills as placental abruption happened due to the c-section he performed. Systems factors comprise poor management and labor organization. The process errors relevant to the outcome are the new physician’s failure to read the notes and his inability to administer the right medication due to his lack of knowledge as well as poor surgical skills.
There were many steps that did not go as intended in this particular case. First of all, the notes on the patient’s state and possible complications should have been carefully considered. Secondly, magnesium should have been administered to stabilize her condition. Thirdly, she should have given birth herself instead of having a c-section, which would have been possible if the right medication had been given to her. The outcome was also impacted by the equipment performance as the doctors did not manage to restart the patient’s heartbeat after the cardiac arrest; it is possible that the equipment for that was faulty.
There are many areas in a healthcare organization where a similar sentinel event can happen since this event is conditioned by poor management within the hospital itself. All patients with serious health risks monitored by their physicians run the risk of being admitted to a hospital with an acute state and being operated on or treated by a doctor who knows nothing about the patient’s illnesses and risk factors. This may lead to all kinds of complications and even deaths as the exchange of information is poor not only between different clinics but also, sometimes, between different departments as well. In cases where a patient’s health depends on the physician’s timely access to information, the uncoordinated work of different departments presents a threat to the patient’s life and health.
During this particular sentinel event, the staff performance did not meet the expectations. The necessary medication was not administered, and clinical symptoms were ignored till it became too late and the transfer of the patient to the OR became necessary. The surgical part, the c-section, was performed badly and resulted in placental abruption and subsequent cardiac arrest. Resuscitation measures taken were possibly insufficient since the OR staff did not manage to restart the patient’s heart again. Moreover, they lost the baby as well and failed to revive it.
The corrective action plan must be developed to eliminate similar risks in future events. For this, risk reduction strategies in management, as well as the medical field, must be elaborated and implemented. In the management field, the key problem is the lack of adequate exchange of information between the departments, which results in poor performance of the medical teams in urgent cases as they often have no knowledge of a patient’s previous medical history. To remedy this situation, a special application for information exchange should be elaborated where doctors, entering the name of a particular patient, can see all the chronic diseases and treatment the patient receives as well as recommended medical manipulations. Moreover, the clinical guidelines of the hospital should comprise an obligatory familiarization with the patient’s medical history before any major interventions such as baby delivery or any kind of surgery.
In the medical field, risk reduction strategies should comprise staff education on the most common disease complications that they can come across in their practice, as well as strategies to avoid these complications. In the field of child delivery, every physician should be taught about the risks of maternal hypertension and pre-eclampsia states as well as diabetes and the risks it poses for mother and child in the labor process. Education on the symptoms through which such states manifest themselves as well as on the necessary measures needed to offset these states and alleviate risks should be conducted on a regular and sustainable basis. Thus, the improvements in the communication system across the departments, as well as the improvement in staff training schemes, are likely to significantly contribute to the reduction of similar sentinel events.
As it was mentioned above, the sentinel event took place largely due to the barriers that led to the breakdown in communication. Missing information at the time of transition of care became the leading factor that largely contributed to the sentinel event. Moreover, the lack of adequate training and education about maternal hypertension and pre-eclampsia states resulted in the poor care provided to the patient. A possible failure of the equipment in the OR may have been a cause why resuscitation measures failed. Moreover, the procedures of child delivery in patients from high risks groups are inadequate and should be revised.
To evaluate the success of the corrective action plan, a monitoring process at the hospital facilities should be established. The effectiveness of staff training programs should be assessed on the basis of tests or exams taken by the physician and nurses. To assess the effectiveness of the communication exchange, the monitoring process should include the analysis of the time it takes for the information to be transferred either in electronic or paper form and the number of clinical cases where there was a lack of information due to the disruption of communication processes. Staff should be encouraged to report on the lack of information issue, thus promoting the culture of exchange and openness within the organization. The allocation of budgetary resources should be channeled into personnel education and training as well as adequate staffing of hospital departments. These measures would allow significantly reduce the number of medical errors as well as adequately distribute responsibilities among the staff. The distribution of responsibilities would allow the staff to take proper care of every patient from the risk group so that no one is left with poor quality care or unattended. Moreover, the hospital must ensure the proper quality of medical equipment and supplies so that no errors occur due to equipment failures.
References
Balakrishnan, K., Brenner, M. J., Gosbee, J. W., & Schmalbach, C. E. (2019). Patient safety/quality improvement primer, part II: prevention of harm through root cause analysis and action (RCA2). Otolaryngology–Head and Neck Surgery, 161(6), 911-921.
Cox, M., & Sandberg, K. (2018). Modeling causal relationships in quality improvement. Current problems in pediatric and adolescent health care, 48(7), 182-185.
Patra, K. P., & De Jesus, O. (2021). Sentinel Event. StatPearls [Internet].
Parent, R., & Parent, C. (2021). Sentinel Event Reviews in the United States and Canada: Enhancing Service Delivery to the Community. In Enhancing Police Service Delivery (pp. 125-141). Springer, Cham. DOI: 10.1007/978-3-030-61452-2_9